Abstract
Background
Although fluorescein angiography (FA) is a frequently used imaging modality in patients with non-infectious uveitis (NIU), it has not been reliably used for objective assessment of posterior segment inflammatory outcomes in these patients. In this index study we report the posterior segment inflammatory outcomes of two different doses of intravenous (IV) infusions of tocilizumab (TCZ), an IL-6 inhibitor, in eyes with NIU using a semi-quantitative FA scoring system.
Methods
STOP-Uveitis is a randomized, multi-center clinical trial conducted at 5 clinical centers across the United States. The study evaluated the role of TCZ in patients with NIU. Thirty-seven (37) patients with NIU were randomized into one of two treatment groups in a ratio of 1:1. Group 1 received IV infusions of 4 mg/kg TCZ and group 2 received IV infusions of 8 mg/kg TCZ. Infusions were given every 4 weeks in both groups until month 6 (primary endpoint). Posterior segment inflammatory outcomes were assessed by evaluating FA at baseline and month 6 by graders at a central reading center. A previously reported, semi-quantitative, scoring system for FA was used to assess signs that represent ongoing inflammatory processes in the posterior segment. These signs included optic disc hyperfluorescence, macular edema, retinal vascular staining and/or leakage, capillary leakage, retinal capillary nonperfusion, neovascularization of the optic disc, neovascularization elsewhere, pinpoint leaks, and retinal staining and/or subretinal pooling. Statistical significance was set at p < 0.05. Main outcome measures included change in posterior segment inflammation as assessed using FA at month 6.
Results
37 eyes (37 patients) were randomized in the STOP-Uveitis study. 30 eyes were found to be eligible for this sub-study based on study criteria. Seven eyes had ungradable images at either baseline or month 6 and were therefore excluded from the analysis. The reduction in FA inflammatory scores at month 6 were statistically significant in both groups (p < 0.05). The difference between the two groups was not significant (p = 0.351).
Conclusions
IV infusions of tocilizumab (both 4 and 8 mg/kg) are effective in improving posterior segment inflammation in eyes with NIU. A semi-quantitative FA scoring system may be used as a reliable outcome measure for assessment of posterior segment inflammation.
ClinicalTrials.gov Identifier: NCT01717170
Similar content being viewed by others
Background
Uveitis and its complications, account for approximately 5–20% of cases of preventable blindness in the developed world, and up to 25% of cases in developing countries [1]. The primary aim in the management of patients with uveitis is to achieve and maintain quiescence in inflammation and prevent the development of ocular adverse events. Although corticosteroids are still considered the first-line therapy for patients with non-infectious uveitis (NIU), they are associated with considerable local and systemic side effects. Therefore, steroid-sparing agents such as Tocilizumab (TCZ), are currently under investigation. TCZ is a recombinant humanized monoclonal antibody directed against IL-6; which is a pro-inflammatory cytokine with a proven role in immune mediated diseases such as uveitis. The Study of the safety, tolerability, and bioactivity of Tocilizumab On Patients with non-infectious Uveitis (STOP-Uveitis) study was the first multicenter, randomized, open label clinical trial evaluating two different doses of TCZ (4 mg/kg and 8 mg/kg) in patients with NIU. The study has previously reported a favorable safety and efficacy profile at the month 6 primary endpoint of the study [2].
Although the vitreous haze (VH) score is a commonly used clinical marker for posterior segment inflammation in patients with NIU, it may not be the most reliable marker since every patient may not initially present with significant vitreous haze. Therefore, alternative methods to reliably assess posterior segment inflammatory outcomes in patients with uveitis need to be explored. Fluorescein Angiography (FA) is a frequently used imaging modality in patients with NIU. However, FA analyses are qualitative, and grader dependent, making comparisons among different end points challenging. To overcome this challenge, different fluorescein angiography scoring schemes have been previously reported [3,4,5]. The Angiography Scoring for Uveitis Working Group (ASUWOG) have reported a semi-quantitative scoring system using fluorescein and indocyanine angiography, to assess posterior segment inflammation in patients with uveitis [6]. We used this particular scoring system for the grading of posterior segment inflammation in our study because it evaluates both the extent (area of fundus involved) and the magnitude (severity) of the most important inflammatory parameters in patients with NIU including; optic disc hyperfluorescence; macular edema; retinal vascular staining/leakage; capillary leakage; retinal capillary nonperfusion; neovascularization of the optic disc (NVD); neovascularization elsewhere (NVE); pinpoint leaks; retinal staining/pooling. (Table 1) In addition, this scoring system has been previously utilized extensively in clinical studies evaluating several ocular inflammatory diseases with the authors reporting good inter-grader agreement [7,8,9,10,11,12].
