Abstract
Background
Laparoscopic liver resection (LLR) is increasingly utilized for patients with hepatocellular carcinoma (HCC). However, long-term outcomes for patients requiring conversion to an open procedure during LLR have not been examined.
Methods
Patients undergoing attempted LLR for HCC were identified within the National Cancer Database. Patients undergoing successful LLR were compared with those who required unplanned conversion with regard to perioperative outcomes and overall survival (OS). Those experiencing conversion were further compared with patients who underwent planned open resection after propensity score matching.
Results
Unplanned conversion occurred in 228 (18.0%) of 1270 patients undergoing LLR. Compared with successful LLR, conversion was associated with greater length of stay (6 vs. 4 days, p < 0.001), higher readmission rates (7.8% vs. 2.6%, p = 0.001), and reduced OS (55.1 vs. 67.6 months, p = 0.074). Unplanned conversion during major hepatectomy was associated with significantly worse OS (median 35.7 months) compared with successful major and minor LLR (median not reached and 67.6 months, respectively, p = 0.004). Compared with planned open resection, similar results were noted as conversion during major LLR was associated with worse OS (median 27.3 months) compared with open major hepatectomy (median not reached; p = 0.002). Unplanned conversion was independently associated with increased mortality (hazard ratio 1.38) after adjustment in a multivariable model. Tumor size was the strongest predictor of conversion on logistic regression analysis.
Conclusions
Unplanned conversion during LLR for HCC is associated with inferior OS. This difference is most pronounced for major hepatectomy. LLR should be considered cautiously in patients with larger, more advanced tumors likely to require major resection.
Similar content being viewed by others
Laparoscopic liver resection (LLR) is considered an oncologically safe and acceptable approach for hepatocellular carcinoma (HCC).1,2,3,4,5,6 In turn, the utilization of LLR has increased significantly over the past two decades.7,8 As experience with LLR has grown, so has the extent and complexity of hepatic resections.8,9,10
Short-term outcomes for patients undergoing successful LLR have been shown to be equivalent or superior to traditional open resection.11 However, greater rates of morbidity and perioperative mortality for patients requiring an unplanned conversion to an open procedure during LLR have been reported.12,13,14,15 To date, the impact of unplanned conversion on long-term survival for patients with HCC has not been evaluated.
The current study examined the factors associated with unplanned conversion to better identify patients at risk of unsuccessful LLR. In addition, the long-term survival for patients requiring unplanned conversion is examined and compared with successful LLR and planned open resection. It is hypothesized that conversion during LLR is associated with worse overall survival (OS), exclusive of perioperative mortality, and there are identifiable factors that may predict patients at greater risk for unsuccessful LLR.
Methods
Data Source and Patient Selection
The National Cancer Data Base (NCDB) is a hospital-based clinical oncology dataset estimated to include 70% of the nation’s annual malignant diagnoses. Cases are identified via the third edition of the International Classification of Disease for Oncology (ICD-O-3) histologic codes. As the NCDB contains appropriately de-identified patient data, this study was deemed exempt by the University of Tennessee Health Science Center institutional review board.
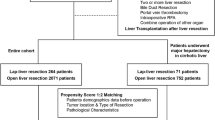
Patients with ICD-O-3 histologic codes corresponding to a diagnosis of HCC were selected from the 2000–2014 NCDB dataset. Because the NCDB has only more recently included information regarding unplanned conversion, only those cases from 2010 to 2014 were able to be analyzed. Surgical cases were subdivided by operative approach: those undergoing successful LLR and those experiencing unplanned conversion to an open procedure during attempted LLR. Patients undergoing total hepatectomy (i.e., transplant), nonresectional local interventions alone (i.e., ablation), combined HCC-cholangiocarcinoma, and those with metastatic disease were excluded (see Supplemental Fig. 1 for selection flow diagram).
Factors Associated with Unplanned Conversion
Patients undergoing successful LLR were contrasted with those experiencing conversion with regard to baseline patient- and tumor-specific characteristics, including demographics, comorbidities, facility type, and case-volume, as well as tumor size, stage, and grade. Additionally, the extent of resection (minor or major hepatectomy) was compared between groups. The extent of resection was determined via surgical procedure codes with lobectomy and extended lobectomy codes defined as major hepatectomies and segmental resections classified as minor hepatectomies.16 Factors approaching significance on univariate comparison were included in a multivariable analysis to determine their independent association with conversion.
