Summary
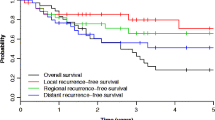
The present study examined the Liverpool database in an attempt to determine what proportion of N0 necks for various head and neck primary sites harbored subclinical squamous cell carcinoma and whether empiric treatment of occult disease improved survival over and above a “wait-and-watch policy” (treatment when metastasis becomes manifest). One hundred seventeen neck dissections were carried out for N0 necks, with 32% of specimens found to contain squamous cell carcinoma. The risk of carcinoma was highest in the hypopharynx, with 50% of specimens associated with a pyriform fossa primary cancer. Twenty-nine percent of neck dissection specimens for oral cavity cancer contained carcinoma and this was commonly associated with lateral border of tongue or anterior floor of mouth carcinomas. Twenty-five percent of specimens when primary tumor was in the oropharynx contained carcinoma and were due to tonsillar carcinoma. Twenty-one percent of laryngeal cancers produced histologically positive nodes and were mostly associated with posterior epiglottic tumors. Two hundred forty-six patients had a pyriform fossa cancer and of these only 37 had N0 disease and surgical treatment. Of these, 23 patients had radical neck dissections, whereas in 14 the necks were not treated. There was no difference in survival between the two groups (ξ1 2 = 0.787, P = NS). The Liverpool database also contained 1631 previously untreated patients with no clinical evidence of neck node metastases. Of these only 107 had a neck dissection. There was no difference in survival (ξ1 2 = 2.79, P = NS). When these data were analyzed by multivariate methods (Cox's proportional hazards model) prophylactic neck dissection was found to have no significant effect.
Similar content being viewed by others
References
Ari S, Tiwari RM, Snow GB (1985) False positive and false negative neck nodes. Head Neck Surg 8:78–82
Armitage P (1987) Statistical methods in medical research. Blackwell London
Bearhs OH, Henson DE, Hutter RVP, Myers MH (1988) American Joint Committee for Cancer Staging and End Result Reporting. Manual for staging of cancer, 3rd edn. Lippincott, Philadelphia
Cox DR (1972) Regression models and life tables. J R Stat Soc B34:187–220
Grandi C, Malloisio E, Moglia D, Podrecca S, Sala L, Salvatori P, Mollinari R (1985) Prognostic significance of lymphatic spread in head and neck carcinoma: therapeutic implications. Head Neck Surg 8:67–73
Hajek BC, Salomonwitz E, Turk R, Tscholakoff D, Kumpan W, Czembirek H (1986) Lymph nodes of the neck: evaluation with VS1. Radiology 158:739–742
Hermanek P, Sobin LH (1987) UICC. The TMN classification of malignant tumours, 4th edn. Springer, Berlin Heidelberg New York
Kalnins JK, Leonard AG, Soko K, Razack MS, Shed DP (1977) Correlation between prognosis and degree of lymph node involvement in carcinomas of the oral cavity. Ann J Surg 134:450–454
Ogura JH, Piller HF, Wette R (1971) Elective neck dissection for pharyngeal and laryngeal cancers: an evaluation. Ann Otol 80:646–651
Peto R, Pyke MC, Armitage P, Breslow NE, Cox DR, Howard SV, Mantel N, McPherson K, Peto J, Smith PH (1977) Design in analysis of randomised trials requiring prolonged observation of each patient. Br J Cancer 35:1–39
Sako K, Bradier RN, Marchettes FC, Bickren JW (1964) Fallibility of palpation in the diagnosis of metastases to cervical nodes. Surg Gynecol Obstet 118:989–990
Schuller DE, McGuirt WF, McCabe BF, Young D (1980) The prognostic significance of metastatic cervical lymph nodes. Laryngoscope 90:557–570
Snow GB, Annyas A, Vanslooten A, Bartelink H, Hart AAM (1982) Prognostic factors of neck node metastases. Clin Otolaryngol 7:185–192
Spiro RH, Strong EW (1973) Epidermoid carcinoma of the oral cavity and oropharynx. Arch Surg 107:382–384
Stell PM, Maran AGD (1978) Head and neck surgery. Heinemann, London
Stevens LP, Parkin JL (1985) Computed tomography of cervical lymph nodes. Staging and management of head and neck cancer. Arch Otolaryngol 111:735–739
Van den Brekel MWM, Castelijns JA, Croll GA, Stel HV, Valk J, Van der Waal I, Golding RP, Meyer CJLM, Snow GB (1991) Magnetic resonance imaging vs palpation of cervival lymph node metastases. Arch Otolaryngol Head Neck Surg 117:666–673
Van Den Brouck C, Sancho-Garnier H, Chassagne D, Saravene D, Cachin Y, Micheau C (1980) Elective versus therapeutic radical neck dissection in epidermoid carcinoma of the oral cavity. Cancer 46:386–390
Author information
Authors and Affiliations
Additional information
Based on a presentation at the International Symposium on the N0 neck: Göttingen, September 1992
Correspondence to A. S. Jones
Rights and permissions
About this article
Cite this article
Jones, A.S., Phillips, D.E., Helliwell, T.R. et al. Occult node metastases in head and neck squamous carcinoma. Eur Arch Otorhinolaryngol 250, 446–449 (1993). https://doi.org/10.1007/BF00181087
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00181087