In this index study, we assessed posterior segment inflammatory outcomes using a FA scoring system in patients with NIU treated with two different monthly infusions of Tocilizumab.
Methods
Data from the STOP-Uveitis study was utilized for this study. The STOP-Uveitis study was a multicenter, randomized, open-label clinical trial designed to assess the safety and efficacy of repeated intravenous (IV) infusions of two doses of TCZ (4 mg/kg and 8 mg/kg) in subjects with non-infectious uveitis (NIU). The infusions were administered over one hour.
The STOP-Uveitis trial is registered at http://www.clinicaltrials.gov under the identifier NCT01717170 and was conducted in compliance with the United States Code of Federal Regulations Title 21, the Declaration of Helsinki, and the Harmonized Tripartite Guidelines for Good Clinical Practice (1996). The study was approved by local institutional review boards for selected sites and by a central review board for others. Signed informed consents were obtained from all the participants in the study.
Fluorescein angiography images were acquired using the Zeiss FF-450 Fundus Camera (Carl Zeiss Meditec Inc., Dublin, CA) at 2 study sites, and using the Topcon TRC-50DX (Topcon Corporation, Tokyo, Japan) fundus camera at 3 study sites. OCT imaging was performed using the Heidelberg Spectralis HRA + OCT device (Heidelberg Engineering, Heidelberg, Germany) at all the study sites.
Patient eligibility and exclusion criteria
Patients were included in the index sub-study analysis if they met the following criteria: (1) participation in the STOP-Uveitis clinical trial and completion of the primary end-point visit of month 6; (2) availability of gradable fluorescein angiography images at baseline and month 6. Eyes with ungradable images at the baseline and/or month 6 visit were excluded from the analysis. Inclusion and exclusion criteria of the STOP-Uveitis study have been published previously [2].
Randomization and intervention
During the treatment period (Day 0 to month 5), patients in Group 1 (4 mg/kg, low-dose group) and Group 2 (8 mg/kg, high-dose group) received intravenous (IV) infusions of TCZ on days 0, 30, 60, 90, 120 and 150. During the follow-up period (month 6 to 12), treatment was optional and administered only if patients qualified for treatment based on re-treatment criteria.
Fluorescein angiography analysis for posterior segment inflammatory outcomes
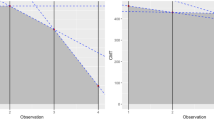
The ASUWOG fluorescein angiography scoring system was used to determine the inflammatory scores in the study eyes at baseline and Month 6. This scoring system assigns scores to various inflammatory signs on FA with a maximum total score of 40 (Table 1). Two independent certified graders assessed the images at a central reading center, the Ocular Imaging Research and Reading Center (OIRRC, Sunnyvale, CA). The graders were masked to both the timepoint and treatment when scoring images. A senior grader adjudicated any discrepancies between the two graders. Figure 1 provides representative FA images of a patient at the baseline and month 6 visit.
Outcome measures
Mean change in posterior segment inflammation as assessed using the FA inflammatory score, from baseline to month 6, in the two study groups.
Statistical analysis
As the STOP-Uveitis study was an exploratory, pilot phase 1/2 study, the sample size was not chosen based on statistical calculation. The sample size per dose group was chosen based on clinical judgment; it was estimated that approximately 18 subjects in each group may be able to provide initial information regarding the safety and efficacy of TCZ infusions in patients with uveitis. Non-parametric tests were used to analyze the data. Quantitative data was analyzed for significance within groups using Wilcoxon Signed Rank test and between groups using Mann Whitney U test. Stata V14.1 (Stata Corp, TX) was used for all statistical analyses. Statistical significance was set at p < 0.05.
Results
A total of 37 patients were enrolled in the STOP-Uveitis study. Baseline demographic characteristics of the two study groups have been reported previously and are shown in Table 2. Out of 37 patients, 30 patients (30 eyes) were included in this sub-study analysis based on the inclusion and exclusion criteria. Seven subjects (7 eyes) had ungradable FA images and were therefore excluded from the study.
Fluorescein angiography inflammatory outcomes
Table 3 shows the median changes in the FA inflammatory scores from baseline to month 6 in the study groups. At month 6, the overall (groups combined) median FA inflammatory score improved from 6.00 ± 3.26 (median ± SD/standard deviation) at baseline to 2.00 ± 3.40 at month 6 (p = 0.0006). The median FA inflammatory score in group 1 decreased from 7.50 ± 3.56 at baseline to 2.00 ± 4.05 at month 6 (p = 0.019). Similarly, the median FA inflammatory score decreased from 5.50 ± 2.67 at baseline to 2.00 ± 2.50 at month 6 in group 2 (p = 0.013). The difference in median improvement of FA inflammatory score between the two study groups was not statistically significant (p > 0.05).
