Abstract
Background:
The most important complication of Kawasaki disease is coronary aneurysm (CA). The purpose of this study is to identify risk factors for coronary aneurysm in patients with Kawasaki disease treated at Sawanpracharak hospital during October 2006 to November 2011.
Methods:
Clinical, laboratory and treatment of patients diagnosed with Kawasaki disease were reviewed and categorized into two groups, CA (+) and CA (-) group. Clinical variables of interest were compared between the two groups and independent risk factors for coronary aneurysm were analyzed using a cluster logistic regression model.
Results:
A total of 67 patients were diagnosed with Kawasaki disease, of these,11 patients developed coronary aneurysm (16.4%). The CA (+) group had higher white blood cell counts, higher platelet counts, longer time from onset of disease to start of IVIG (IVIGd), lower hematocrit levels, and lower serum albumin. Cluster logistic regression was applied by dividing patients into 3 age groups, less than 12, 12-60months, and over 60 months. Risk factors for coronary aneurysm were: total neutrophil count > 12,000 / mm (OR = 15.46, 95%CI 5.56-43.00, p<0.001), erythrocyte sedimentation rate (ESR) >80 mm/ hr (OR = 5.00, 95%CI 2.60-9.64, p < 0.001), IVIGd > 8 days (OR 17.04, 95%CI 6.45-45.03, p < 0.001). Area under the curve (ROC) was 0.8807.
Conclusion:
Comparing patients with Kawasaki disease at the same age group, risk factors for coronary aneurysm were total neutrophil count > 12,000 / mm3, ESR > 80 mm/ hr and time from onset of disease to start of IVIG ≥ 8 days. When these risk factors are found in patients with Kawasaki disease, physicians should closely monitor these patients, give timely treatment, and consider early referral to a pediatric cardiologist.
Similar content being viewed by others
Introduction
Kawasaki disease is an acute self limited vasculitis of childhood, characterized by fever, bilateral non-exudative conjunctivitis, erythema of the lips and oral mucosa, changes in the extremities, rash, and cervical lymphadenopathy. The disease was first described in Japan in 1967 by Tomisaku Kawasaki (1) and was first reported in Thailand in 1982 (2). While the etiology remains unknown, evidence supports an infection-triggered immune response in genetically susceptible individuals leading to systemic vasculitis, including coronary arteritis. Because of the obscure etiology, no prevention or control measures are available other than close monitoring and timely treatment.
Kawasaki disease is now the leading cause of acquired heart disease in children (3). The most important complication is coronary aneurysm (CA) which develops in 15-25% of untreated children (4) and may lead to myocardial infarction or sudden death. Treatment with intravenous immunoglobulin (IVIG) can reduce coronary complications (5) and is recommended as a standard treatment.
Several studies report risk factors of coronary artery abnormalities in patients with Kawasaki disease such as extreme age, male sex, incomplete Kawasaki disease, abnormal laboratory data (including C-reactive protein, erythrocyte sedimentation rate, hemoglobin concentration, platelets counts, and neutrophil counts), delayed treatment and IVIG nonresponsiveness (3, 6-12). Risk factors were used to identify patients that may benefit from IVIG treatment. However, there are no universal agreement in these parameters or cut-off points, and no perfect scoring system for clinical recommendation. American Heart Association guideline 2004 recommends to giving IVIG to all acute phase Kawasaki patients, preferably within 10 days of illness (1). However, risk factors can be useful tools in tailoring individual care, especially for pediatricians in provincial hospitals without a pediatric cardiologist. Risk factors studies may also be different in various populations. The purpose of this study is to determine risk factors for coronary aneurysm in patients with Kawasaki disease treated at Sawanpracharak hospital, Nakomsawan, Thailand during October 2006 to November 2011.
Methods
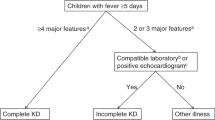
Patients. This study was approved by the Ethic committee of Sawanpracharak Hospital. A retrospective cohort study was conducted and medical records of 76 Kawasaki disease patients admitted at Sawanpracharak hospital, during October 2006 to November 2011 were reviewed. For incomplete Kawasaki disease, diagnosis was made base on the 2004 revised American Heart Association recommendation (1). Inclusion criteria included both complete and incomplete Kawasaki disease patients who were treated with 2 g/Kg of IVIG. Exclusion criteria were: inconclusive diagnosis or later diagnosis of other diseases known to mimic Kawasaki disease, and those patients who underwent less than 2 echocardiograms. For recurrent Kawasaki disease, the duration between two admissions must be longer than 2 weeks. IVIG nonresponsive was defined as continuation of fever more than 2 days after IVIG administration and were re-treated with IVIG 1-2 g/Kg.
