Abstract
Background
This phase III study was undertaken to evaluate the efficacy of an allogeneic whole-cell vaccine (Canvaxin™) plus bacillus Calmette-Guerin (BCG) after complete resection of stage IV melanoma.
Methods
After complete resection of ≤5 distant metastases, patients were randomly assigned to BCG+Canvaxin (BCG/Cv) or BCG+placebo (BCG/Pl). The primary endpoint was overall survival (OS); secondary endpoints were disease-free survival (DFS), and immune response measured by skin test (ClinicalTrials.gov identifier: NCT00052156).
Results
Beginning in May 1998, 496 patients were randomized. In April 2005, the Data Safety Monitoring Board recommended stopping enrollment due to a low probability of efficacy. At that time, median OS and 5-year OS rate were 38.6 months and 44.9%, respectively, for BCG/Pl versus 31.4 months and 39.6% in the BCG/Cv group (hazard ratio (HR), 1.18; p = 0.250). Follow-up was extended at several trial sites through March 2010. Median OS and 5-year and 10-year survival was 39.1 months, 43.3 and 33.3%, respectively, for BCG/Pl versus 34.9 months, 42.5 and 36.4%, in the BCG/Cv group (HR 1.053; p = 0.696). Median DFS, 5- and 10-year DFS were 7.6 months, 23.8 and 21.7%, respectively, for BCG/Pl versus 8.5 months, 30.0%, and 30.0%, respectively, for the BCG/Cv group (HR 0.882; p = 0.260). Positive DTH skin testing correlated with increased survival.
Discussion
In this, the largest study of postsurgical adjuvant therapy for stage IV melanoma reported to date, BCG/Cv did not improve outcomes over BCG/placebo. Favorable long-term survival among study patients suggests that metastasectomy should be considered for selected patients with stage IV melanoma.
Similar content being viewed by others
Until 2011, no medical therapy had been shown to improve long-term survival in melanoma. In that dismal setting, surgical therapy for resectable distant metastases was commonly used by some centers and was associated with favorable outcomes relative to nonsurgically treated patients.1 Perhaps as many as 50% of melanoma patients will have resectable oligometastases on initial Stage IV presentation.2,3,4,5,6 In these patients, complete resection of distant metastatic melanoma has been reported to be associated with a median survival of 15–20 months and an average 5-year survival rate of ~20%.4,5,7,8,9,10,11,12 Postsurgical adjuvant phase II trials with Canvaxin™ (Cv) plus bacillus Calmette Guerin (BCG) demonstrated a median survival of 33 months and a 5-year survival rate of 36% warranting evaluation in a phase III trial.4,5 This report examines a trial of adjuvant vaccination after complete surgical resection of Stage IV melanoma in the era that predates modern drug availability.
In 1998, an international, randomized, double-blind, phase III study (the Malignant Melanoma Active Immunotherapy Trial in Stage IV disease [MMAIT-IV]) was initiated to examine the survival associated with complete resection of stage IV melanoma followed by Cv plus BCG or placebo (Pl) plus BCG. The study was terminated after the second interim analysis indicated a low probability of a significant survival benefit for the BCG/Cv arm. When enrollment was terminated in April 2005, 496 of the planned 670 patients had been randomized, making MMAIT-IV the largest adjuvant therapy study reported to date for resected stage IV melanoma. An extended follow-up protocol continued until March 2010 to obtain longer-term survival data.
Patients and Methods
Patients
This multicenter, randomized, double-blind study enrolled subjects with AJCC 5th edition stage IV melanoma (1998 staging guidelines), and no clinical evidence of disease after complete resection of distant soft tissue or lymph node metastases or metastases in deep iliac/obturator nodes (AJCC stage IV M1a) and/or distant lung or other visceral metastases (AJCC 5th ed. stage IV M1b).13 Prestudy computed tomography (CT) of chest, abdomen and pelvis, magnetic resonance imaging (MRI) or CT of the brain, and bone scan confirmed no evident disease at trial entry. Exclusion criteria included abnormal liver function and LDH >1.5 times the upper limit of normal. Patients could have no more than five metastases in no more than two visceral organ sites at the time of definitive surgery and were required to start study drug 14–90 days after surgery. Written informed consent, minimum life-expectancy of 5 years excluding the diagnosis of melanoma, and an ECOG performance status of 0–1 were required.