All 30 patients analyzed in the study had an inflammatory score greater than 0 at baseline, suggesting some degree of posterior segment inflammation at baseline. Table 4 demonstrates the percentage of patients in each group that showed improvement, worsening or no change in FA inflammatory scores at month 6. 25 patients (83.3%) showed an improvement, three patients (10%) showed worsening and two (6.6%) showed no change in the inflammatory score at month 6. There was no significant difference in the percentage of patients that showed improvement in the inflammatory scores at month 6 between the two study groups. All three patients that showed worsening in the inflammatory score did so due to a 1-point increase in capillary leakage at the month 6 visit.
Discussion
There are several therapeutic agents that are currently being investigated for NIU. However, adalimumab is the only current food and drug administration (FDA) approved non-corticosteroid therapy for adults with non-infectious uveitis. Tocilizumab (TCZ) is a novel recombinant monoclonal antibody directed against IL-6 receptors. It is currently used as an off-label therapy for patients with refractory uveitis and ocular inflammatory diseases. We have previously reported favorable outcomes of patients with NIU treated with TCZ in the STOP-Uveitis study [2, 13]. These included a statistically significant improvement in BCVA, CRT and vitreous haze.
The standardization of uveitis nomenclature vitreous haze score (SUN-VH) is currently the most frequently used parameter for grading of posterior segment inflammation in clinical trials. It relies on the subjective assessment of fuzziness of the posterior segment as assessed using indirect ophthalmoscopy. However, given the significant variability of patients with NIU, many patients may present with significant visual morbidity without the accompanying vitreous haze [14, 15]. In addition, a significant number of patients may not present with a vitreous haze score high enough to demonstrate a 2-step improvement during the study. It is also often challenging to recruit patients with at least 2 + vitreous haze. In the STOP-Uveitis study, patients were defined as having active uveitis and were included in the study if they had vitreous haze greater than or equal to 1 at baseline. A 2-step improvement in the VH score was achieved by 32.3% (10 out of 37) subjects in the STOP-Uveitis study. Only 23 out of 37 subjects initially enrolled had the potential for a 2-step improvement in VH, which suggested that the actual 2-step improvement in patients that had the potential for 2-step improvement in VH was 43.3%. Therefore, assessment of disease activity and progression in patients with NIU cannot be reliably assessed using VH alone.
To overcome this challenge, we used a semi-quantitative FA scoring system to report the posterior segment inflammatory outcomes in these patients. Fluorescein angiography (FA) is a commonly used imaging modality in patients with posterior segment disease. However, given the qualitative mode of assessment and variability in grader assessment, it has not been frequently used to report large-scale data in patients with NIU. Therefore, the role of FA as a reliable disease marker in clinical trials has not realized its fullest potential. We used a novel FA scoring system proposed by the ASUWOG group, which is a semi-quantitative scoring system that was initially proposed in 2008, to evaluate both the severity and extent of posterior segment inflammation in patients with NIU. In this index study, we report improved posterior segment inflammatory outcomes in patients with NIU treated with TCZ at the month 6 visit. Both the low-dose and high-dose groups showed a significant reduction in inflammatory scores.
A reliable scoring system in patients with uveitis has several advantages: it can help support the diagnosis; reduce personal bias, improve assessment during follow-up visits and communication between physicians, and allow an objective way of analyzing data for clinical trials. The FA scoring system reported by the ASUWOG group has been utilized in multiple studies previously [6, 10]. Mantovani et al. [12] studied the inter-observer variability in the ASUWOG scoring system. The study concluded that the ASUWOG scoring system is a reliable method for assessing degree of ocular inflammation. Kang et al. [16] also utilized the ASUWOG FA scoring system to study patients with Adamantiades-Bechet’s disease patients for long-term progression of retinal vasculitis, an essential feature of the disease. Using this scoring system, they were able to show that there is no significant difference in the degree of inflammation between the first episode and subsequent flares in the patients. Furthermore, they also demonstrated that there is a significant difference in inflammatory signs between the active and quiescent phases of the disease.