Echocardiography. Two dimensional echocardiography was done at acute phase and 4-6 weeks later. Definition of coronary artery abnormalities (CAA) were based on the Japanese Ministry of Health and Welfare criteria (13) or a maximal z score of internal diameter of proximal right coronary artery, proximal left anterior descending coronary artery or left main coronary artery > 2.5 (14). Definition of coronary aneurysm (CA) was CAA with anatomical bulging (internal diameter of a segment at least 1.5 times as large as that of an adjacent segment).
Statistics. Variables that were tested as risk factors for coronary aneurysm were age, sex, selected clinical manifestations, selected laboratory findings, and time from onset of disease to start of IVIG (IVIGd). In case of multiple laboratory data, data acquired closest to the time of diagnosis were used.
Patients were categorized into 2 groups, CA (+) and CA (-) group and variables with selected cut-off points were compared using statistical program Stata 10.1 (StataCorp, Inc, College Station, Tx, U.S.A.). Nominal data and continuous data were compared by using Fisher’s exact test or unpaired t-test, respectively. Odds ratio and 95% confident interval were calculated. Data showing a significant difference or risk were stepwise tested by using cluster logistic regression. Data were expressed as mean± standard deviation or percentages. A p value of < 0.05 was considered to be statistically significant.
Results
There were 76 Kawasaki disease patients admitted at Sawanpracharak hospital during October 2006 to November 2011 but 9 patients was excluded due to inconclusive diagnosis (2 patients), inadequate echocardiogram (1 patient), no IVIG treatment (5 patients) and later diagnosis as polyarteritis nodosa (1 patients). Of the 67 patients, 49 (73.1%) were complete Kawasaki disease and 18 (26.9%) were incomplete Kawasaki disease. In this study, one patient (1.5%) had recurrent Kawasaki disease and 7 patients (10.5%) were diagnosed as IVIG nonresponsiveness.
Echocardiographic evidence of CAA was detected in 20 patients (29.9%) and 11 patients (16.4%) developed CA. Giant aneurysms were noted in 3 patients (4.5%).
The CA (+) group had higher white blood cell count (22.4 ± 1.5 vs 17.0 ± 0.9 K/mm3, p = 0.016), higher platelets count (635.5 ± 82.1 vs 375.5 ± 18.6 K/mm3, p < 0.001) and longer time from onset of disease to start of IVIG (IVIGd) (10.3 ± 0.9 vs 7.1 ± 0.3 days p < 0.001), lower hematocrit (28.6 ± 1.3 vs 31.1 ± 0.5 %, p = 0.040) and lower serum albumin (3.1 ± 0.2 vs 3.5 ± 0.1 g/dl, p = 0.030) (table 1). Using selected cut-off points for each variables, the percentage of abnormal value of the two groups were compared and shown in table 2.
Risk factors for coronary aneurysm as single variable analysis were total neutrophil count > 12,000/mm3 (OR = 8.10, 95%CI 1.43-81.61,p = 0.006), hematocrit < 28 % (OR = 6.00, 95%CI 1.10-27.52, p = 0.017), platelets count > 450,000/ mm3 (OR = 9.14, 95%CI 1.79-49.90, p = 0.002), serum albumin < 3 g/dl (OR 4.44, 95%CI 1.12-17.6, p = 0.032), IVIGd > 8 days (OR 5.63, 95%CI 1.14-35.84, p = 0.015) (table 3).
Using cluster logistic regression by divided patients into 3 groups, age < 12 , 12-60, >60 months, independent risk factors for coronary aneurysm were total neutrophil count > 12,000 / mm3 (OR = 15.46, 95%CI 5.5643.00, p<0.001), erythrocyte sedimentation rate (ESR) >80 mm/ hr (OR = 5.00, 95%CI 2.60-9.64, p < 0.001), IVIGd > 8 days (OR 17.04, 95%CI 6.45-45.03, p < 0.001). Area under the curve (ROC) = 0.8807 (table 4).
