Abstract
Background
To date, the association of serum macrophage migration inhibitory factor (MIF) and serum adipokines with lupus nephritis is controversial.
Objective
To assess the utility of serum MIF, leptin, adiponectin and resistin levels as markers of proteinuria and renal dysfunction in lupus nephritis.
Methods
Cross-sectional study including 196 systemic lupus erythematosus (SLE) patients and 52 healthy controls (HCs). Disease activity was assessed by Systemic Lupus Erythematosus Disease Activity Index (SLEDAI). Renal SLE involvement was investigated by renal-SLEDAI. MIF, adiponectin, leptin and resistin levels were quantified by ELISA. We assessed the correlations of quantitative variables by Spearman correlation (rs). Multivariable linear regression adjusted the variables associated with the severity of proteinuria.
Results
SLE patients had higher MIF (p = 0.02) and adiponectin (p < 0.001) than HCs. Patients with renal SLE involvement (n = 43) had higher adiponectin (19.0 vs 13.3 μg/mL, p = 0.002) and resistin (10.7 vs 8.9 ng/mL, p = 0.01) than patients with non-renal SLE (n = 153). Proteinuria correlated with high adiponectin (rs = 0.19, p < 0.009) and resistin (rs = 0.26, p < 0.001). MIF (rs = 0.27, p = 0.04). Resistin correlated with increased creatinine (rs = 0.18, p = 0.02). High renal-SLEDAI correlated with adiponectin (rs = 0.21, p = 0.004). Multiple linear regression showed that elevated adiponectin (p = 0.02), younger age (p = 0.04) and low MIF (p = 0.02) were associated with the severity of proteinuria. Low MIF and high adiponectin levels interacted to explain the association with the severity of proteinuria (R2 = 0.41).
Conclusions
High adiponectin combined with low MIF concentrations int+eract to explain the severity of proteinuria in renal SLE. These findings highlight the relevance of adiponectin, resistin and MIF as markers of LN.
Similar content being viewed by others
Background
Systemic lupus erythematosus (SLE) is considered a chronic inflammatory autoimmune disorder characterised by an extensive spectrum of inflammation in organs and tissues, with the kidneys being one of the main organs affected by the disease. The cumulative incidence of renal involvement in SLE is 54%, and it has a prevalence that varies from 30 to 80% [1, 2]. Lupus nephritis (LN) is associated with significant morbidity and mortality, with an incidence of end-stage renal disease (ESRD) of 27.6 per 1000 patient-years, although this pattern can differ depending on race [3]. For instance, Hispanic patients have a high predisposition to LN, similar to that of Asian and African American populations and higher than that of Caucasians [4]. One of the main strategies to detect patients at risk of LN is using clinical markers. Traditional markers of LN, such as increased native double-stranded DNA antibody (anti-dsDNA) and decreased C3 and C4 complement fractions, are currently used in the clinical assessment of LN [5]; however, these markers do not appear to have sufficient sensitivity for detecting LN in a subgroup of SLE patients, thus, new non-traditional markers should be tested [6]. Among these other markers of LN are included the serum levels of adipokines and cytokines. These molecules have been associated with the parameters of renal involvement, such as proteinuria, decrease in glomerular filtration rate, impairment of creatinine clearance, haematuria, and increase in urinary leucocytes or casts [7,8,9,10]. Nevertheless, some cytokines and adipokines such as the serum levels of the macrophage migration inhibitory factor (MIF), leptin, adiponectin and resistin have been insufficiently evaluated as markers in LN. MIF is a pleiotropic cytokine with a wide variety of proinflammatory and immunomodulatory functions, including the regulation of the inflammatory response mediated by T-cells [11, 12]. Although MIF is constitutively expressed in many tissues, in the kidneys, it can be expressed mainly by glomerular epithelial cells and cortical tubules [13]. Experimental models of glomerulonephritis have shown an upregulation of renal mRNA MIF, leading to the overexpression of MIF [14]. In models of kidney damage, the overexpression of MIF in podocytes induces progressive injury to these cells and progression to glomerulosclerosis [15]. In SLE patients, the participation of MIF in the disease activity of SLE has been investigated by a few studies. Tu et al. found an increase in the serum MIF levels in SLE patients compared with controls, and MIF levels correlated with the severity of disease activity measured by the Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) [16]. Moreover, to date the relevance of MIF in LN has been infrequently evaluated, assessed mainly in relationship with MIF urinary concentrations [17, 18]. Some authors have examined the association between urinary MIF levels and proteinuria. Brown et al. did not observe a relationship between serum or urinary MIF levels and the amount of proteinuria [17]. However, these authors identified an increase in urinary MIF only in patients with proliferative nephritis [17]. On the other hand, Vincent et al. did not identify correlations between urinary MIF and nephritis in SLE patients, although high concentrations of urinary MIF were related to high disease activity in these patients [18]. In the clinical context, the presence and severity of proteinuria is a key variable to suspect LN, and it has been included as one of the items described in the renal-SLEDAI to identify renal disease activity [19]. Proteinuria is not only a clinical marker for LN but also recognised as a major prognostic factor of ESRD [20]. Therefore, the correlation between serum MIF levels and proteinuria requires a more detailed assessment.