Short- and Long-term Outcomes
Patients with missing follow-up or survival data were excluded from subsequent outcomes analysis (n = 326; Supplemental Fig. 1), with an equal proportion of patients excluded from each group. Resection margins, 30- and 90-day mortality, length of stay (LOS), and readmission were assessed. OS, defined as the time from diagnosis to death or censoring, was evaluated for both groups and was further substratified based on extent of resection (major vs. minor hepatectomy). Multiple factors potentially associated with OS, including unplanned conversion, were evaluated within a Cox proportional hazards model to determine their independent effect on survival.
Comparison to Open Liver Resection
Using similar selection criteria, patients experiencing unplanned conversion were compared with those undergoing planned open resection following propensity score matching to account for likely differences. Propensity scores were estimated based on a logistic regression model accounting for key covariates, including age, gender, race, comorbidities (Charlson–Deyo Comorbidity Index), extent of resection (major vs. minor hepatectomy), and tumor characteristics, such as primary tumor (T) classification, grade, and the presence of lymphovascular invasion. 1:1 matching between groups was performed based on generated propensity scores. Analysis of indicated covariates was performed pre- and post-matching to ensure adequate balance. Groups were then compared with regard to short- and long-term outcomes.
Data Analysis
Continuous variables were expressed using the median and interquartile range (IQR) and analyzed with the Wilcoxon rank-sum test. Categorical variables were stated as counts with relative frequencies and compared using the Chi-square test or Fisher’s exact test when appropriate. Univariate survival comparison was performed with Kaplan–Meier curves and the log-rank test. A p value < 0.15 was used to select variables for initial inclusion in multivariable models. Logistic regression model fit was assessed with the Hosmer–Lemeshow goodness-of-fit test. All statistical analysis was performed with SAS version 9.4 (SAS Institute, Cary, NC).
Results
A total of 1270 patients with HCC underwent attempted LLR over the 5-year period. Patients were predominantly male (71.2%) and Caucasian (68.8%), with a median age of 65 (IQR 58–72). Most were treated at an academic facility (68.0%). Overall median tumor size for patients undergoing attempted LLR was 3.9 (IQR 2.5–6.3) cm, and most were T1 (57.6%) or T2 (28.8%) tumors. Overall, 349 (27.5%) patients underwent attempted major hepatectomy via a laparoscopic approach.
The number of attempted LLR per year increased from 188 in 2010 to 320 in 2014. Unplanned conversion occurred in 228 cases (18.0%). There was no significant difference in conversion rates between years (range 16.2–20.2%, p = 0.796), nor was there a discernable trend in conversion rates over time (Supplemental Fig. 2).
Examination of Patient-Specific Variables
Comparison of patient- and tumor-specific variables for successful LLR and unplanned conversion are detailed in Table 1a. There was no significant difference between the groups with regard to age, gender, race, or comorbid status. The median number of attempted LLR was similar between facilities in either group (8.0 cases/5 years vs. 7.5 cases/5 years, p = 0.109). Patients experiencing conversion had larger tumors (median 5.0 vs. 3.7 cm, p < 0.001) and a greater percentage of T3/T4 tumors (21.1% vs. 11.6%, p = 0.002) compared with those undergoing successful LLR. The presence of lymphovascular invasion was associated with unplanned conversion (32.9% vs. 23.2%, p = 0.006).
For both groups, most resections were minor hepatectomies. However, the rate of unplanned conversion was greater for those undergoing major hepatectomy (38.2% vs. 25.1%, p < 0.001). On examination of cases of attempted major LLR, 30.2% of those undergoing right/extended right hepatectomy experienced unplanned conversion compared with only 19.9% of those undergoing left/extended left hepatectomy (p = 0.042) (note: in 49 of 349 major hepatectomies, the laterality was not indicated).
Results of a multivariable analysis of those characteristics approaching significance on univariate comparison are shown in Table 1b. Tumor size was the only factor found to be independently associated with the occurrence of unplanned conversion (odds ratio [OR] 1.07, 95% confidence interval [CI] 1.02–1.12), even after adjusting for multiple other factors.
Outcomes Following Unplanned Conversion
Median follow-up times for the unplanned conversion and successful LLR groups were 24.3 and 26.3 months, respectively. Patients who underwent unplanned conversion had a higher percentage of positive margins compared with the LLR group (11.6% vs. 7.5%), although this was not statistically significant (p = 0.086; Table 2). Median LOS was 2 days longer (6 days vs. 4 days, p < 0.001) and 30-day readmission rates were three times higher (7.8% vs. 2.6%, p = 0.001) among patients who required conversion compared with those who underwent successful LLR. Short-term mortality was not significantly different between the groups.