Procedures, Randomization, and Masking
Patients enrolled after providing informed consent to a protocol approved by the Institutional Review Board or Ethics Committee. After central confirmation of eligibility, patients were randomized 1:1 to receive either BCG plus Canvaxin (BCG/Cv) or BCG plus placebo (BCG/Pl). The study used a random permuted block design (block size = 20) with stratification by site of metastasis (soft tissue or nonvisceral lymph nodes [stage IV M1a] or visceral sites [stage IV M1b]) and number of metastatic lesions (1, 2–3, or 4–5). The identity of the investigational agent was masked to investigators and study personnel. Canvaxin or placebo was administered by intradermal injection on days 0, 14, 28, 42, and 56, monthly thereafter during year 1, every 2 months during year 2, and every 3 months during years 3 through 5. Vaccination was stopped at recurrence; however, BCG/Cv or BCG/Pl could be restarted after completion of treatment for recurrence. Patients who received systemic chemotherapy for recurrence did not receive additional study drug.
Investigational Products
Canvaxin™ was comprised of three irradiated whole-cells melanoma lines (M10-VACC, M24-VACC, and M101-VACC) suspended in RPMI 1640 containing 7.5% human serum albumin and 10% dimethyl sulfoxide; the placebo contained the same medium and additives but was free of melanoma cells.14 BCG (Tice strain, Organon Technika Inc., Durham NC) was given with the first two doses of study drug. BCG doses were 3 × 106 colony-forming units (cfu) on day 0 and 1.5 × 106 cfu on day 14 and were reduced based on prestudy PPD positivity.
Purified protein derivative (PPD) tuberculin tests were applied prior to the first injection and at day 28, day 56, and month 4, or until positive. A positive PPD was prespecified as >10 mm induration. The DTH response to Canvaxin in the Canvaxin group or to placebo in the placebo group was measured each time the agent was administered during the first 16 weeks. One tenth of the normal dose of the investigational agent (with no BCG) was administered intradermally. Induration was measured at 48 hours. DTH response was prespecified as induration of ≥7 mm during the first 12 weeks.15
Study Endpoints and Data Analysis
The primary endpoint was overall survival (OS). The study had 80% power to demonstrate a significant difference, assuming a treatment effect corresponding to a 33% increase in OS (hazard ratio 0.75) with a two-sided significance level of 0.05.
The primary analysis was of the intent-to-treat (ITT) population, defined as all patients randomized into the study. Secondary analyses assessed disease-free survival (DFS) and skin test immune response. Survivals were compared by stratified log-rank test. A proportional hazard (Cox) regression model was fitted to identify OS prognostic variables. Adverse events were graded according to the National Cancer Institute’s common toxicity criteria (Common Toxicity Criteria, Version 2.0. March 1998).
A Data Safety Monitoring Board (DSMB) monitored the study according to NCI guidelines, meeting at least yearly to review safety data and interim efficacy analyses. A stochastic curtailment procedure was used to provide conditional power estimates. The funder of the study had no role in study design, data collection, analysis, interpretation, or manuscript preparation. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Between May 1998 and April 2005, 496 patients were enrolled and randomized at 69 centers (Fig. 1). There was no significant difference in demographic or disease characteristics between the two arms (Table 1). Patients in BCG/Pl and BCG/Cv groups had received radiation therapy (10 and 11%, respectively), chemotherapy (11 and 8%, respectively), biotherapy (16 and 11%, respectively), and/or immunotherapy (17 and 14%, respectively).
The median duration of study drug administration was 8.1 months for both arms. When accrual was stopped, median follow-up was 13.8 months for the BCG/Cv group and 16.4 months for the BCG/Pl group. Early termination of the trial raised concern that long-term survival estimates may be imprecise. Therefore, high-accruing multicenter sites continued to monitor patients under a follow-up protocol (Fig. 1b), extending median follow-up from 15.1 months to 19.7 months (BCG.CV 19.0 months, BCG/Pl 20.5 months).