Nowadays, there is some evidence supporting that MIF expression can be related with certain adipokines. For instance, Koska et al. observed that the mRNA expression of MIF in adipocytes is negatively associated with the levels of adiponectin [21]. However, currently, there is a lack of information regarding the relation between serum MIF levels and adipokines in LN, and it has not been determined whether the association observed between adipokines and renal flare in SLE is independent of MIF levels.
In LN, some adipokines, such as leptin, resistin and adiponectin, have been investigated with discordant results. For instance, Hutcheson et al. found that adiponectin concentrations decrease with the increase in disease activity [8], whereas our group observed a positive correlation between high adiponectin levels and the severity of proteinuria [11].
In consequence, there are insufficient data regarding the possible role of MIF and adipokines levels as markers of renal involvement in SLE patients. Therefore, we decided to assess the value of serum MIF, leptin, adiponectin and resistin levels as markers of proteinuria and renal dysfunction in LN.
Methods
Study design
We conducted a cross-sectional study of female patients with SLE. These patients met the following inclusion criteria: a) a diagnosis of SLE as corroborated by a rheumatologist; b) met the 1982 American College of Rheumatology criteria of SLE [22]; c) age ≥ 18 years; d) ethnicity of Mexican-Mestizos [23]; and e) disease duration of at least 1 year since the first symptom. We excluded patients with overlap syndrome, pregnancy, active infection, and diseases other than SLE that might produce abnormal proteinuria.
Clinical setting
All patients were selected from the lupus cohort of an outpatient rheumatology clinic of one largest secondary-care centres in Guadalajara, Mexico (Hospital General Regional 110, Instituto Mexicano del Seguro Social [IMSS]).
A healthy controls (HCs) group of 52 females matched by age and ethnicity were selected. These controls were clinically healthy subjects recruited from patients visiting the Department of Preventive Medicine for check-ups at the same hospital. HCs were included to compare the values of MIF and adipokines with those of the SLE patients.
Clinical evaluations
Three trained rheumatologist researchers assessed the SLE patients using a structured chart, including disease features, comorbid diseases, and current pharmacological treatment. Assessment of disease damage: This was investigated using the Systemic Lupus International Collaborating Clinics/American College of Rheumatology (SLICC/ACR) damage index [24]. Assessment of disease activity: This assessment was performed using the Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) [19]. The SLEDAI is an index designed to assess disease activity in the preceding 10 days, with 24 weighted clinical and laboratory variables corresponding to 9 different organs/systems. The SLEDAI score ranges from 0 to 105. Renal activity was evaluated with the renal-SLEDAI (rSLEDAI) [19], which represents the sum of the renal items of the SLEDAI. The rSLEDAI includes the following items: proteinuria, pyuria, erythrocyturia, and urine casts; each one is scored with 0 meaning absence or 4 points meaning presence; therefore, the maximum rSLEDAI is 16 [19]. The main criterion of renal activity was proteinuria greater than 0.5 g/day or in conjunction with any of the following features: persistent haematuria, leucocytes in urine or urine casts by granulocytes or erythrocytes (excluding other causes). SLE patients with these features were classified as the renal SLE group, and this group was compared with the non-renal group, which consisted of SLE patients that did not meet any criteria of the rSLEDAI. We used the Mexican version of the SLEDAI (MEX-SLEDAI) [25]. The MEX-SLEDAI is an adaptation of the SLEDAI that does not include laboratory immunological parameters such as complement fraction and anti-dsDNA [25]. The MEX-SLEDAI score ranges from 0 to 32.
MIF and adipokine measurements
Blood samples were extracted from SLE patients and HCs at the time of clinical evaluation. Samples were stored at room temperature for 30 min after sampling. Then, the samples were centrifuged at 1300×g for 15 min at 4 °C. Serum samples were stored at − 80 °C without freeze-thaw cycles for a maximum of 6 months. All serum samples were coded before the measurements. This strategy was made to blind the researchers who assessed the clinical characteristics to the MIF and adipokine results, minimising the risk of measurement bias. Serum MIF levels were quantified using a commercial ELISA kit (R&D™, Minneapolis, USA). The sensitivity of this assay was 0.068 ng/mL. Measurements of adipokines, including leptin (sensitivity of 7.8 pg/mL), adiponectin (sensitivity of 0.89 ng/mL), and resistin (sensitivity of 0.055 ng/mL), were performed using commercial ELISA kits (R&D™, Minneapolis, USA). If required, we performed a serum sample dilution in cases with values above the highest point on the standard curve. All ELISAs were performed according to the manufacturer’s instructions. All samples were run in duplicate to improve assay precision.