All 30 patients analyzed in this study had a baseline inflammatory score greater than 0, suggesting some degree of inflammation at baseline. 83% of these patients showed improvement in the inflammatory scores at month 6. Two patients demonstrated no change in the inflammatory scores and three patients showed worsening. All three patients that showed worsening had a 1-point increase in the inflammatory scores attributed to mild worsening of macular leakage at month 6. None of these three patients that showed worsening in the inflammatory scores demonstrated a visual decline. This finding reiterates the importance of using the FA inflammatory score in combination with other clinical parameters to make accurate assessments regarding disease management.
We assessed the correlation between the changes in the FA inflammatory score, BCVA and CRT during the study and found only a weak correlation between these study variables. This finding re-emphasizes again the importance of analyzing all outcome measures in combination. Non-infectious uveitis is a group of diseases that often shows great variability in disease presentation and the underlying pathological processes involved may be significantly different. Assessment using FA will only add to the armamentarium at our disposal for accurate assessment and follow up of patients with NIU, and caution must be exercised when using it in isolation for management decisions. A composite scoring system utilizing all modes of assessment including BCVA, CRT, FA inflammatory score, and VH for example, may be more helpful in improving the accuracy and reliability of assessments in these patients.
The strengths of our study include the mandatory monthly treatment design and well-characterized study population of a multicenter clinical trial. Previous studies of TCZ have largely been limited to case reports and short case-series. All images were graded at a central reading center in a controlled environment. In addition, we used a previously verified semi-quantitative scoring system for assessment of posterior segment inflammatory outcomes in our study.
The mean FA inflammatory score at baseline was 6.00 ± 3.26, suggesting a low-grade of posterior segment inflammation at baseline. This may either suggest a low sensitivity of the scoring system for detecting posterior segment disease or more likely that the patients did not have significant posterior segment inflammatory findings at baseline. In the STOP-Uveitis study patients with active uveitis were enrolled in the study. Active uveitis was defined as the presence of ≥ 1 vitreous haze at baseline. The presence of other posterior segment inflammatory findings was therefore not necessary at baseline, which may explain the relatively low baseline FA inflammatory score.
Possible limitations of our study include the relatively small sample size, post-hoc nature of analysis, and the short duration of follow-up. Data from seven patients in the study (18.9%) could not be utilized for this sub study analysis due to the presence of ungradable images at either baseline or at month 6. In addition, the study was not statistically powered to compare the efficacy of the two doses and to assess the efficacy among the different causes of uveitis in the study.
Conclusions
Our study reports that monthly infusions of tocilizumab significantly improve posterior segment inflammatory outcomes in patients with non-infectious uveitis. Fluorescein angiography analyses using an objective scoring system may be employed for assessment of posterior segment inflammation in these patients. We propose employing such scoring methods in combination with other outcome measures, to help uveitis specialists make reliable management decisions in patients with non-infectious uveitis.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASUWOG:
-
Angiography Scoring for Uveitis WOrking Group
- BCVA:
-
Best corrected visual acuity
- CRT:
-
Central retinal thickness
- FA:
-
Fluorescein angiography
- IV:
-
Intravenous
- NIU:
-
Non-infectious uveitis
- SUN:
-
Standardization of uveitis nomenclature
- TCZ:
-
Tocilizumab
- VH:
-
Vitreous haze
References
Miserocchi E, Fogliato G, Modorati G, Bandello F. Review on the worldwide epidemiology of uveitis. Eur J Ophthalmol. 2013;23(5):705–17.
Sepah YJ, Sadiq MA, Chu DS, Dacey M, Gallemore R, Dayani P, et al. Primary (month-6) outcomes of the STOP-uveitis study: evaluating the safety, tolerability, and efficacy of tocilizumab in patients with noninfectious uveitis. Am J Ophthalmol. 2017;183:71–80.
Ben Ezra D, Forrester JV, Nussenblatt RB, Tabbara K, Timonen P. Uveitis scoring system. Uveitis Scoring System. Berlin: Springer; 1991. p. 1–2.
van Kooij B, Fijnheer R, de Boer J, ten Dam-van LN, Bartelink I, Roest M, et al. A randomized, masked, cross-over trial of lisinopril for inflammatory macular edema. Am J Ophthalmol. 2006;141(4):646–51.
Tugal-Tutkun I, Herbort CP, Khairallah M, Group TASfUW. Scoring of dual fluorescein and ICG inflammatory angiographic signs for the grading of posterior segment inflammation (dual fluorescein and ICG angiographic scoring system for uveitis). Int Ophthalmol. 2010;30(5):539–52.
