Abstract
Background
Workplace violence (WPV) is considered a global problem, particularly in the health sector; however, no studies have assessed the national prevalence of WPV against emergency physicians and the associated factors in China.
Methods
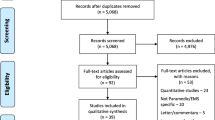
A national cross-sectional survey was conducted in 31 provinces/autonomous regions/municipalities across China between July 2019 and September 2019. A total of 15 455 emergency physicians were selected using a multistage stratified random sampling method. A structured self-administered questionnaire was used to collect information on WPV and potential associated factors among emergency physicians. Descriptive and multivariable logistic regression analyses were used to identify the predictors of WPV.
Results
A total of 14 848 emergency physicians responded effectively (effective response rate: 96.07%). Of the respondents, 90.40%, 51.45%, and 90.00% reported exposure to any type of WPV, physical or nonphysical violence in the preceding year, respectively. Verbal aggression (87.25%) was the most common form of violence, followed by threat (71.09%), physical assault (48.24%), verbal sexual harassment (38.13%), and sexual assault (19.37%). Patients’ families were the main perpetrators of these incidents. Unmet patient needs, taking drugs or drinking, and long waiting times were the main contributors to WPV. Physicians who were from low-developed regions, female, and without shift work were less likely to have experienced any type of WPV. Chinese emergency physicians who were from medium-developed regions, had a bachelor’s degree, worked in a higher level hospital, had a higher professional title, with lower incomes, had a history of hypertension or coronary heart disease, were smokers or drinkers, and worked in hospitals without preventive measures or training for WPV and not encouraging to report WPV were more likely to have experienced any type of WPV. The predictors of WPV varied in different types of WPV.
Conclusions
This study shows that the prevalence of WPV against emergency physicians is high in China. Measures should be taken at the physicians, patients, hospital, and national levels to protect GPs from WPV; for example, improving physicians’ level of service and hospital’ reporting procedures. Creating a prevention strategy and providing a safer workplace environment for emergency physicians should be prioritized.
Similar content being viewed by others
Background
Workplace violence (WPV) is defined as “incidents where staff are abused, threatened, or assaulted in circumstances related to their work, including commuting to and from work, involving an explicit or implicit challenge to their safety, well-being, or health” [1]. WPV against healthcare workers (HCWs) has become an important global challenge. A meta-analysis of WPV for all HCWs identified that 61.9% of HCWs reported exposure to any form of WPV [2]. WPV may contribute to reduced job satisfaction, commitment and efficiency, poor quality of life, increased stress, sleep disruption, burnout, turnover, and even death [3,4,5,6,7,8,9]. Therefore, the primary prevention of such violence worldwide is an important public health priority.
Violence against HCWs has been increasingly reported in China. The overall prevalence of WPV against healthcare professionals was 62.4%, and the prevalence of WPV across different specialties was significantly different, with WPV being highest in departments of emergency medicine (79.8%), followed by departments of pediatrics (73.7%), surgery (62.4%), gynecology (61.1%), and internal medicine (59.3%) [10]. In emergency departments (EDs), several factors converge that could contribute to WPV incidents. Concerning the patients, alcohol and drug intoxication and psychiatric illnesses were identified as important risk factors [3, 7, 8]. In terms of the organization and staff in EDs, long waiting times for patients, shift work, understaffed EDs, and high job demands of staff increased the risk of WPV [3, 7, 11]. Many emergency physicians believe that the threat of WPV ‘‘comes with the territory’’ of working in the EDs.
Previous studies have been conducted to investigate WPV and its risk factors among HCWs in EDs [3, 12,13,14,15,16,17]. Specially, studies that have focused on emergency physicians were limited [13, 14, 18]. To date, only one study investigated the prevalence and predictors of WPV toward 1103 frontline clinicians in EDs during the COVID-19 pandemic in China [19]. The lack of national-level data, it is difficult to provide comprehensive information and implement appropriate prevention policies and measures to prevent violence toward physicians in EDs. Therefore, this observational, national, cross-sectional survey aimed to investigate the prevalence of WPV toward emergency physicians and to determine the associated factors of different types of WPV in China.
Methods
Study population and sampling
A cross-sectional study was carried out in China from July 2019 to September 2019. The sample size was calculated according to the formula, n = [Z2π(1 − π)]/δ2 (n = sample size, Z = confidence level for a normal distribution, π = expected prevalence, and δ = absolute error). The prevalence of WPV among healthcare professionals in EDs in China was 79.8%, which was reported in a previous meta-analysis [10]. Taking a confidence interval (CI) of 95% and an absolute error of 1%, the ideal sample size was 6193. This sample size was increased to 6812 to compensate for nonresponses.