Statistical analysis
Quantitative variables are described as medians (ranges), and qualitative characteristics are described as frequencies (%). The chi-square test (or Fisher’s exact test) was used for comparisons between proportions. Comparisons of quantitative variables between the renal-SLE and non-renal groups were performed using the Mann-Whitney U test. To compare the differences in quantitative variables among the three groups (renal SLE, non-renal SLE, and HCs), we used the Kruskal-Wallis test. In this analysis, p-values for multiple comparisons were adjusted by Bonferroni correction. To identify the correlations between MIF, adipokines and other clinical variables, Spearman’s test was performed. Multiple regression analysis was used (stepwise method) to identify variables associated with proteinuria (g/day). In this model, variables with biological plausibility and statistical significance (p < 0.20) in univariate analysis were introduced as covariables.
We further explored the possible interaction effect of MIF and adipokines. For this proposed interaction, we constructed individual regression models. Before the construction of interaction models, we first evaluated the collinearity between MIF and adipokines and their product term. We used the mean centring method for testing interactions as described below [26, 27]. In brief, for each of the tested predictor variables, the mean was subtracted before testing the products to represent their interaction. Then, models of the interactions of multiplicative terms were tested for each of the transformed variables (correcting for MIF and adipokines). We used SPSS Statistics for Windows (Version 25.0, IBM Corp., Armonk, NY) and R version 4.0.0 [28] to perform the statistical analyses. Figures were constructed in R using the ggplot2 package [29]. A p-value ≤ 0.05 was considered statistically significant.
Results
Comparison of healthy controls and SLE patients
This study included 196 SLE patients and 52 HCs. Table 1 shows comparisons of the clinical variables between the SLE and HCs groups. All SLE patients and HCs were females and Mexican-Mestizo. SLE patients had a similar median age compared with HCs (45 vs 47 years, p = 0.87). Body mass index (BMI) was not significantly different between the SLE and HCs groups (27.3 vs 27.9, p = 0.86).
Characteristics of the SLE patients
Table 1 also includes a description of the selected characteristics of the total group of SLE patients. Of 196 SLE patients, 28.1% had positive anti-dsDNA antibodies. The median SLEDAI score was 2 points. Seventy-six (38.8%) SLE patients had active disease (SLEDAI> 4). The r-SLEDAI ranged from 0 to 12 points. Forty-three SLE patients (21.9%) presented renal disease activity. All SLE patients were receiving glucocorticoids, although only 60 (30.6%) were receiving a dosage > 10 mg/day. Of the total SLE patients, 74% were receiving immunosuppressive therapy.
Comparison of MIF and adipokine levels between SLE and HCs
Figure 1 presents the comparison of MIF and adipokine levels between the SLE and HCs groups. Serum MIF and adiponectin concentrations were higher in SLE patients than in HCs. Increased MIF levels were observed in SLE patients [9.1 (0.6–43.9) ng/mL vs. 5.3 (0.3–32.7) ng/mL, p = 0.02]. Adiponectin concentrations were also higher in SLE patients than in HCs [14.5 (0.6–45.1) μg/mL vs 10.2 (1.6–24.3) μg/mL, p < 0.001]. Resistin levels were lower in SLE patients than in HCs [9.1 (2.4–37.1) ng/mL vs 14.3 (1.3–55.9) ng/mL], p < 0.001). No differences were identified in the concentrations of leptin between SLE patients and HCs [18.6 (1.6–136.5) ng/mL vs 18.3 (0.31–87.48) ng/mL, p = 0.92].
Comparison of MIF and adipokine levels in HCs, renal SLE and non-renal SLE
Figure 2 shows the comparison of the MIF and adipokine levels among the HCs, renal SLE and non-renal SLE groups. The three groups had differences in adiponectin levels (p < 0.001). Post hoc analysis showed that adiponectin concentrations were more elevated in renal SLE patients than in HCs [19.0 (7.3–45.1) μg/mL vs 10.2 (1.6–23.4) μg/mL, p < 0.001] and non-renal SLE patients [19.0 (7.3–45.1) μg/mL vs 13.3 (0.6–37.0) μg/mL, p = 0.002]. Non-renal SLE patients presented higher levels of adiponectin than HCs [13.3 (0.6–37.0) μg/mL vs 10.2 (1.6–23.4) μg/mL, p = 0.002]. Resistin concentrations were more elevated in HCs than in non-renal SLE patients [14.3 (1.3–55.9) ng/mL vs 8.9 (2.5–37.1) ng/mL, p < 0.001] and renal SLE patients [14.3 (1.3–55.9) ng/mL vs 10.7 (6.2–26.2) ng/mL, p < 0.001]. MIF and leptin levels were not significantly different among the three groups.
Comparison of MIF and adipokines in HCs, renal SLE, and non-renal SLE. HCs: healthy controls. SLE: Systemic lupus erythematosus. Renal SLE includes patients with proteinuria higher than 0.5 g/day as the sole criterion or in conjunction with persistent haematuria, leucocytes in urine or urine casts by granulocytes or erythrocytes. Comparisons between quantitative variables were performed with the Kruskal-Wallis test. p < 0.05. P values for multiple comparisons were adjusted by Bonferroni correction. ns: p > 0.05. *p < = 0.05, **p < = 0.01, ***p < = 0.001, ****p < = 0.0001
Comparison of variables between renal SLE and non-renal SLE
Renal SLE patients received higher doses of prednisone than patients without renal activity [20 (2.5–75) mg/day vs 7.5 (2.5–50.0) mg/day, p < 0.001], but the frequency of the concurrent use of immunosuppressive drugs was similar in renal SLE and non-renal SLE patients (p = 0.64). Furthermore, renal SLE and non-renal SLE patients had similar disease durations [43 (18–62) years vs 46 (18–73) years, p = 0.13]. Other comparisons of variables between renal SLE patients and non-renal SLE patients are described in Table 2.
