Abstract
INTRODUCTION: As the U.S. population ages, primary care clinicians (PCCs) will encounter more patients with geriatric syndromes, such as urinary incontinence (UI) and falls. Yet, current evidence suggests that care of these conditions does not meet expected standards and that PCCs would benefit from tools to improve care of these conditions. Little is known about the role of computerized condition-specific templates for improving care of geriatric syndromes.
AIM: We sought to develop and assess the usefulness of condition-specific computerized templates in a primary care setting.
SETTING: A large academic Veterans Affairs medical center.
PROGRAM DESCRIPTION: We developed and tested the usefulness of 2 condition-specific computerized templates (UI and falls) that could be added on to an existing electronic health record system.
PROGRAM EVALUATION: Semistructured interviews were used to identify barriers to use of computerized templates. Usefulness and usability were assessed through a randomized-controlled trial involving standardized patients.
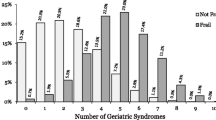
DISCUSSION: Use of condition-specific templates resulted in improved history and physical exam assessment for both UI and falls (P<.05). Our computerized, condition-specific templates are a promising method for improving care of geriatric conditions in a primary care setting, but require improvement in usability before widespread implementation.
Similar content being viewed by others
References
Campbell PA. State Population Projections. U.S. Census Bureau. 2005. Available at: http://www.census.gov/prod/2/pop/p25/p25-1131.pdf. Accessed March 16, 2006.
Wenger NS, Solomon DH, Roth CP, et al. The quality of medical care provided to vulnerable community-dwelling older patients. Ann Intern Med. 2003;139:740–7.
Bland DR, Dugan E, Cohen SJ, et al. The effects of implementation of the agency for health care policy and research urinary incontinence guidelines in primary care practices. J Am Geriatr Soc. 2003;51:979–84.
Chang JT, Morton SC, Rubenstein LZ, et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ. 2004;328:680.
Ostaszkiewicz J, Johnston L, Roe B. Habit retraining for the management of urinary incontinence in adults. Cochrane Database Syst Rev. 2004; (2):CD002801.
Wenger NS, Roth CP, Shekelle PG, et al. A controlled trial of a practice-based intervention to improve primary care for falls, incontinence, and dementia. J Gen Intern Med. 2005;20(suppl):52.
Reuben DB, Roth C, Kamberg C, Wenger NS. Restructuring primary care practices to manage geriatric syndromes: the ACOVE-2 intervention. J Am Geriatr Soc. 2003;51:1787–93.
Wrenn K, Rodewald L, Lumb E, Slovis C. The use of structured, complaint-specific patient encounter forms in the emergency department. Ann Emerg Med. 1993;22:805–12.
Mulvehill S, Schneider G, Cullen CM, Roaten S, Foster B, Porter A. Template-guided versus undirected written medical documentation: a prospective, randomized trial in a family medicine residency clinic. J Am Board Family Pract. 2005;18:464–9.
Flocke SA, Frank SH, Wenger DA. Addressing multiple problems in the family practice office visit. J Fam Pract. 2001;50:211–6.
Matsumura Y, Takeda H, Okada T, et al. Devices for structured data entry in electronic patient record. Medinfo. 1998;9(part 1):85–8.
Porter SC, Kohane IS. Optimal data entry by patients: effects of interface structure and design. Medinfo. 2001;10(part 1):141–5.
Gaul GM. Revamped Veterans’ Health Care Now a Model. Washington Post 2005 August 22: A01.
Department of Veterans Affairs. The Electronic Record: CPRS. Employee Orientation Toolkit. 2003. Available at: http://www.va.gov/oaa/orientation/admin_cprs.asp. Accessed May 17, 2004.
Weir CR, Hurdle JF, Felgar MA, Hoffman JM, Roth B, Nebeker JR. Direct text entry in electronic progress notes. An evaluation of input errors. Methods Inf Med. 2003;42:61–7.
Department of Veterans Affairs. U.S. Veteran Population (Includes Puerto Rico, Territories and Foreign Countries). Department of Veterans Affairs Veteran Data and Information Program Statistics. Available at: http://www.va.gov/vetdata/ProgramStatics/index.htm. Accessed March 16, 2006.
Rubenstein LV, Yano EM, Fink A, et al. Evaluation of the VA’s pilot program in institutional reorganization toward primary and ambulatory care: part I, changes in process and outcomes of care. Acad Med. 1996;71:772–83.
A New Generation of American Innovation Transforming Health Care: The President’s Health Information Technology Plan. The White House. 2005. Available at: http://www.whitehouse.gov/infocus/technology/economic_policy200404/chap3.html. Accessed March 16, 2006.
Freemantle N, Wood J, Crawford F. Evidence into practice, experimentation and quasi experimentation: are the methods up to the task? J Epidemiol Commun Health. 1998;52:75–81.
Campbell M, Fitzpatrick R, Haines A, et al. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000; 321:694–6.
Kushniruk AW, Patel VL. Cognitive and usability engineering methods for the evaluation of clinical information systems. J Biomed Inform. 2004;37:56–76.
Glassman PA, Luck J, O’Gara EM, Peabody JW. Using standardized patients to measure quality: evidence from the literature and a prospective study. Jt Comm J Qual Improv. 2000;26:644–53.
Shekelle PG, Mac Lean CH, Morton SC, Wenger NS. Assessing care of vulnerable elders: methods for developing quality indicators. Ann Intern Med. 2001;135(part 2):647–52.
Asch SM, Baker DW, Keesey JW, et al. Does the collaborative model improve care for chronic heart failure. Med Care. 2005;43:667–75.
Patterson ES, Nguyen AD, Halloran JP, Asch SM. Human factors barriers to the effective use of ten HIV clinical reminders. J Am Med Inform Assoc. 2004;11:50–9.
Saliba D, Elliott M, Rubenstein LZ, et al. The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community. J Am Geriatr Soc. 2001;49:1691–9.
Author information
Authors and Affiliations
Corresponding author
Additional information
She recognizes the support of members of the Older Americans Independence Center (OAIC) External Advisory Committee and Emmett Keeler, PhD.
Finally, Dr. Fung recognizes the time and effort of C. Alex Terry in the West Los Angeles CPRS Support Office, who helped program the computerized templates, and Colletta Austin, MA, in the CPRS Support Office, who set up the test server accounts for the project. The views expressed in this article are those of the author and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
Funding: This research study was supported by the UCLA Claude D. Pepper Older Americans Independence Center, NIH Grant P60 AG10415.
Commercial Associations: Dr. Fung is a staff member on a project funded by Pfizer and is a staff physician at the West Los Angeles VA Medical Center.
Rights and permissions
About this article
Cite this article
Fung, C.H. Computerized condition-specific templates for improving care of geriatric syndromes in a primary care setting. J GEN INTERN MED 21, 989–994 (2006). https://doi.org/10.1007/BF02743150
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02743150