There were 112 (45%) deaths in the BCG/Pl group and 116 (47%) deaths in the BCG/Cv group. Seven patients in the BCG/Pl group and six in the BCG/Cv group died of nonmelanoma causes. By ITT analysis, median OS was 38.6 months in the BCG/Pl group and 34.9 months in the BCG/Cv group (hazard ratio [HR], 1.04; 95% confidence interval [CI] 0.80–1.35; p = 0.773). The 5-year and 10-year OS rates were, respectively, 43.0 and 33.0% in the BCG/Pl group and 42.7 and 36.6% in the BCG/Cv group (Fig. 2a). Per-protocol analysis (excluding 38 BCG/Pl and 45 BCG/Cv patients who did not receive 12 weeks of study drug or had a significant protocol violation) showed a similar hazard ratio (HR 0.97; 95%; CI 0.73–1.31; p = 0.858).
Median OS for patients with M1a melanoma was 60.6 months with BCG/Pl versus 36.3 months with BCG/Cv (HR 1.28; 95% CI 0.85–1.91; p = 0.235; Fig. 2b); median OS for patients with M1b melanoma was 29.9 months with BCG/Pl versus 33.0 months with BCG/Cv (HR 0.906; 95% CI 0.65–1.27; p = 0.571; Fig. 2c). Among the 183 patients with lung metastases (Table 1), median OS, 5-year OS and 10-year OS were 33.8 months, 37.6 and 25.6%, respectively, with BCG/Pl and 29.3 months, 36.1 and 28.8%, respectively, with BCG/Cv (HR 0.99, 95% CI 0.66–1.48; p = 0.948).
Resection of a single metastatic lesion yielded a median survival of 38.6 months with BCG/Pl versus 34.9 months with BCG/Cv (HR 0.97; 95% CI 0.69–1.38, p = 0.879); resection of 2–5 lesions yielded a median survival of 43.3 months with BCG/Pl versus 26.6 months with BCG/Cv (HR 1.14; 95% CI 0.77–1.67, p = 0.516). There was no significant difference in OS related to the number of lesions resected (Fig. 2d). Regression analysis showed two significant factors for OS: diagnosis of stage III disease prior to stage IV (HR 1.37; 95% CI 1.03–1.84; p = 0.029) and an elevated serum LDH level before the first dose of study drug (HR 1.50; 95% CI 1.00–2.26; p = 0.047; Table 2).
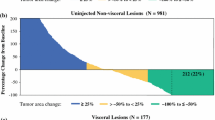
Recurrence occurred in 167 (67%) BCG/Pl patients and 155 (63%) BCG/Cv patients. Seven patients in the BCG/Pl group and six in the BCG/Cv group died without recurrence. Median DFS was 7.6 months for BCG/Pl and 8.5 months for BCG/Cv (HR 0.88; 95% CI 0.71–1.10; p = 0.260; Fig. 3). Most first recurrences (84%) occurred within 12 months after study entry. DFS for BCG/Pl and BCG/Cv arms, respectively, was 39.9 and 43.6% at 1 year and 23.8 and 30.0% at 5 years. Most patients with recurrence received surgery [n = 142, (43.7%)] and/or systemic chemotherapy [n = 125 (38.5%)] or biotherapy [n = 64 (28.3%)].
In the BCG/Pl group, the number of patients with a positive DTH to placebo was 29 (12%). In the BCG/Cv group, the number of patients with a positive DTH to Canvaxin was 178 (75%). In the BCG/Cv group, survival was longer in responders than in nonresponders (HR 0.61; p = 0.023; Table S1a). If a positive response was defined as 10 mm in duration, median OS was 47.3 months versus 25.6 months (HR 0.56; p = 0.003).
In the BCG/Pl group, the number of patients with a positive PPD response was 132 (53%). In the BCG/Cv group, the number of patients with a positive PPD response was 148 (60%). In the BCG/Cv group, survival was longer in PPD responders than in nonresponders (HR 0.62; p = 0.010; Table S1b). Survival was not significantly different between responders and nonresponders in the BCG/Pl group (HR 0.77; p = 0.160).
Adverse Events
Adverse events were similar between the two study arms. The most common adverse events were localized injection site reactions including ulceration (approximately 60% of patients). This occurred almost exclusively during the first 8 weeks and did not vary by study arm (BCG/Cv 55% vs. BCG/Pl 59%). Other adverse events comprised transient constitutional symptoms, such as fatigue, pyrexia, and rigors. Less than 1% of patients were unable to tolerate treatment (1 patient in the BCG/Pl arm and 2 patients in the BCG/Cv arm). Vitiligo developed in 15 BCG/Pl patients and 13 BCG/Cv patients. There were no cases of melanoma-associated retinopathy.