Correlations of MIF and adipokines with clinical variables
Table 3 describes the correlations of MIF and adipokines with clinical and laboratory variables. Lower serum MIF levels were correlated with increased age (p = 0.003) and longer duration of SLE (p = 0.004). MIF did not correlate with SLEDAI, rSLEDAI, proteinuria or other features. Serum leptin levels correlated with BMI (p < 0.001), proteinuria (p = 0.01) and estimated glomerular filtration rate (eGFR) (p = 0.02). High concentrations of adiponectin correlated with proteinuria (p = 0.009), rSLEDAI (p = 0.004), and high Mex-SLEDAI scores (p = 0.03). However, adiponectin levels were negatively correlated with eGFR (p = 0.05). Additionally, serum adiponectin levels correlated with glucocorticoid dose (p = 0.02) and BMI (p < 0.001). Correlations were observed between resistin levels and proteinuria (p < 0.001), serum creatinine (p = 0.02), SLICC/ACR (p = 0.01), and glucocorticoid dose (p = 0.03). No correlations were observed between serum leptin or resistin and proteinuria, SLEDAI or rSLEDAI.
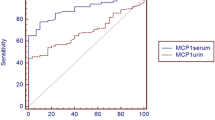
Correlations of MIF and adipokines with parameters of renal activity in the 43 renal SLE patients
We investigated the correlations of MIF and adipokine levels with parameters of renal activity in renal SLE patients. MIF levels were significantly correlated with proteinuria in g/day (rs = − 0.47; p = 0.008) but not with serum creatinine (rs = − 0.24; p = 0.13), 24-h creatinine clearance (rs = − 0.14; p = 0.40), or eGFR (rs = 0.15; p = 0.33). Furthermore, in renal SLE patients, adiponectin levels correlated only with serum creatinine (rs = 0.34; p = 0.03) but not with other parameters of renal activity. Resistin and leptin did not show any correlations with renal inflammatory features (data not shown).
Variables associated with the severity of proteinuria (g/day): results of the multiple linear regression analysis
Table 4 demonstrates the findings of the factors associated with the severity of proteinuria in g/day obtained in the multiple linear regression analysis. With the enter method, the variables associated with the severity of proteinuria (g/day) were glucocorticoid dose (p < 0.001), adiponectin level (p < 0.001), MIF level (p = 0.01) and age (p < 0.001). Using the forward stepwise method in multivariable linear regression analysis, the factors associated with the severity of proteinuria in g/day were higher glucocorticoid doses (p < 0.001), higher adiponectin levels (p = 0.001), lower MIF levels (p = 0.005) and younger age (p = 0.011). This model was adjusted by glucocorticoid dose, immunosuppressive therapy, disease duration, age, and MIF, adiponectin, leptin, and resistin levels. The R2 and adjusted R2 of this model were 0.41 and 0.40, respectively.
We tested for interactions in the multiple regression analysis to assess weighted variables associated with the amount of proteinuria (data not shown). After testing for interactions, we identified an interaction between age and adiponectin levels as well as an interaction of serum MIF and adiponectin levels with the amount of proteinuria in SLE patients. In the interaction model, higher adiponectin levels and higher age increased proteinuria levels. Lower MIF levels interacted with higher adiponectin levels to increase proteinuria. The adjusted R2 of the final interaction model was 0.41 with p < 0.001.
Discussion
In the bivariable analysis, an increase in the levels of the three adipokines (adiponectin, leptin and resistin) correlated with the severity of proteinuria. In the multivariable analysis, we identified an interaction between adiponectin and MIF levels, suggesting that high adiponectin levels combined with low concentrations of MIF is associated with the severity of proteinuria in LN. On the other hand, in the examination of renal dysfunction, we found that high MIF and resistin levels were correlated with an increase in serum creatinine in the entire SLE group. However, when we examined exclusively the subgroup of SLE with proteinuria, MIF and resistin concentrations did not remain correlated with serum creatinine, whereas resistin was also not correlated with eGFR when examined in the LN subgroup.