Discussion
Various demographic and clinical risk factors have been previously reported to be associated with coronary involvement in Kawasaki disease. In this study, male sex, extreme age (age < 1 year or > 5 years) and incomplete Kawasaki disease could not be demonstrated as risk factors for coronary aneurysm. The reasons could be from variation in the population. Another possibility is our small sample size was unable to demonstrate the effects of these parameters (beta error). Confounding factors such as relationship between variables could also be problematic. Kawasaki disease patients with age < 1 year often had incomplete criteria, making diagnosis difficult. In the over 5 years age group Kawasaki disease is generally rare, thus resulting in delayed diagnosis. These factors may have contributed in later diagnosis and longer time from onset of disease to start of IVIG (IVIGd). Because a previous study demonstrated that age was a risk factor for CAA (8). We decided to use age as a control variable in risk factor analysis by using cluster logistic regression.
There has been a great attempt to focus on laboratory factors and cut-off points in making algorithm for clinical decision in the diagnosis and treatment of Kawasaki disease. Laboratory data were clearly defined in the 2004 revised American Heart Association recommendations to help clinicians evaluate children with suspected incomplete Kawasaki disease (1). Laboratory data were inconsistent in previous risk factor studies (9-11) but there was a propensity for some factors in detail. Total neutrophil count > 12,000 / mm3, ESR > 80 mm/ hr and time from onset of disease to start of IVIG > 8 days were risk factors of coronary aneurysm in this study.
Duration of fever, presumably reflecting prolonged and ongoing vasculitis, has been confirmed as a powerful predictor of CAA (11). Time from onset of disease to start of IVIG (IVIGd) is slightly shorter than total duration of fever except for IVIG nonresponsive cases. We used IVIGd in this study because it discarded the problem of IVIG nonresponsive cases and was considered to be more practical. In this study, IVIGd > 8 days was the most outstanding risk factor of coronary aneurysm.
Leukocytosis is typical during acute stage of Kawasaki disease with preponderance of immature and mature granulocytes. Total neutrophil count was composed of two factors, leukocyte count and percentage of neutrophil. The latter were commonly used in risk factor studies but only several studies used total neutrophil count. Beiser et al used baseline neutrophil and band counts as risk factors (15). Our study also supported the use of total neutrophil count as an important risk factor for coronary aneurysm.
ESR, representing acute phase reactant, is frequently used as a risk factor although it had smaller effects comparing to IVIGd and total neutrophil count in predicting CAA. In single variable analysis, ESR > 80 mm/hr was considered insignificant risk factor but its propensity for prediction could not be overlooked. Thus ESR was chosen for analysis in cluster logistic regression which unsurprisingly showed its significance.
The incidence of coronary artery abnormality, coronary aneurysm and giant aneurysm were higher than expected in our study. McCrindle et al reported coronary artery abnormality 23% by using Japanese Ministry of Health and Welfare criteria (15) and 26% by using z score > 2.5 (14). Our study used both criteria which may have increased the incidence. Other possible explanations of high incidence of coronary aneurysm (16.4%) could be from different study population and the technical term difference in discrimination between small aneurysm (especially diameter less than 4 mm) and coronary dilation. Delayed IVIG therapy could also be the explanation of our high incidence of coronary aneurysm and was mainly from delayed diagnosis. Our hospital is a tertiary care center receiving patients referred from other hospitals, which may have contributed to the delay in diagnosis. Limitations of the study is the small sample size performed in a single center, therefore our findings may not be generalizable to other populations. The enrollment of incomplete Kawasaki disease patient also raises suspicions in the diagnosis.
The results of this study allowed clinician taking care of Kawasaki disease patients to plan for further management. The use of no IVIG therapy in patients without risk factors could hardly be recommended since all risk factors algorithm are not perfect and there remains potential concerns about long-term abnormal coronary artery function even in patients whose coronary artery involvement was never detected(1). Knowledge in Kawasaki disease and the importance of proper and prompt IVIG therapy should be emphasized to health care providers in the community. Further study in risk scoring for coronary aneurysm and for prediction of IVIG nonresponsiveness could be beneficial (16-17). The evidences from our study also supported that prolonged and severe inflammation were associated with coronary aneurysm formation (11)
Conclusion
Compared to patients with Kawasaki disease at the same age group, risk factors for coronary aneurysm were total neutrophil count > 12,000 / mm3, ESR > 80 mm/ hr and time from onset of disease to start of IVIG > 8 days. Physicians who take care of patients diagnosed with Kawasaki disease with these risk factors should carefully monitor the patients, give timely and proper additional therapies if fever continues after IVIG treatment and consider early referral to a pediatric cardiologist.