There are 22 provinces, 5 autonomous regions, and 4 municipalities of mainland China (not including Hong Kong, Macao, and Taiwan), and China is usually divided into eastern, central, and western regions. A multistage stratified random sampling design was used in this study. First, a total of 31 Chinese provinces/autonomous regions/municipalities were classified as high-developed, medium-developed, and low-developed regions according to per capita disposable income in 2018 (Additional file 1: Appendix). Second, we selected 10 hospitals randomly from each province/autonomous region/municipality. Third, according to the number and scale of the hospitals, from each sampled hospital, 40% of the emergency physicians who had practiced in the EDs for at least 6 months were randomly selected to complete a self-administered questionnaire. A simple random sampling method was used at each stage. The eligibility criteria of participants were: (1) physicians practiced in EDs; (2) worked for at least 6 months. In total, 15 455 emergency physicians were asked to participate in this survey, and 182 physicians did not respond. In addition, 30 questionnaires were discarded, because information on WPV was missing. Given the purpose of investigating the prevalence of WPV in the past year, we further excluded 395 emergency physicians whose work tenure was less than 1 year. Ultimately, 14 848 eligible questionnaires were used in this analysis. Thus, the sample size was sufficient for our study.
The study protocol was approved by the Institutional Ethics Board of the Second Affiliated Hospital of Hainan Medical University, Haikou, China (HYLL-2018-035). We obtained the consent of each medical institution involved in this study. All individuals provided written informed consent to the researchers before the survey, and participants’ personal information was kept confidential.
Instrument and measurement
The questionnaire was designed based on literature reviews, group discussions, and preliminary interviews. The questionnaire consisted of six parts: factors associated with WPV (sociodemographic information, health-related factors, and work environment related to WPV prevention), WPV, attitudes toward pre-hospital first aid, job burnout, depression symptoms, and turnover intention. Given the purpose of this study, the data from section 1 and 2 were included.
By reviewing the literature [6, 7, 13, 20, 21], we extracted the factors that might predict WPV: (1) sociodemographic characteristics: region, age, sex, marital status, education level, level of hospital, ownership, work tenure, contract status, professional title, income status, and shift work; (2) health-related factors: body mass index (BMI), history of hypertension, history of diabetes, history of coronary heart disease (CHD), smoking status, and alcohol drinking; (3) work environment related to WPV prevention: whether having preventive measures of WPV, having preventive training of WPV, and encouraging to report WPV. In this study, “shift work” was evaluated by one item “do you have night shifts in your usual work?” with 2 response options (yes/no).
The dependent variable was WPV toward emergency physicians. The Chinese version of the Workplace Violence Scale (WVS), developed by Wang et al. [22], has good reliability and validity for measuring the incidence of WPV when applied to medical staff in China. It includes 5 items measured with a four-point ordinal scale (0 = never, 1 = once, 2 = two or three times, 3 = more than three times). Five types of WPV including physical assault, verbal abuse, threat, verbal sexual harassment, and sexual assault were investigated. The total score of the WVS was created by adding the scores for each item, ranging from 0 to 15, with higher scores indicating a higher frequency of experiencing WPV. Scoring 0 was considered not to have been exposed to WPV, and scoring 1 to 5, 6 to 10, and 11 to 15 indicated low, medium, and high frequency of WPV, respectively [22]. WPV was further classified as physical (physical assault and sexual assault) and nonphysical (verbal abuse, threat, and verbal sexual harassment) violence. In this study, Cronbach’s alpha for WVS was 0.80.
Moreover, the perpetrators, causes, and reactions to the most recent experience of WPV in the past year were assessed in this study. The perpetrators of WPV were investigated by one closed-ended, multiple-choice question with 8 responses (patients, patients’ families, colleagues, managers/supervisors, external colleagues, general public, visitors, and others). Two closed-ended, multiple-choice questions (more than one answer) were used to investigate the reasons for WPV (long waiting times, dissatisfied with GPs’ service, unmet patient needs, perpetrators’ death, perpetrators’ mental disorder, thinking medical costs high, requiring financial compensation, after taking drugs or drinking, dissatisfied with treatment effect, and others) and the reactions to WPV (took no action, tried to pretend it never happened, stopped the perpetrators, told friends or families, told colleagues, sought help from managers, sought help from union, called the police, transferred to another position, completed a WPV report, pursued prosecution, and others), respectively.
Data collection and quality control
In the stage of study design, we invited 20 healthcare experts to evaluate the content validity of the questionnaire. A pretest involving 50 emergency physicians was conducted in Wuhan’s community hospitals to improve the quality of the questionnaire. A total of 47 respondents could clearly understand all the context of the questionnaire. Further modifications were made according to the feedback of respondents. A web link to the online questionnaire, which was designed using Questionnaire Star, was disseminated to participants through WeChat (similar to WhatsApp in Western countries, WeChat is the largest communication platform in China, with over one billion users). To prevent the same participant from repeatedly answering the questionnaire, each device (e.g., smartphone or computer) was eligible to complete the questionnaire once, and logical checks were concurrently run on the Questionnaire Star platform to identify invalid questionnaires. The data were entered into a web-based database by trained investigators to ensure accuracy.