In this work, we evaluated proteinuria as the main surrogate variable of LN. Proteinuria is an important biological marker in LN, and proteinuria > 3.5 g/day is a risk factor for ESRD [20]. Patients with persistent proteinuria develop chronic renal disease with an increase in fibrosis in the renal tubules and renal interstitium [30]. MIF concentrations were related to a decrease in proteinuria in renal SLE, and this relationship remained in the multivariable analysis after adjusting for confounders. These findings are different from the previously published. Brown et al. identified an increase in urinary MIF that was observed only in proliferative nephritis, whereas no association was detected between serum or urinary MIF levels and the amount of proteinuria [17]. Vincent et al. found no associations between urinary MIF levels and LN, although elevated urinary MIF was observed in SLE patients with high disease activity [18]. These results suggest that the relation of MIF with the presence of LN is complex and requires an assessment of possible interactions with other molecules, including adipokines that could be associated with LN. MIF is a pleiotropic cytokine inducer of the synthesis of TNF-α and IL-6; additionally, MIF is a modulator of the inflammatory response, regulating T-cell proliferation [11]. In vivo studies have shown that MIF can abrogate the anti-inflammatory effect of glucocorticoids [31]. Studies in animal models demonstrate that blocking MIF induces a protective effect against inflammation in adjuvant-induced arthritis [32]. MIF can antagonise the immunosuppressive effect of glucocorticoids [33]. However, to date, it is not clear whether immunosuppressive treatments might modify MIF levels, whereas it has been suggested that TNF-α or IFN-γ might increase the release of MIF [34]. Instead, in our study no correlations were observed between MIF or leptin levels with glucocorticoids dose.
On the other hand, MIF concentrations correlated with an increase in serum creatinine only in the entire group of SLE patients but not in patients with renal activity. These data generate new questions regarding whether MIF could be a marker of renal dysfunction but not a marker of renal inflammation. Our findings are supported by the results observed by Otukesh et al., who identified a higher MIF/creatinine ratio in paediatric patients with LN than in those without LN [35].
In our study, high adiponectin levels were correlated with an increase in proteinuria. Nevertheless, many confounders can influence these results. Therefore, we performed a multivariable analysis, including those confounding variables that might affect the results. After this analysis, adiponectin levels remained a factor associated with proteinuria. Although we tested other adipokines in the present study, only adiponectin remained associated with the severity of proteinuria in SLE. These findings might reflect that adiponectin levels are a risk factor for proteinuria; nevertheless, these findings can also reflect an increase in adiponectin as a result of renal inflammation, with high serum levels acting as a potential protective homeostatic mechanism. An experimental study performed in cell cultures suggests that adiponectin can protect against the development of chronic renal disease by decreasing reactive oxygen species, local renal inflammation and fibrosis [36]. Another experimental study performed in cultured podocytes showed that the adiponectin regulation of inflammation could be mediated through the stimulation of AMP-activated protein kinase (AMPK) and a decrease in NADPH oxidase [37]. These experimental studies support our second hypothesis that adiponectin can have a role as anti-inflammatory molecule secreted in response to the stimuli of renal inflammation.
On the other hand, we observed a weak correlation between adiponectin and a decrease in eGFR, but we did not observe any correlation between adiponectin levels and an increase in serum creatinine. These findings are opposite to those observed by Hutchenson et al., who reported an association between adiponectin levels and renal dysfunction measured by serum creatinine [8]. However, our SLE patients had more disease activity than renal dysfunction, and the lack of a subgroup with very high levels of serum creatinine can influence the difference observed in our results.
Regarding the comparison between SLE and HCs groups. Our findings did not show differences in leptin between SLE and controls; instead, resistin was clearly increased in SLE patients compared with controls. Several publications have described increased levels of leptin and resistin in SLE patients [8, 38,39,40,41]. However, two different meta-analyses had opposite results regarding whether leptin levels are different in SLE vs controls [42, 43]. Regarding resistin, in a meta-analysis, Huang et al. did not identify differences between SLE patients and controls [44]. However, the heterogeneity of the characteristics of the SLE patients included in these meta-analyses can influence the variability of their results.
Finally, the findings of our study suggest that the relationship between adipokines and disease activity in SLE is more related with specific organs than a general increment of disease activity. We did not observe a correlation between the serum levels of leptin or resistin and disease activity measured by SLEDAI or MEX-SLEDAI. Our findings are supported by the results of the study performed by Santos et al., who did not identify an association of leptin or resistin with disease activity in SLE [45].
Regarding renal dysfunction and resistin levels, we found that serum resistin levels correlated with an increase in creatinine concentrations only in the entire group of SLE patients. Our findings were supported by the work performed by Hutcheson et al., who identified high resistin levels in SLE patients with renal dysfunction, including an increase in serum creatinine [8]. Nevertheless, we cannot conclude that resistin is a marker of renal dysfunction because in the subgroup of renal disease activity, the statistical significance of the correlations between resistin and serum creatinine or eGFR were lost.
To date, no previously published studies have evaluated the possible relation of serum adipokines with MIF levels in LN. Therefore, the present study was the first to assess a possible association of MIF and adipokines with proteinuria in SLE using a multivariable approach. Our findings support the interaction effect of serum levels of adiponectin and decreased MIF levels on proteinuria in SLE. The interaction that we observed between high adiponectin levels and lower MIF levels in patients with proteinuria secondary to LN might contribute to the identification of a different subgroup of patients with LN with more severe activity. However, it also allows us to formulate the question of whether our findings could reflect an adaptation mechanism involving increased adiponectin levels to limit renal damage in SLE nephritis and could be used to plan other therapeutic strategies.