Discussion
Despite a clear biological rationale and strong Phase 2 trial data, there was no indication of either benefit or harm from adjuvant treatment with vaccine compared to placebo in this study.16,17 Outcome data from earlier vaccine trials was confirmed with very favorable survival observed in vaccine-treated patients, but similarly favorable survival was seen among postsurgical patients receiving BCG and placebo. Indeed, among trial patients as a whole, survival beyond 5 years was experienced by more than 40%, even in an era that predates broadly effective systemic treatment. To our knowledge, this is the highest 5-year survival ever reported in a phase III trial for Stage IV melanoma. Whereas longer-term follow-up would be desirable, we believe these outcomes are robust in a clinical era when median survivals were very short. Although the reasons for this high survival in both arms are unknown, three possible explanations can be considered: selection bias, a beneficial effect of metastasectomy, or a beneficial effect of BCG.
As is typical for clinical trial populations, selection bias is very likely to have resulted in more favorable outcomes in this study. The selection process was particularly rigorous in this case, because all patients needed to be resected to no evidence of disease. Estimates of the fraction of stage IV patients who fall into this category vary. Data from the JWCI melanoma database indicate that 86% of stage IV patients present with single-organ involvement, and the first Multicenter Selective Lymphadenectomy Trial found that 55% of patients underwent surgery as initial treatment for Stage IV recurrence.3,18 Others have found a much lower percentage of surgical candidates at the time of stage IV presentation.19
Resectability does not appear to be an adequate explanation for the high survival in the study. Numerous prior series have demonstrated 5-year survival following surgical treatment alone in the 20% range, and a registry study performed by the Southwest Oncology Group confirmed these results prospectively.11 Retrospective matched-pair analysis among resected stage IV patients demonstrated 5-year survivals rates of 39% for vaccine-treated patients and 20% for nonvaccine-treated patients.5 One additional level of selection for MMAIT patients, relative to historic controls, was the requirement for more current radiographic staging studies for trial eligibility. Subjects were required to begin injections within 90 days of surgery and to have had CT scans of chest, abdomen, and pelvis and brain imaging within 45 days of randomization. This could exclude some patients with very early recurrence who might not have been excluded from the historic analyses.
The use of BCG also distinguishes the study populations from historical controls. The therapeutic effect of adjuvant BCG has been the subject of considerable debate. Although randomized trials have not demonstrated benefit, most of those trials were markedly underpowered, inadequately stratified, or complicated by the concomitant use of cytotoxic therapy.20,21,22 Several studies have shown decreased melanoma incidence and improved prognosis among patients who have had prior vaccination, including to BCG.23,24 No prior trial has evaluated the dose or schedule of BCG administration used in the present study, in which there was a strong correlation between both OS and DFS and PPD response. This dose was developed early during vaccine development based on an increased an immune response and PPD conversion. While this may simply reflect a correlation of outcome and immune competence, intradermal and intratumoral BCG injections also are known to cause regression of injected and noninjected, clinically evident metastases. Therefore, a therapeutic effect is certainly plausible.25,26
The past several years have seen a revolution in the systemic treatment of melanoma.27,28,29,30 Successful development of numerous drug therapies has changed the context in which resection of melanoma metastases is considered. For example, far more patients who experience a partial or mixed response to drug treatment may now be candidates for resection either to consolidate their response or to eliminate specific tumors with demonstrated treatment resistance. Appropriate patient selection has always been a vital consideration for metastasectomy, using factors, such as tumor-volume doubling-time, disease-free interval, and comorbidities.18,31,32 The increased efficacy of drug therapy may shift the balance of these factors, increasing the number of patients who undergo initial systemic therapy, rather than up-front surgery. However, none of this changes the observation of this study that, even in the absence of effective systemic therapy, long-term survival can be achieved by surgical resection of metastases. Given the expense of recently approved drug therapies, surgical resection also is likely to be relatively very cost-effective. Despite recent advances, a large percentage of patients with metastatic melanoma will die of metastatic melanoma, and we must afford them every opportunity for potentially effective therapy. This must continue to include consideration of metastasectomy in appropriate patients.
References
Ollila D, Hsueh E, Stern S, Morton D. Metastasectomy for recurrent stage IV melanoma. J Surg Oncol. 1999;71(4):209–13.
Ozao-Choy J, Lee DJ, Faries MB. Melanoma vaccines: mixed past, promising future. Surg Clin North Am. 2014;94(5):1017–30, viii.