On initial analysis, patients who experienced unplanned conversion had significantly lower OS compared with those who underwent successful LLR (median OS: 54.7 vs. 67.6 months, p = 0.0154; figure not shown). However, this difference was no longer significant when patients with 90-day mortality were excluded (median OS: 67.6 months [LLR] vs. 55.1 months [conversion], p = 0.074; Fig. 1a). Upon further sub-stratification based on the extent of resection (Fig. 1b), it was noted that patients who experienced unplanned conversion while undergoing major hepatectomy had a significantly lower estimated probability of survival (median OS 35.7 months) compared with those who experienced conversion during minor hepatectomy (median OS not reached) as well as those who underwent successful laparoscopic minor (median 67.6 months) and major hepatectomy (median not reached; p = 0.004).
On multivariable Cox regression analysis (Table 3), multiple factors were found to be independently associated with survival, including patient comorbidities (hazard ratio [HR] 1.77, 95% CI 1.34–2.34), tumor grade (HR 1.50, 95% CI 1.13–2.00), and advanced tumor stage (HR 1.89, 95% CI 1.32–2.71). Tumor size also was significantly associated with OS and appeared to be incremental in effect as the hazard of death increased with the dimensions of the tumor: a tumor 2–5 cm in size was associated with a hazard of death 1.6 times that of a tumor < 2 cm (p = 0.052) and increased to a hazard nearly 2 times baseline for tumors ≥ 5 cm (p = 0.011). The occurrence of unplanned conversion remained significantly associated with mortality in the model even after adjusting for other patient and tumor characteristics (HR 1.38, 95% CI 1.03–1.86).
Comparison to Open Resection
Following propensity matching, patients who underwent conversion were compared with 167 well-matched patients who underwent planned open hepatectomy. Median follow-up times for the matched unplanned conversion and open resection groups were 24.3 and 29.6 months, respectively. Groups were similar with regard to rates of positive margins (11.4% vs. 9.0%, p = 0.492) and readmission (7.8% vs. 7.2%, p = 0.835). Patients who required unplanned conversion had a nonsignificant trend toward greater LOS compared with those who underwent planned open resection (median 6 vs. 5 days, p = 0.053). There was no difference in the occurrence of 90-day mortality (10.2% vs. 8.4%, p = 0.572).
After excluding cases involving 90-day mortality, median OS was similar for those experiencing conversion and those undergoing open resection (54.7 vs. 57.5 months, p = 0.179). However, a significant difference was again found upon stratification based on the extent of resection (Fig. 2). Patients who underwent conversion during major hepatic resection had a significantly reduced OS (median 27.3 months) compared with those who experienced conversion during minor resection (55.1 months), along with those who underwent open minor (57.5 months) and major hepatectomy (median OS not reached) (p = 0.002).
Discussion
This is the first report to examine the long-term survival for patients who experienced unanticipated conversion to an open procedure during LLR. Not only do the results in this analysis coincide with previously published studies of the short-term outcomes associated with unplanned conversion, they also suggest that conversion is associated with reduced OS beyond the early postoperative period.13 These differences in survival were most pronounced for patients undergoing major hepatectomy and remained significant after multivariable adjustment.
Contemporary multi-institutional series of LLR have described 5-year overall and recurrence-free survival rates of 73% and 50%, respectively, paralleling those of open resection.5,8 In a recent meta-analysis examining 917 patients (334 with HCC) undergoing either laparoscopic or open major hepatectomy, Kasai et al.11 found that a laparoscopic approach was associated with a lower rate of postoperative morbidity and a reduced LOS. For patients with HCC, there was no difference in OS between the laparoscopic and open major hepatectomy groups. While the results for successful LLR in the current analysis agree with these previous reports, the long-term implications for those patients undergoing conversion should be noted. Despite adjustment for multiple other significant prognostic factors, conversion remained independently associated with an increased hazard of death on multivariable analysis in this study. Furthermore, although survival rates were similar for patients undergoing successful laparoscopic and planned open major resection, unplanned conversion during major LLR was associated with significantly worse survival exclusive of 90-day mortality (Figs. 1b, 2).