There are some limitations in this work. First, the cross-sectional design represents only a snapshot of the complex relations of these inflammatory molecules with LN. Therefore, we ignored whether our findings of an increase in adiponectin together with a decrease in MIF levels might have occurred before the findings of renal relapse or if contrarily, adiponectin could have been increased after renal inflammation as an attempt to control the inflammatory process leading to low MIF levels. Follow-up studies are needed to solve this issue. Another limitation of our study was that the majority of our patients had a long SLE duration, and the characteristics of the cytokine and adipokine profiles might vary in patients with early SLE who develop nephritis. Additionally, a potential limitation of our study was that all of the SLE patients included were receiving treatment with glucocorticoids at the time of the study. We cannot exclude the effects associated with glucocorticoids on these molecules. An interesting observation published in the literature is that MIF is a cytokine that has been observed to decrease the effect of glucocorticoids [13]. Therefore, we ignored whether the MIF levels influenced the chain of events prior to the development of proteinuria in our SLE patients as a factor of corticosteroid resistance. Additionally, since glucocorticoids can increase the serum levels of some adipokines, further studies including a group of SLE patients prior to receiving glucocorticoids are needed to control for these confounders. Our results were derived from patients with SLE mainly with a long disease duration who were previously treated with glucocorticoids and immunosuppressive drugs, and a future study assessing LN patients with a recent diagnosis and measuring the molecules prior to starting immunosuppressive treatment is advised. Finally, a comparison of the serum levels of these analytes with urinary levels should be relevant to identify other associations. Future studies should take into account the importance of this comparison.
Conclusions
In conclusion, with a multivariable approach, higher adiponectin serum levels combined with low concentrations of MIF were found to be associated with proteinuria in LN. After excluding the effect of other adipokines or MIF, this interaction remained. Leptin and resistin levels correlated with proteinuria. This study raises a new hypothesis that the levels of these molecules together could play an essential role as markers in LN. However, longitudinal studies including SLE of recent onset are needed.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACR:
-
American College of Rheumatology
- BMI:
-
Body mass index
- anti-dsDNA:
-
Double-stranded DNA antibody
- eGFR:
-
Estimated glomerular filtration rate
- HCs:
-
Healthy controls
- LN:
-
Lupus nephritis
- MIF:
-
Macrophage migration inhibitory factor
- MEX-SLEDAI:
-
Mexican Systemic Lupus Erythematosus Disease Activity Index
- rSLEDAI:
-
Renal-SLEDAI
- rs :
-
Spearman rank correlation
- SLE:
-
Systemic lupus erythematosus
- SLEDAI:
-
Systemic Lupus Erythematosus Disease Activity Index
- SLICC/ACR:
-
Systemic Lupus International Collaborating Clinics/American College of Rheumatology
References
Borchers AT, Leibushor N, Naguwa SM, Cheema GS, Shoenfeld Y, Gershwin ME. Lupus nephritis: a critical review. Autoimmun Rev. 2012;12:174–94.
Bastian HM, Roseman JM, Mcgwin G, Alarcón GS, Friedman AW, Fessler BJ, et al. Systemic lupus erythematosus in three ethnic groups. XII. Risk factors for lupus nephritis after diagnosis. Lupus. 2002;11:152–60.
Plantinga L, Lim SS, Patzer R, McClellan W, Kramer M, Klein M, et al. Incidence of end-stage renal disease among newly diagnosed systemic lupus Erythematosus patients: the Georgia lupus registry: ESRD incidence in SLE patients. Arthritis Care Res. 2016;68:357–65.
Hanly JG, O’Keeffe AG, Su L, Urowitz MB, Romero-Diaz J, Gordon C, et al. The frequency and outcome of lupus nephritis: results from an international inception cohort study. Rheumatology Oxford. 2016;55:252–62.
Misra R, Gupta R. Biomarkers in lupus nephritis. Int J Rheum Dis. 2015;18:219–32.
Soliman S, Mohan C. Lupus nephritis biomarkers. Clin Immunol. 2017;185:10–20.
Adhya Z, Borozdenkova S, Karim MY. The role of cytokines as biomarkers in systemic lupus erythematosus and lupus nephritis. Nephrol Dial Transplant. 2011;26:3273–80.
Hutcheson J, Ye Y, Han J, Arriens C, Saxena R, Li Q-Z, et al. Resistin as a potential marker of renal disease in lupus nephritis: an adipokine marker in lupus nephritis. Clin Exp Immunol. 2015;179:435–43.
Chen D-Y, Chen Y-M, Wen M-C, Hsieh T-Y, Hung W-T, Lan J-L. The potential role of Th17 cells and Th17-related cytokines in the pathogenesis of lupus nephritis. Lupus. 2012;21:1385–96.
Diaz-Rizo V, Bonilla-Lara D, Gonzalez-Lopez L, Sanchez-Mosco D, Fajardo-Robledo NS, Perez-Guerrero EE, et al. Serum levels of adiponectin and leptin as biomarkers of proteinuria in lupus nephritis. PLoS One. 2017;12:e0184056. https://doi.org/10.1371/journal.pone.0184056.
Lang T, Foote A, Lee JPW, Morand EF, Harris J. MIF: implications in the Pathoetiology of systemic lupus Erythematosus. Front Immunol. 2015;6:577.
