Abstract
Background
Optimal margin width for breast-conserving therapy (BCT) after neoadjuvant chemotherapy (NAC) is unknown. We sought to determine the impact of margin width on local recurrence and survival after NAC and BCT.
Methods
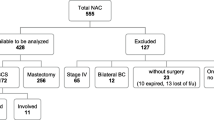
Patients treated with NAC and BCT for stage I–III breast cancer from 2002 to 2014 were identified. Multivariate Cox regression was performed to determine the relationship between margin width and local recurrence free-survival (LRFS), disease-free survival (DFS), and overall survival (OS).
Results
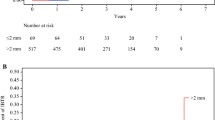
A total of 382 patients were included. Median age was 51 years [range 22–79], median tumor size 3.0 cm [range 0.6–11.0], and receptor subtypes included 144 (37.7%) HR−/HER2−, 47 (12.3%) HR−/HER2+, 118 (30.9%) HR+/HER2−, and 70 (18.3%) HR+/HER2+. Breast pathologic complete response (pCR) was achieved in 105 (27.5%) patients. Final margin status was positive in 8 (2.1%) patients, ≤ 1 mm in 65 (17.0%), 1.1–2 mm in 30 (7.9%), and > 2 mm in 174 (45.5%). The 5-year LRFS was 96.3% (95% CI 94.0–98.6), DFS was 85.5% (95% CI 81.8–90.7), and OS was 90.8% (95% CI 87.4–94.2). There was no difference in LRFS, DFS, or OS for margins ≤ 2 versus > 2 mm, and no difference in DFS or OS for margins ≤ 1 versus > 1 mm. HR+ subtype (p = 0.04) and pCR (p = 0.03) were correlated with favorable DFS and node negativity (p < 0.001) with favorable DFS and OS.
Conclusions
In this cohort treated with NAC and BCT, there was no association between margin width and LRFS, DFS, or OS. Although further studies are needed, the excellent long-term outcomes demonstrated in patients with close (≤ 2 mm) margins following NAC suggest that a margin of “no-ink-on-tumor” may be acceptable in appropriately selected patients.

Similar content being viewed by others
Change history
25 August 2018
In the original article, there is an error in Jungeun Choi’s affiliation. It is corrected as reflected here.
25 August 2018
In the original article, there is an error in Jungeun Choi?s affiliation. It is corrected as reflected here.
References
Rastogi P, Anderson SJ, Bear HD, et al. Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol. 2008;26:778–85.
van der Hage JA, van de Velde CJ, Julien JP, Tubiana-Hulin M, Vandervelden C, Duchateau L. Preoperative chemotherapy in primary operable breast cancer: results from the European Organization for Research and Treatment of Cancer trial 10902. J Clin Oncol. 2001;19:4224–37.
Swisher SK, Vila J, Tucker SL, et al. Locoregional control according to breast cancer subtype and response to neoadjuvant chemotherapy in breast cancer patients undergoing breast-conserving therapy. Ann Surg Oncol. 2016;3:749–56.
Chen AM, Meric-Bernstam F, Hunt KK, et al. Breast conservation after neoadjuvant chemotherapy: the MD Anderson Cancer Center Experience. J Clin Oncol. 2004;22:2303–12.
Mieog JS, van der Hage JA, van de Velde CJ. Neoadjuvant chemotherapy for operable breast cancer. Br J Surg. 2007;94:1189–200.
Houssami N, Macaskill P, Marinovich ML, Dixon JM, Irwig L, Brennan ME, Solin SJ. Meta-analysis of the impact of surgical margins on local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy. Eur J Cancer. 2010;46:3219–32.
Moran MS, Schnitt SJ, Giuliano AE, et al. Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. Ann Surg Oncol. 2014;21:704–16.
Rouzier R, Extra JM, Carton M, et al. Primary chemotherapy for operable breast cancer: incidence and prognostic significance of ipsilateral breast tumor recurrence after breast-conserving surgery. J Clin Oncol. 2001;19:3828–35.
Jwa E, Shin KH, Kim JY, et al. Locoregional recurrence by tumor biology in breast cancer patients after preoperative chemotherapy and breast conservation treatment. Cancer Res Treat. 2016;48:1363–72.
King TA, Morrow M. Surgical issues in patients with breast cancer receiving neoadjuvant chemotherapy. Nat Rev Clin Oncol. 2015;12:335–43.
R Development Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria (2008). http://www.R-project.org. ISBN 3-900051-07-0.
Bossuyt V, Provenzano E, Symmans WF, et al. Recommendations for standardized pathological characterization of residual disease for neoadjuvant clinical trials of breast cancer by the BIG-NABCG collaboration. Ann Oncol. 2015;26:1280–91.
Mukhtar RA, Yau C, Rosen M, Tandon VJ, I-SPY 1 TRIAL and ACRIN 6657 Investigators, Hylton N, Esserman LJ. Clinically meaningful tumor reduction rates vary by prechemotherapy MRI phenotype and tumor subtype in the I-SPY 1 TRIAL (CALGB 150007/150012; ACRIN 6657). Ann Surg Oncol. 2013;20:3823–30.
Volders JH, Haloua MH, Krekel NM, et al. Neoadjuvant chemotherapy in breast-conserving surgery—consequences on margin status and excision volumes: a nationwide pathology study. Eur J Surg Oncol. 2016;42:986–93.
Teshome M, Kuerer HM. Breast conserving surgery and locoregional control after neoadjuvant chemotherapy. Eur J Surg Oncol. 2017;43:865–74.
Boughey JC, McCall LM, Ballman KV et al. Tumor biology correlates with rates of breast-conserving surgery and pathologic complete response after neoadjuvant chemotherapy for breast cancer: findings from the ACOSOG Z1071 (Alliance) Prospective Multicenter Clinical Trial. Ann Surg 2014;260:608–14 (discussion 614–6).
Von Minckwitz G, Untch M, Blohmer JU, et al. Definition and impact of pathological complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30:1796–9.
Lovrics PJ, Cornacchi SD, Farrokhyar F, Garnett A, Chen V, Franic S, Simunovic M. Technical factors, surgeon case volume and positive margin rates after breast conservation surgery for early-stage breast cancer. Can J Surg. 2010;53:305–12.
Hanna J, Lannin D, Killelea B, Horowitz N, Chagpar AB. Factors associated with persistently positive margin status after breast-conserving surgery in women with breast cancer: an analysis of the national cancer database. Am Surg. 2016;82:748–52.
Lowery AJ, Kell MR, Glynn RW, Kerin MJ, Sweeney KJ. Locoregional recurrence after breast cancer surgery: a systematic review by receptor phenotype. Breast Cancer Res Treat. 2012;133:831–41.
Caudle AS, Yu TK, Tucker SL, et al. Local-regional control according to surrogate markers of breast cancer subtypes and response to neoadjuvant chemotherapy in breast cancer patients undergoing breast conserving therapy. Breast Cancer Res. 2012;14:R83.
Disclosures
The authors have no disclosures to declare.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Choi, J., Laws, A., Hu, J. et al. Margins in Breast-Conserving Surgery After Neoadjuvant Therapy. Ann Surg Oncol 25, 3541–3547 (2018). https://doi.org/10.1245/s10434-018-6702-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6702-4