Abstract
Background
Circulating monocyte-derived, tumor-associated macrophages are associated with a poor prognosis for various cancers. Conversely, circulating lymphocytes are the source of tumor-infiltrating lymphocytes, which are associated with an improved prognosis. This study evaluated the prognostic value of the preoperative blood lymphocyte-to-monocyte ratio (LMR) for patients undergoing hepatectomy for liver-only colorectal metastases.
Methods
This retrospective study examined 140 consecutive patients with liver-only colorectal metastases. Disease-free survival (DFS), post-recurrence survival (PRS), cancer-specific survival (CSS), and overall survival (OS) were analyzed in relation to LMR values using both Kaplan–Meier and multivariate Cox-regression methods.
Results
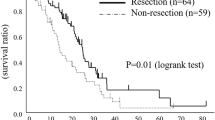
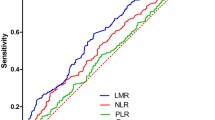
In the multivariate analysis, high LMR (>3) was significantly associated with increased OS [hazard ratio (HR), 2.43; 95 % confidence interval (CI), 1.32–4.48; P = 0.004], CSS (HR 2.15; 95 % CI 1.13–4.10; P = 0.020), and PRS (HR 2.15; 95 % CI 1.15–4.01; P = 0.016) but not with DFS. An LMR lower than 3 may have been associated with decreased CSS and PRS by increasing the rate of multifocal recurrence (P = 0.063). In the multivariate analysis comparing LMR, the neutrophil–lymphocyte ratio, and the platelet-lymphocyte ratio, LMR remained the only significant prognostic variable of CSS.
Conclusion
This study identified preoperative LMR as an independent prognostic factor for PRS, CSS, and OS but not for DFS in patients undergoing hepatectomy for liver-only colorectal metastases. In the future, interventions to augment immune function could improve survival for low-LMR patients.


Similar content being viewed by others
References
Grundmann RT. Current state of surgical treatment of liver metastases from colorectal cancer. World J Gastrointest Surg. 2011;3:183–96.
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230:309–21.
John SK, Robinson SM, Rehman S, et al. Prognostic factors and survival after resection of colorectal liver metastasis in the era of preoperative chemotherapy: an 11-year single-centre study. Dig Surg. 2013;30:293–301.
Tomlinson JS, Jarnagin WR, DeMatteo RP, et al. Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol. 2007;25:4575–80.
Ayez N, Lalmahomed ZS, Van der Pool AEM, et al. Is the clinical risk score for patients with colorectal liver metastases still useable in the era of effective neoadjuvant chemotherapy? Ann Surg Oncol. 2011;18:2757–763.
Nakagawa K, Tanaka K, Nojiri K, Kumamoto T, Takeda K, Ueda M, Endo I. The modified Glasgow prognostic score as a predictor of survival after hepatectomy for colorectal liver metastases. Ann Surg Oncol. 2014;21:1711–8.
Halazun KJ, Aldoori A, Malik HZ, Al-Mukhtar A, Prasad KR, Toogood GJ, Lodge JP. Elevated preoperative neutrophil to lymphocyte ratio predicts survival following hepatic resection for colorectal liver metastases. Eur J Surg Oncol. 2008;34:55–60.
Neofytou K, Smyth EC, Giakoustidis A, Khan AZ, Cunningham D, Mudan S. Elevated platelet-to-lymphocyte ratio predicts poor prognosis after hepatectomy for liver-only colorectal metastases, and it is superior to neutrophil to lymphocyte ratio as an adverse prognostic factor. Med Oncol. 2014;31:239–48.
Kawai O, Ishii G, Kubota K, et al. Predominant infiltration of macrophages and CD8(+) T cells in cancer nests is a significant predictor of survival in stage IV nonsmall cell lung cancer. Cancer. 2008;113:1387–95.
Corthay A. Does the immune system naturally protect against cancer? Front Immunol. 2014;5:197.