While multiple factors, including T classification, histologic grade, lymphovascular invasion, and the extent of resection correlated with conversion on a univariate level, only tumor size remained independently associated with unplanned conversion on multivariable analysis. The OR of 1.07 obtained from the logistic regression analysis indicates that the odds of conversion increase by 7% for each centimeter of increased tumor size. This association with tumor size may explain why major hepatectomy remains associated with conversion in many published series.12,13,14,17 On retrospective analysis of 223 patients undergoing major LLR, Cauchy et al. found tumor diameter > 10 cm to be strongly associated with conversion (HR 8.91, p = 0.014) on multivariable analysis.14 In a recent review of 2861 LLR performed at seven tertiary referral centers across Europe, Halls et al.17 determined that lesion size (OR 1.4, p = 0.001) and the extent of resection (OR 1.2, p = 0.003) were both independently associated with conversion. In addition, the authors noted that patients who experienced emergent conversion due to an adverse intraoperative event (i.e., bleeding) experienced inferior perioperative outcomes compared with those who underwent conversion for an unanticipated finding (i.e., dense adhesions, inability to progress, etc.). This suggests that early and prompt conversion, when appropriate, is in the patient’s best interest and should not be viewed as failure.18
Notable results also were observed when unplanned conversion was compared with planned open resection. Short-term outcomes, including LOS, readmissions, and early mortality rates, were, at best, equivalent between groups. This mirrors a previous examination of the NSQIP database, in which similar rates of morbidity and mortality were found in patients undergoing conversion compared with a cohort of propensity-matched open cases.13 Interestingly, conversion during major hepatectomy resulted in significantly decreased long-term survival in the current analysis. This would indicate that the stakes are much higher for major hepatectomy and conversion should not be viewed as a trivial occurrence in this group. In contrast, OS was not negatively impacted when conversion occurred during minor LLR compared to successful LLR and planned open resections. Therefore, when minor resection can be assured preoperatively, as in small isolated lesions, LLR may be approached with more confidence as these results suggest that conversion does not necessarily guarantee a poor long-term result.
There are certain restrictions to the current analysis, mostly related to inherent limitations of the NCDB. Due to large amounts of missing data for certain liver-specific variables, such as the hepatic fibrosis score, the degree of underlying cirrhosis or other parenchymal alterations were unable to be accounted for. Similarly, this analysis could not account for the presence of liver disease or the underlying cause if cirrhosis was present. Secondly, the database does not contain information regarding the exact cause of conversion, only its occurrence. Thus, the true incentives for conversion in these cases was not determined. While attempts were made to adjust for the volume of procedures performed at individual facilities, it was not possible to adjust for the experience of individual surgeons. Because a learning curve exists for minimally invasive hepatobiliary procedures, the omission of this covariate likely introduces a degree of bias into these results.9,19,20,21 Finally, because the current analysis is limited to patients with HCC, it cannot be fully extrapolated to patients with other primary hepatic or metastatic lesions.
Conclusions
Within this national oncology dataset, tumor size was the most significant predictor of conversion during attempted LLR for HCC. Patients undergoing unplanned conversion to an open procedure during LLR experienced inferior short-term outcomes and reduced OS compared with those undergoing successful LLR, especially in those cases involving major hepatic resection. Compared with open liver resection, unplanned conversion was again associated with inferior survival for those undergoing major hepatectomy. Major hepatic resection via a laparoscopic approach should be reserved for cases with a high likelihood of success and should be approached cautiously in patients with large tumors.
References
Belli G, Limongelli P, Fantini C, et al. Laparoscopic and open treatment of hepatocellular carcinoma in patients with cirrhosis. Br J Surg. 2009;96(9):1041–8. https://doi.org/10.1002/bjs.6680.
Dagher I, Belli G, Fantini C, et al. Laparoscopic hepatectomy for hepatocellular carcinoma: a European experience. J Am Coll Surg. 2010;211(1):16–23. https://doi.org/10.1016/j.jamcollsurg.2010.03.012.
Tranchart H, Di Giuro G, Lainas P, et al. Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc. 2010;24(5):1170–6. https://doi.org/10.1007/s00464-009-0745-3.
Cherqui D, Laurent A, Tayar C, et al. Laparoscopic liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease. Ann Surg. 2006;243(4):499–506. https://doi.org/10.1097/01.sla.0000206017.29651.99.