Howard JH, Thompson JF, Mozzillo N, et al. Metastasectomy for distant metastatic melanoma: analysis of data from the first Multicenter Selective Lymphadenectomy Trial (MSLT-I). Ann Surg Oncol. 2012;19(8):2547–55.
Morton D, Ollila D, Hsueh E, Essner R, Gupta R. Cytoreductive surgery and adjuvant immunotherapy: a new management paradigm for metastatic melanoma. CA Cancer J Clin. 1999;49(2):101–16.
Hsueh E, Essner R, Foshag L, et al. Prolonged survival after complete resection of disseminated melanoma and active immunotherapy with a therapeutic cancer vaccine. J Clin Oncol. 2002;20(23):4549–54.
Wasif N, Bagaria SP, Ray P, Morton DL. Does metastasectomy improve survival in patients with Stage IV melanoma? A cancer registry analysis of outcomes. J Surg Oncol. 2011;104(2):111–5.
Wong SL, Coit DG. Role of surgery in patients with stage IV melanoma. Curr Opin Oncol. 2004;16(2):155–60.
Essner R, Lee JH, Wanek LA, Itakura H, Morton DL. Contemporary surgical treatment of advanced-stage melanoma. Arch Surg. 2004;139(9):961–6; discussion 6–7.
Karakousis C, Velez A, Driscoll D, Takita H. Metastasectomy in malignant melanoma. Surgery. 1994;115(3):295–302.
Meyer T, Merkel S, Goehl J, Hohenberger W. Surgical therapy for distant metastases of malignant melanoma. Cancer. 2000;89(9):1983–91.
Sosman JA, Moon J, Tuthill RJ, et al. A phase 2 trial of complete resection for stage IV melanoma: results of Southwest Oncology Group Clinical Trial S9430. Cancer. 2011;117(20):4740–6.
Harpole D, Johnson C, Wolfe W, George S, Seigler H. Analysis of 945 cases of pulmonary metastatic melanoma. J Thorac Cardiovasc Surg. 1992;103(4):743–8.
American Joint Committee on Cancer. AJCC Cancer Staging Manual, 5th edn. Philadelphia: Lippincott-Raven; 1997.
Morton D, Foshag L, Hoon D, et al. Prolongation of survival in metastatic melanoma after active specific immunotherapy with a new polyvalent melanoma vaccine. Ann Surg. 1992;216(4):463–82.
Hsueh E, Gupta R, Qi K, Morton D. Correlation of specific immune responses with survival in melanoma patients with distant metastases receiving polyvalent melanoma cell vaccine. J Clin Oncol. 1998;16(9):2913–20.
Hsueh E, Nathanson L, Foshag L, et al. Active specific immunotherapy with polyvalent melanoma cell vaccine for patients with in-transit melanoma metastases. Cancer. 1999;85:2160–9.
Morton D, Hoon D, Nizze J, et al. Polyvalent melanoma vaccine improves survival of patients with metastatic melanoma. Ann NY Acad Sci. 1993;690:120–34.
Barth A, Wanek L, Morton D. Prognositic factors in 1,521 melanoma patients with distant metastases. J Am Coll Surg. 1995;181(3):193–201.
Wevers KP, Hoekstra HJ. Stage IV melanoma: completely resectable patients are scarce. Ann Surg Oncol. 2013;20(7):2352–6.
Paterson AH, Willans DJ, Jerry LM, Hanson J, McPherson TA. Adjuvant BCG immunotherapy for malignant melanoma. Can Med Assoc J. 1984;131(7):744–8.
Eilber F, Morton D, Holmes E, Sparks F, Ramming K. Adjuvant immunotherapy with BCG in treatment of regional lymph node metastases from malignant melanoma. N Engl J Med. 1976;294(5):237–40.
Agarwala SS, Neuberg D, Park Y, Kirkwood JM. Mature results of a phase III randomized trial of bacillus Calmette-Guerin (BCG) versus observation and BCG plus dacarbazine versus BCG in the adjuvant therapy of American Joint Committee on Cancer Stage I-III melanoma (E1673): a trial of the Eastern Oncology Group. Cancer. 2004;100(8):1692–8.
Kolmel KF, Grange JM, Krone B, et al. Prior immunisation of patients with malignant melanoma with vaccinia or BCG is associated with better survival. A European Organization for Research and Treatment of Cancer cohort study on 542 patients. Eur J Cancer. 2005;41(1):118–25.