Balermpas P, Rödel F, Liberz R, et al. Head and neck cancer relapse after chemoradiotherapy correlates with CD163+ macrophages in primary tumor and CD11b+ myeloid cells in recurrences. Br J Cancer. 2014;111:1509–18.
Bingle L, Brown NJ, Lewis CE. The role of tumor-associated macrophages in tumor progression: implications for new anticancer therapies. J Pathol. 2002;196:254–65.
Stotz M, Pichler M, Absenger G, et al. The preoperative lymphocyte to monocyte ratio predicts clinical outcome in patients with stage III colon cancer. Br J Cancer. 2014;110:435–40.
Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–16.
Schmidt H, Bastholt L, Geertsen P, Christensen IJ, Larsen S, Gehl J, von der Maase H. Elevated neutrophil and monocyte counts in peripheral blood are associated with poor survival in patients with metastatic melanoma: a prognostic model. Br J Cancer. 2005;93:273–8.
Porrata LF, Ristow K, Colgan JP, et al. Peripheral blood lymphocyte/monocyte ratio at diagnosis and survival in classical Hodgkin’s lymphoma. Haematologica. 2012;97:262–9.
Szkandera J, Gerger A, Liegl-Atzwanger B, et al. The lymphocyte/monocyte ratio predicts poor clinical outcome and improves the predictive accuracy in patients with soft tissue sarcomas. Int J Cancer. 2014;135:362–70.
Koh YW, Park CS, Yoon DH, Suh C, Huh J. Should the cutoff values of the lymphocyte-to-monocyte ratio for prediction of prognosis in diffuse large B-cell lymphoma be changed in elderly patients? Eur J Haematol. 2014;93:340–8.
Kubota K, Kadomura T, Ohta K, et al. Analyses of laboratory data and establishment of reference values and intervals for healthy elderly people. J Nutr Health Aging. 2012;16:412–6.
Wolchok JD, Kluger H, Callahan MK, et al. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 2013;369:122–33.
Robert C, Thomas L, Bondarenko I, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364:2517–26.
Hoffmann TK, Dworacki G, Tsukihiro T, Meidenbauer N, Gooding W, Johnson JT, Whiteside TL. Spontaneous apoptosis of circulating T lymphocytes in patients with head and neck cancer and its clinical importance. Clin Cancer Res. 2002;8:2553–62.
Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21:137–48.
Rabinowich H, Cohen R, Bruderman I, Steiner Z, Klajman A. Functional analysis of mononuclear cells infiltrating into tumors: lysis of autologous human tumor cells by cultured infiltrating lymphocytes. Cancer Res. 1987;47:173–7.
Väyrynen JP, Tuomisto A, Klintrup K, Mäkelä J, Karttunen TJ, Mäkinen MJ. Detailed analysis of inflammatory cell infiltration in colorectal cancer. Br J Cancer. 2013;109:1839–47.
Fidler IJ, Schroit AJ. Recognition and destruction of neoplastic cells by activated macrophages: discrimination of altered self. Biochim Biophys Acta. 1988;948:151–73.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–44.
Pollard JW. Tumor-educated macrophages promote tumor progression and metastasis. Nat Rev Cancer. 2004;4:71–8.
Richards DM, Hettinger J, Feuerer M. Monocytes and macrophages in cancer: development and functions. Cancer Microenviron. 2013;6:179–91.
Acknowledgment
This study was supported by the National Institute for Health Research Royal Marsden/Institute for the Cancer Research Biomedical Research Centre.
Disclosure
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Neofytou, K., Smyth, E.C., Giakoustidis, A. et al. The Preoperative Lymphocyte-to-Monocyte Ratio is Prognostic of Clinical Outcomes for Patients with Liver-Only Colorectal Metastases in the Neoadjuvant Setting. Ann Surg Oncol 22, 4353–4362 (2015). https://doi.org/10.1245/s10434-015-4481-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4481-8