Lan HY. Role of macrophage migration inhibition factor in kidney disease. Nephron Exp Nephrol. 2008;109:e79–83. https://doi.org/10.1159/000145463.
Roger T, Chanson AL, Knaup-Reymond M, Calandra T. Macrophage migration inhibitory factor promotes innate immune responses by suppressing glucocorticoid-induced expression of mitogen-activated protein kinase phosphatase-1. Eur J Immunol. 2005;35:3405–13.
Lan HY, Yang N, Metz C, Mu W, Song Q, Nikolic-Paterson DJ, et al. TNF-alpha up-regulates renal MIF expression in rat crescentic glomerulonephritis. Mol Med. 1997;3:136–44.
Sasaki S, Nishihira J, Ishibashi T, Yamasaki Y, Obikane K, Echigoya M, et al. Transgene of MIF induces podocyte injury and progressive mesangial sclerosis in the mouse kidney. Kidney Int. 2004;65:469–81.
Tu Y, Guo R, Li J, Wang S, Leng L, Deng J, et al. MiRNA regulation of MIF in SLE and attenuation of murine lupus nephritis with miR-654. Front Immunol. 2019;10:2229. https://doi.org/10.3389/fimmu.2019.02229.
Brown FG, Nikolic-Paterson DJ, Hill PA, Isbel NM, Dowling J, Metz CM, et al. Urine macrophage migration inhibitory factor reflects the severity of renal injury in human glomerulonephritis. J Am Soc Nephrol. 2002;13(Suppl 1):S7–S13.
Vincent FB, Slavin L, Hoi AY, Kitching AR, Mackay F, Harris J, et al. Analysis of urinary macrophage migration inhibitory factor in systemic lupus erythematosus. Lupus Sci Med. 2018;5:e000277. https://doi.org/10.1136/lupus-2018-000277.
Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH, Austin A, et al. Derivation of the SLEDAI. A disease activity index for lupus patients. Arthritis Rheum. 1992;35:630–40.
Kono M, Yasuda S, Kato M, Kanetsuka Y, Kurita T, Fujieda Y, et al. Long-term outcome in Japanese patients with lupus nephritis. Lupus. 2014;23:1124–32.
Koska J, Stefan N, Dubois S, Trinidad C, Considine RV, Funahashi T, et al. mRNA concentrations of MIF in subcutaneous abdominal adipose cells are associated with adipocyte size and insulin action. Int J Obes. 2009;33:842–50.
Tan EM, Cohen AS, Fries JF, Masi AT, Mcshane DJ, Rothfield NF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271–7.
Sánchez-Serrano C. Mestizaje e historia de la población en México. Madrid: Real Academia de Ciencias Exactas Físicas y Naturales; 1996. p. 173–93.
Gladman D, Ginzler E, Goldsmith C, Fortin P, Liang M, Sanchez-Guerrero J, et al. The development and initial validation of the systemic lupus international collaborating clinics/American college of rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum. 1996;39:363–9.
Guzmán J, Cardiel MH, Arce-Salinas A, Sánchez-Guerrero J, Alarcón-Segovia D. Measurement of disease activity in systemic lupus erythematosus. Prospective validation of 3 clinical indices. J Rheumatol. 1992;19:1551–8.
McClelland GH, Irwin JR, Disatnik D, Sivan L. Multicollinearity is a red herring in the search for moderator variables: a guide to interpreting moderated multiple regression models and a critique of Iacobucci, Schneider, Popovich, and Bakamitsos (2016). Behav Res Methods. 2017;49:394–402.
Eberly LE. Multiple linear regression. In: Ambrosius WT, editor. Topics in Biostatistics. Totowa: Humana Press; 2007. p. 165–87.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for statistical Computing; 2019. Available from: https://www.R-project.org/.
Wickham H. ggplot2: Elegant Graphics for Data Analysis. 2nd ed. New York: Springer International Publishing; 2016.
Medina-Rosas J, Touma Z. Proteinuria: assessment and utility in lupus nephritis. Orthop Res Physiother. 2016;2:1–8.
Calandra T, Bernhagen J, Metz CN, Spiegel LA, Bacher M, Donnelly T, et al. MIF as a glucocorticoid-induced modulator of cytokine production. Nature. 1995;377:68–71.
Leech M, Metz C, Bucala R, Morand EF. Regulation of macrophage migration inhibitory factor by endogenous glucocorticoids in rat adjuvant-induced arthritis. Arthritis Rheum. 2000;43:827–33.
Kang I, Bucala R. The immunobiology of MIF: function, genetics and prospects for precision medicine. Nat Rev Rheumatol. 2019;15:427–37.
Calandra TT, Bernhagen J, Mitchell RA, Bucala R. The macrophage is an important and previously unrecognised source of macrophage migration inhibitory factor. J Exp Med. 1994;17:1895–902.
Otukesh H, Chalian M, Hoseini R, Chalian H, Hooman N, Bedayat A, et al. Urine macrophage migration inhibitory factor in pediatric systemic lupus erythematosus. Clin Rheumatol. 2007;26:2105–7.