Acknowledgements
The authors wish to thank Associate Professor Patumanond Jayanton for statistical analysis of this study and Professor Apichai Khongphatthanayothin and Dr. Monvasi Pachinburavan for their precious advice and proof-reading of the manuscript.
References
Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the committee on rheumatic fever, endocarditis and Kawasaki disease, Council on cardiovascular disease in the young, American Heart Association. Circulation 2004;110:2747-71.
Thisyakorn C, Thisyakorn U. Kawasaki disease in Thai children. Pediatr Infect Dis J 1995; 14: 324-6.
Newburger JW, Fulton DR. Kawasaki disease. Curr Opin Pediatr 2004;16:508-14.
Kato H, Sugimura T, Akagi T, Sato N, Hashino K, Maeno Y, et al. Longterm consequences of kawasaki disease. A 10 to 21- year follow-up study of 594 patients. Circulation 1996;94:1379-85.
Durongpisitkul K, Gururaj VJ, Park JM, Martin CF. The prevention of coronary aneurysm in Kawasaki disease: a metaanalysis on the efficacy of aspirin and immunoglobulin treatment. Pediatrics. 1995;96:1057-61.
Manlhiot C, Yeung RSM, Clarizia NA, Chahal N, McCrindle BW. Kawasaki disease at the extremes of the age spectrum. Pediatrics 2009; 124;e410
Muta H, Ishii M, Sakaue T, Ekami K, Furui J, Sugahara Y, et al. Older age is a risk factor for the development of cardiovascular sequelae in Kawasaki disease. Pediatrics 2004;114;751
Song D, Yeo YK, Ha KS, Jang GY, Lee JH, Lee KC, et al. Risk factors for Kawasaki disease-associated coronary abnormalities differ depending on age. Eur J Pediatr 2009; 168:1315-21
Kim JJ, Hong YM, Yun SW, Han MK, Lee KY, Song MS, et al. Assessment of risk factors for Korean children with Kawasaki disease. Pediatr Cardiol; published online:22 November 2011
Hongkanen VEA, McCrindle BW, Laxer RM, Feldman BM, Schneider R, Silverman ED. Clinical relevance of the risk factors for coronary artery inflammation in Kawasaki disease. Pediatr Cardiol 2003;24:122-6
Kim TY, Choi WS, Woo CW, Choi BM, Lee JH, Lee KC, et al. Predictive risk factors for coronary artery abnormalities in Kawasaki disease. Eur J Pediatr 2007;166:421-5
Nakamura Y, Yashiro M, Sadakane A, Aoyama Y, Oki I, Uehara R, et al. Six principal symptoms and coronary sequelae in Kawasaki disease. Pediatrics International 2009:51:705-8.
Research Committee on Kawasaki disease. Report of subcommittee on standardization of diagnostic criteria and reporting of coronary artery lesions in Kawasaki disease. Tokyo, Japan: Japanese Ministry of Health and welfare;1984
McCrindle BW, Li JS, Minich LL, Colan SD, Atz AM, Takahashi M, et al. Coronary artery involvement in children with Kawaski disease Risk factors from analysis of serial normalized measurements. Circulation 2007;116:174-9.
Beiser AS, Takahashi M, Baker AL, Sundel RP, Newburger JW. A predictive instrument for coronary artery aneurysms in Kawasaki disease. Am J Cardiol 1998;81:116-20.
Uehara R, Belay ED, Maddox RA, Holman RC, Nakamura Y, Yashiro M, et al. Analysis of potential risk factors associated with nonresponse to initial intravenous immunoglobulin treatment among Kawasaki disease patient in Japan. Pediatr Infect Dis J 2008;27:155-60.
Kobayashi T, Inoue Y, Takeuchi K, Okada Y, Tamura K, Tomomasa T, et al. Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease. Circulation 2006; 113:2606-12.
Author information
Authors and Affiliations
Corresponding author
Additional information
Correspondence to Pentip Supachokchaiwattana, MD, Department of Pediatrics. Sawanpracharak Hospital. Nakhonsawan. Thailand. Telephone: (+665) 621 9888. Fax: (+665) 621 9899. E-mail: pentip_s@yahoo.com. Open Access: This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Supachokchaiwattana, P., Vibulwatanakij, S. Risk Factors for Coronary Aneurysm in Kawasaki Disease in Central Thailand. Asean Heart J 22, 1 (2014). https://doi.org/10.7603/s40602-014-0001-5
Published:
DOI: https://doi.org/10.7603/s40602-014-0001-5