Fancellu A, Rosman AS, Sanna V, et al. Meta-analysis of trials comparing minimally-invasive and open liver resections for hepatocellular carcinoma. J Surg Res. 2011;171(1):e33–45. https://doi.org/10.1016/j.jss.2011.07.008.
Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015;261(4):619–29. https://doi.org/10.1097/sla.0000000000001184.
Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection—2,804 patients. Ann Surg. 2009;250(5):831–41. https://doi.org/10.1097/sla.0b013e3181b0c4df.
Berardi G, Van Cleven S, Fretland ÅA, et al. Evolution of laparoscopic liver surgery from innovation to implementation to mastery: perioperative and oncologic outcomes of 2,238 patients from 4 European Specialized Centers. J Am Coll Surg. 2017;225(5):639–49. https://doi.org/10.1016/j.jamcollsurg.2017.08.006.
Dagher I, OʼRourke N, Geller DA, et al. Laparoscopic major hepatectomy. Ann Surg. 2009;250(5):856–60. https://doi.org/10.1097/sla.0b013e3181bcaf46.
Dagher I, Gayet B, Tzanis D, et al. International experience for laparoscopic major liver resection. J Hepatobiliary Pancreat Sci. 2014;21(10):732–6. https://doi.org/10.1002/jhbp.140.
Kasai M, Cipriani F, Gayet B, et al. Laparoscopic versus open major hepatectomy: a systematic review and meta-analysis of individual patient data. Surgery. 2018;163(5):985–95. https://doi.org/10.1016/j.surg.2018.01.020.
Troisi RI, Montalti R, Van Limmen JGM, et al. Risk factors and management of conversions to an open approach in laparoscopic liver resection: analysis of 265 consecutive cases. HPB. 2014;16(1):75–82. https://doi.org/10.1111/hpb.12077.
Stiles ZE, Behrman SW, Glazer ES, et al. Predictors and implications of unplanned conversion during minimally invasive hepatectomy: an analysis of the ACS-NSQIP database. HPB. 2017;19(11):957–65. https://doi.org/10.1016/j.hpb.2017.06.012.
Cauchy F, Fuks D, Nomi T, et al. Risk factors and consequences of conversion in laparoscopic major liver resection. Br J Surg. 2015;102(7):785–95. https://doi.org/10.1002/bjs.9806.
Goh BKP, Chan C-Y, Wong J-S, et al. Factors associated with and outcomes of open conversion after laparoscopic minor hepatectomy: initial experience at a single institution. Surg Endosc. 2015;29(9):2636–42. https://doi.org/10.1007/s00464-014-3981-0.
Strasberg SM. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg. 2005;12(5):351–5. https://doi.org/10.1007/s00534-005-0999-7.
Halls MC, Cipriani F, Berardi G, et al. Conversion for unfavorable intraoperative events results in significantly worst outcomes during laparoscopic liver resection. Ann Surg. 2017. https://doi.org/10.1097/sla.0000000000002332.
Buell JF, Cherqui D, Geller D, et al. The international position on laparoscopic liver surgery. Ann Surg. 2009;250(5):825–30. https://doi.org/10.1097/sla.0b013e3181b3b2d8.
Komatsu S, Scatton O, Goumard C, et al. Development process and technical aspects of laparoscopic hepatectomy: learning curve based on 15 years of experience. J Am Coll Surg. 2017. https://doi.org/10.1016/j.jamcollsurg.2016.12.037.
van der Poel MJ, Besselink MG, Cipriani F, et al. Outcome and learning curve in 159 consecutive patients undergoing total laparoscopic hemihepatectomy. JAMA Surg. 2016;151(10):923. https://doi.org/10.1001/jamasurg.2016.1655.
Nomi T, Fuks D, Kawaguchi Y, et al. Learning curve for laparoscopic major hepatectomy. Br J Surg. 2015;102(7):796–804. https://doi.org/10.1002/bjs.9798.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
All authors deny conflicts of interest pertinent to this work.
Additional information
Disclaimer: The National Cancer Data Base (NCDB) is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. The CoC’s NCDB and the hospitals participating in the CoC NCDB are the source of the de-identified data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Stiles, Z.E., Glazer, E.S., Deneve, J.L. et al. Long-Term Implications of Unplanned Conversion During Laparoscopic Liver Resection for Hepatocellular Carcinoma. Ann Surg Oncol 26, 282–289 (2019). https://doi.org/10.1245/s10434-018-7073-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-7073-6