Tugal-Tutkun I, Herbort CP, Khairallah M. Scoring of dual fluorescein and ICG inflammatory angiographic signs for the grading of posterior segment inflammation (dual fluorescein and ICG angiographic scoring system for uveitis). Int Ophthalmol. 2010;30(5):539–52.
El Ameen A, Herbort CP. Comparison of retinal and choroidal involvement in sarcoidosis-related chorioretinitis using fluorescein and indocyanine green angiography. J Ophthalmic Vision Res. 2018;13(4):426–32.
Gillmann K, El Ameen A, Massy R, Fabro F, Gasc A, Herbort CP Jr. Assessment of measurement methods of posterior inflammation in stromal choroiditis: the value of quantitative outcome measures versus the presently qualitatively based paradigm. Int Ophthalmol. 2019;39(7):1567–74.
Fabro F, Herbort CP. Need for quantitative measurement methods for posterior uveitis: comparison of dual FA/ICGA angiography, EDI-OCT choroidal thickness and SUN vitreous haze evaluation in stromal choroiditis. Klin Monatsbl Augenheilkd. 2018;235(4):424–35.
Balci O, Jeannin B, Herbort CP Jr. Contribution of dual fluorescein and indocyanine green angiography to the appraisal of posterior involvement in birdshot retinochoroiditis and Vogt-Koyanagi-Harada disease. Int Ophthalmol. 2018;38(2):527–39.
Massy R, Herbort CP. Contribution of dual fluorescein and indocyanine green angiography to the appraisal of presumed tuberculous chorioretinitis in a non-endemic area. J Ophthalmic Vision Res. 2017;12(1):30–8.
Tugal-Tutkun I, Herbort CP, Khairallah M, Mantovani A. Interobserver agreement in scoring of dual fluorescein and ICG inflammatory angiographic signs for the grading of posterior segment inflammation. Ocul Immunol Inflamm. 2010;18(5):385–9.
Hassan M, Nguyen NV, Halim MS, Afridi R, Sadiq MA, Karkhur S, et al. Effect of vitreomacular adhesion on the treatment outcomes in the STOP-Uveitis clinical trial for non-infectious uveitis. J Ophthalmic Inflamm Infect. 2019;9(1):12.
Selmi C. Diagnosis and classification of autoimmune uveitis. Autoimmun Rev. 2014;13(4–5):591–4.
Seve P, Cacoub P, Bodaghi B, Trad S, Sellam J, Bellocq D, et al. Uveitis: diagnostic work-up. A literature review and recommendations from an expert committee. Autoimmun Rev. 2017;16(12):1254–64.
Kang HM, Lee SC. Long-term progression of retinal vasculitis in Behcet patients using a fluorescein angiography scoring system. Graefe's Arch Clin Exp Ophthalmol. 2014;252(6):1001–8.
Acknowledgements
The STOP-Uveitis study team.
Meeting presentation: The manuscript was presented orally in part at the 2018 American Academy of Ophthalmology (AAO) Congress, Chicago, Illinois, USA.
Funding
The Study was conducted under an Investigative New Drug (IND) granted by the FDA to Dr. Nguyen. The study drug (tocilizumab) was provided by Genentech.
Author information
Authors and Affiliations
Consortia
Contributions
MAS and QDN—Study design, data analysis/interpretation and manuscript preparation. MH, YJS, DVD, SH, RA—study design, data analysis and interpretation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate and publish
The study was conducted in compliance with the United States Code of Federal Regulations Title 21, the Declaration of Helsinki, and the Harmonized Tripartite Guidelines for Good Clinical Practice (1996). The study was approved by local institutional review boards for selected sites and by a central review board for others. Signed informed consent were obtained from all the participants in the study.
Consent for publication
Not applicable.
Competing interests
YJS has received research support from Astellas, Genentech, and Optovue, and serves on the Scientific Advisory Board for Genentech/Roche, Optos, and Regeneron. QDN serves on the Scientific Advisory Board for AbbVie, Bayer, Genentech, Regeneron, and Santen, among others. QDN also chaired the Steering Committee for the STOP-Uveitis Study and was on the Steering Committee for other studies sponsored by Genentech and Regeneron. DVD serves on the Scientific Advisory Board for Allergan, Genentech, Kodiak, Regeneron, and Santen and she has received research support from Genentech and Regeneron. No other authors have received any financial funding or support.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sadiq, M.A., Hassan, M., Afridi, R. et al. Posterior segment inflammatory outcomes assessed using fluorescein angiography in the STOP-UVEITIS study. Int J Retin Vitr 6, 47 (2020). https://doi.org/10.1186/s40942-020-00245-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40942-020-00245-w