Ouedraogo R, Wu X, Xu S-Q, Fuchsel L, Motoshima H, Mahadev K, et al. Adiponectin suppression of high-glucose-induced reactive oxygen species in vascular endothelial cells: evidence for involvement of a cAMP signaling pathway. Diabetes. 2006;55:1840–6.
Declèves A-E, Mathew AV, Cunard R, Sharma K. AMPK mediates the initiation of kidney disease induced by a high-fat diet. J Am Soc Nephrol JASN. 2011;22:1846–55.
Garcia-Gonzalez A, Gonzalez-Lopez L, Valera-Gonzalez IC, Cardona-Muñoz EG, Salazar-Paramo M, González-Ortiz M, et al. Serum leptin levels in women with systemic lupus erythematosus. Rheumatol Int. 2002;22:138–41.
Chen H, Shi B, Feng X, Kong W, Chen W, Geng L, et al. Leptin and neutrophil-activating peptide 2 promote Mesenchymal stem cell senescence through activation of the phosphatidylinositol 3-kinase/Akt pathway in patients with systemic lupus Erythematosus. Arthritis Rheumatol. 2015;67:2383–93.
Elshishtawy H, Ibrahim SE, Helmi A, Farouk N, Elshinnawy MA. Resistin in systemic lupus erythematosus: relation to lupus nephritis and premature atherosclerosis. Egypt Rheumatol. 2012;34:137–46.
Baker JF, Morales M, Qatanani M, Cucchiara A, Nackos E, Lazar MA, Teff K, von Feldt JM. Resistin levels in lupus and associations with disease-specific measures, insulin resistance, and coronary calcification. J Rheumatol. 2011;38:2369–75 https://doi.org/10.3899/jrheum.110237.
Lee YH, Song GG. Association between circulating leptin levels and systemic lupus erythematosus: an updated meta-analysis. Lupus. 2018;27:428–35.
Li H, Zhang T, Leng R, Li X, Li X, Pan H. Plasma/serum Leptin levels in patients with systemic lupus Erythematosus: a meta-analysis. Arch Med Res. 2015;46:551–6.
Huang Q, Tao S-S, Zhang Y-J, Zhang C, Li L-J, Zhao W, et al. Serum resistin levels in patients with rheumatoid arthritis and systemic lupus erythematosus: a meta-analysis. Clin Rheumatol. 2015;34:1713–20.
Santos FMM, Telles RW, Lanna CCD, Teixeira AL, Miranda AS, Rocha NP, et al. Adipokines, tumor necrosis factor and its receptors in female patients with systemic lupus erythematosus. Lupus. 2017;26:10–6.
Funding
This project was financed with funding from the Fondo de Investigación en Salud del Instituto Mexicano del Seguro Social (Grant: FIS/IMSS/PROT/G12/1135).
Author information
Authors and Affiliations
Contributions
Jorge Ivan Gamez-Nava: Conceptualization, Investigation, Resources, Funding acquisition, Supervision, Writing - Original Draft, Writing - Review & Editing. Valeria Diaz-Rizo: Investigation, Conceptualization, Writing - Original Draft, Writing - Review & Editing. Edsaul Emilio Perez-Guerrero: Formal analysis, Data Curation, Writing - Original Draft, Writing - Review & Editing, Visualization, Supervision. Jose Francisco Muñoz-Valle: Validation, Resources, Writing - Original Draft, Writing - Review & Editing. Ana Miriam Saldaña-Cruz: Investigation, Writing - Original Draft, Writing - Review & Editing. Nicte Selene Fajardo-Robledo: Investigation, Writing - Original Draft, Writing - Review & Editing. Heriberto Jacobo-Cuevas: Investigation, Writing - Original Draft, Writing - Review & Editing. Cesar Arturo Nava-Valdivia: Investigation, Writing - Original Draft, Writing - Review & Editing. Miriam Fabiola Alcaraz-Lopez: Investigation, Writing - Original Draft, Writing - Review & Editing. Xochitl Trujillo: Validation, Writing - Original Draft, Writing - Review & Editing. Miguel Huerta: Validation, Resources, Writing - Original Draft, Writing - Review & Editing. Ernesto German Cardona-Muñoz: Conceptualization, Investigation, Resources, Writing - Original Draft, Writing - Review & Editing, Supervision. Laura Gonzalez-Lopez: Conceptualization, Methodology, Investigation, Resources, Writing - Original Draft, Writing - Review & Editing, Supervision, Project administration. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All patients included in this work signed a written informed consent form prior to study entry. This study protocol was approved by the Research and Ethics board of the hospital. Approval reference: R-2011-1301-92. This study followed the recommendations described by the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
All the authors declare that there are no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gamez-Nava, J.I., Diaz-Rizo, V., Perez-Guerrero, E.E. et al. Assessment of serum macrophage migration inhibitory factor (MIF), adiponectin, and other adipokines as potential markers of proteinuria and renal dysfunction in lupus nephritis: a cross-sectional study. Biomark Res 8, 55 (2020). https://doi.org/10.1186/s40364-020-00236-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40364-020-00236-x