Krone B, Kolmel KF, Henz BM, Grange JM. Protection against melanoma by vaccination with Bacille Calmette-Guerin (BCG) and/or vaccinia: an epidemiology-based hypothesis on the nature of a melanoma risk factor and its immunological control. Eur J Cancer. 2005;41(1):104–17.
Morton D, Eilber F, Holmes E, et al. BCG immunotherapy of malignant melanoma: summary of a seven-year experience. Ann Surg. 1974;180(4):635–43.
Kidner TB, Morton DL, Lee DJ, et al. Combined intralesional Bacille Calmette-Guerin (BCG) and topical imiquimod for in-transit melanoma. J Immunother. 2012;35(9):716–20.
Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–23.
Flaherty KT, Puzanov I, Kim KB, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med. 2010;363(9):809–19.
Wolchok JD, Kluger H, Callahan MK, et al. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 369(2):122–33.
Hamid O, Robert C, Daud A, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369(2):134–44.
Ollila D, Stern S, Morton D. Tumor doubling time: a selection factor for pulmonary resection of metastatic disease. J Surg Oncol. 1999;69(4):206–11.
Wood T, DiFronzo A, Rose M, et al. Does complete resection of melanoma metastatic to solid intraabdominal organs improve survival? Ann Surg Oncol. 2001;8(8):658–62.
Acknowledgment
Supported by grants CA76489 and CA012582 from the National Institutes of Health, National Cancer Institute, and by funding from the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Cancer Institute or the National Institutes of Health. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication. The trial was also funded by CancerVax Corporation, Carlsbad, CA.
Collaborators of the MMAIT-IV Clinical Trial Group
John F. Thompson, MD (Royal Prince Alfred Hospital, Sydney, Australia); Mark Smithers, MB, BS (Princess Alexandra Hospital, Brisbane, Australia); Michael Hughes, MBBS (Westmead Hospital, Westmead, Australia); Brendon J. Coventry, MB, BS, PhD (Royal Adelaide Hospital, Adelaide, Australia); Jeremy Shapiro, MBBS (Alfred Hospital, Melbourne, Australia); Grant McArthur, MBBS, PhD (Peter MacCallum Cancer Centre, Melbourne, Australia); Antonio Buzaid, MD (Hospital Sirio Libanes, Sao Paulo, Brazil); Wilson Miller, MD (McGill University, Montreal, Quebec, Canada); Dirk Schadendorf, MD (University Hospital of Mannheim, Mannheim, Germany); Claus Garbe, MD (University of Tuebingen, Tuebingen, Germany); Martin Kaatz, MD (University of Jena, Jena, Germany); Ralf Uwe Peter, MD, PhD (University of Ulm, Ulm, Germany); Patrick Terheyden, MD (University Hospital Wuerzburg, Wuerzburg, Germany); Angus Dalgleish, MD (St. George’s Hospital Medical School, London, Great Britain); Paul Redmond, MD (Cork University Hospital, Cork, Ireland); Schlomo Schneebaum, MD (Tel-Aviv Sourasky Medical Center, Tel Aviv, Israel); Nicola Mozzillo, MD (Istituto Nazionale dei Tumori de Napoli, Naples, Italy); Alessandro Testori, MD (Istituto Europeo Di Oncologia, Milan, Italy); Mario Santinami, MD (Istituto Nazionale dei Tumori-Milano, Milan, Italy); Harald J. Hoekstra, MD, PhD (University Medical Center Groningen and University of Groningen, Groningen, The Netherlands); Michael McCrystal, MD (North Shore Hospital, Auckland, New Zealand); Reinhard Dummer, MD (University of Zurich, Zurich, Switzerland); Mohammed Kashani-Sabet, MD (University of California, San Francisco, Mt. Zion Medical Center, CA, USA); Mark C. Kelley, MD (Vanderbilt University, Nashville, TN, USA); Ronald DeConti, MD (H. Lee Moffitt Cancer Center, Tampa, FL, USA); Jeffrey Lee, MD (MD Anderson Cancer Center, Houston, TX, USA); James F. Huth, MD (University of Texas Southwestern Medical Center at Dallas, Dallas, TX, USA); Mark Faries, MD (John Wayne Cancer Institute, Santa Monica, CA, USA); Jeffrey Wagner, TX (Wagner, Wagner & Associates, Indianapolis, IN, USA); Evan Hersh, MD (Arizona Cancer Center, Tucson, AZ, USA); Clay Anderson, MD (University of Missouri, Columbia, MO, USA); Kelly McMasters, MD (University of Louisville, Louisville, KY, USA); Lynn Schuchter, MD (University of Pennsylvania Cancer Center, Philadelphia, PA, USA); Constantine P. Karakousis, MD, PhD (Millard Fillmore Hospital, Buffalo, NY, USA); William Kraybill, MD (Roswell Park Cancer Institute, Buffalo, NY, USA); Rene Gonzalez, MD (University of Colorado Cancer Center, Aurora, CO, USA); David Byrd, MD (University of Washington, Seattle, WA, USA); David Ollila, MD (University of North Carolina-Chapel Hill, Chapel Hill, NC, USA); Michael Walker, MD (Ohio State University, Columbus, OH, USA); Ernest Borden, MD (Cleveland Clinic Foundation, Cleveland, OH, USA); Marie-France Demierre, MD (Boston Medical Center, Boston, USA); Dirk Noyes, MD (IHC Cancer Services-LDS Hospital, Salt Lake City, UT, USA); Douglas Reintgen, MD (Lakeland Regional Cancer Center, Lakeland, FL, USA); Lee Riley, MD (St. Luke’s Hospital Cancer Center, Bethlehem, PA, USA); Kathy Yao, MD (Loyola University Medical Center, Chicago, IL, USA); Howard Kaufman, MD (Columbia University, New York, NY, USA); Philip Leming, MD (Christ Hospital, Cinncinnati, OH, USA); Edward Levine, MD (Wake Forest University, Winston-Salem, NC, USA); Neal Ready, MD (BrUOG-Rhode Island Hospital, Providence, RI, USA); Gregory Sarna, MD (Cedars-Sinai Comprehensive Cancer Center, Los Angeles, CA, USA); William Sharfman, MD (Sidney Kimel Comprehensive Cancer Center at Johns Hopkins, Baltimore, MD, USA); Robert Dillman, MD (Hoag Cancer Center, Huntington Beach, CA, USA); Norman Estes, MD (OSF Saint Francis Medical Center, Peoria, IL, USA); Laura Hutchins, MD (University of Arkansas for Medical Sciences (UAMS), Little Rock, AK, USA); Andrew Pecora, MD (Hackensack University Medical Center, Hackensack, NJ, USA); John Richart, MD (St. Louis University Health Sciences Center, St. Louis, MO, USA); Neal Rothschild, MD (Palm Beach Cancer Institute, West Palm Beach, FL, USA); John Vetto, MD (Oregon Health Sciences University, Portland, OR, USA); Harold Wanebo, MD (BrUOG-Roger Williams Hospital, Providence, RI, USA); Michael Warso, MD (University of Illinois at Chicago, Chicago, IL, USA); Ned Carp, MD, PhD (Lankenau Hospital, Wynnewood, PA, USA); George Elias, MD (Franklin Square Hospital Center, Baltimore, MD, USA); Mark Greene, MD (Mayo Clinic Scottsdale, AZ, USA); David Hyams, MD (Comprehensive Cancer Center of the Desert, Palm Springs, CA, USA); Jose Lutzky, MD (Mt. Sinai Comprehensive Cancer Center, Miami Beach, FL, USA); Jonathan Polikoff, MD (Kaiser Hospital, Riverside, CA, USA); Armando Sardi, MD (St. Agnes Healthcare, Baltimore, MD, USA); Frank Senecal, MD (Northwest Medical Specialties, Tacoma, WA, USA).
Disclosures
Guy Gammon, Daniel Pertschuk and Christopher Nardo were employees of the CancerVax Corporation. Donald L. Morton was a stockholder and patent holder for CancerVax Corporation and Canvaxin, respectively. There are no other relelvant conflicts.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Collaborators of the MMAIT-IV Clinical Trial Group are listed in “Acknowledgment”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Faries, M.B., Mozzillo, N., Kashani-Sabet, M. et al. Long-Term Survival after Complete Surgical Resection and Adjuvant Immunotherapy for Distant Melanoma Metastases. Ann Surg Oncol 24, 3991–4000 (2017). https://doi.org/10.1245/s10434-017-6072-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-6072-3