Data analysis
The descriptive analyses used means (standard deviation, SD) for the continuous variables and frequency (percentage) for the categorical data. In the logistic regression model, the predictive variables included socioeconomic development level (developed, middle-developed, less-developed), geographic region (eastern China, central China, western China), age (< 45 years, ≥ 45 years), sex (male, female), marital status (unmarried/widowed/divorced, married), education level (associate’s degree or vocational diploma, bachelor degree, master degree or higher), level of hospital (others, secondary hospital, tertiary hospital), ownership (non-governmental, governmental), work tenure (< 10 years, ≥ 10 years), contract status (permanent, temporary), professional title (elementary or below, intermediate, senior), income status (high, middle, low), shift work (yes, no), BMI (< 18.5 kg/m2, 18.5–< 24.0 kg/m2, 24.0–< 28.0 kg/m2, ≥ 28.0 kg/m2), history of hypertension (yes, no), history of diabetes (yes, no), history of CHD (yes, no), smoking status (nonsmokers, smokers), alcohol drinking (nondrinkers, drinkers), whether working in hospitals which had preventive measures of WPV (yes, no), had preventive training of WPV (yes, no), or encouraged to report WPV (yes, no). Any type of violence, physical violence, and nonphysical violence, as the dependent variables, were treated as categorical variables. Multivariable stepwise logistic regression analysis (cutoffs for selection and elimination: P = 0.05 and P = 0.10, respectively) was used to calculate the odds ratios (ORs) and 95% CIs for factors that might be associated with the prevalence of WPV (any type of violence, physical violence, and nonphysical violence) toward emergency physicians. All analyses were performed using Statistical Package for Social Sciences (SPSS, Inc., Chicago, IL, Version 27.0) software, and all tests were two-sided with a significance level of 0.05.
Results
Table 1 presents the main characteristics of the survey respondents. A total of 14 848 respondents were included in the data analysis, yielding an effective response rate of 96.07%. Among the 14 848 respondents, approximately 40% of respondents were from medium-developed regions. Slightly more than one-third (33.58%) of participants were from western China. The mean age was 37.84 (SD = 8.01) years. Most were men (70.53%), married (84.16%), and had a bachelor’s degree or above (94.19%). More than 65% of the participants had intermediate or senior professional titles. In total, 55.65% of the respondents were in the middle or higher level of income groups, and the majority of the respondents experienced shift work. Less than two-thirds of participants worked in hospitals which had preventive measures for WPV.
Overall, 90.40% of respondents reported exposure to WPV in the previous 12 months. Verbal aggression (87.25%) was the most common form of violence, followed by threat (71.09%), physical assault (48.24%), verbal sexual harassment (38.13%), and sexual assault (19.37%). In addition, 51.45% and 90.00% reported exposure to physical and nonphysical violence, respectively.
The perpetrators, reasons for, and responses to exposure to violent acts
Table 2 shows the perpetrators, reasons for WPV, and reactions to WPV, respectively. In general, violence, whether physical or nonphysical, was perpetrated mainly by patients’ families and by patients. More than two-thirds of respondents reported that they had been exposed to any type of WPV by families of patients. “Unmet patient needs”, “After taking drugs or drinking”, and “Long waiting times” were the top three reasons for WPV among emergency physicians.
Concerning the reactions of emergency physicians to physical violence, 3459 of 7639 participants who had been attacked called the police (45.28%), 2443 reported it to the managers (31.98%), and 2405 completed an incident/accident report (31.48%). Concerning the reactions of emergency physicians to nonphysical violence, 4614 of 13 363 participants who had been attacked called the police (34.53%), 3732 reported it to the managers (27.93%), and 3696 completed an incident/accident report (27.66%).
Factors associated with WPV
The results of the multivariable stepwise logistic regression analysis of the factors associated with the prevalence of any type of violence, physical violence, and nonphysical violence among emergency physicians are shown in Table 3. Socioeconomic development level (medium: OR = 1.20, low: OR = 0.75), sex (female: OR = 0.75), educational level (bachelor degree: OR = 1.31), level of hospital (secondary hospital: OR = 3.14, tertiary hospital: OR = 3.55), professional title (intermediate: OR = 1.45, senior: OR = 1.39), income status (middle: OR = 1.25; low: OR = 1.26), shift work (no: OR = 0.37), history of hypertension (yes: OR = 1.52), history of CHD (yes: OR = 1.64), smokers (OR = 1.20), drinkers (yes: OR = 1.25), worked in hospitals without preventive measures (OR = 1.24) or training (OR = 1.58) of WPV and not encouraging to report WPV (OR = 1.99) were predictors of any type of WPV against emergency physicians. The most significant predictors of physical and nonphysical violence were consistent with those associated with any type of WPV. Moreover, geographic region, age, BMI, and history of diabetes were associated factors for physical violence.
Discussion
To our knowledge, this is the first study investigating the prevalence of WPV and the associated factors in Chinese emergency physicians at a national level. We found that the prevalence of nonphysical violence was higher than physical violence against emergency physicians in China. The sex, level of hospital, professional title, income status, shift work, history of hypertension, history of CHD, alcohol drinking, working in hospitals which had preventive measures or training on WPV and encouraged to report WPV were common factors associated with any type of WPV, nonphysical violence, and physical violence.
Violence in the workplace is a common phenomenon in the EDs. The findings revealed that 90.40% of Chinese emergency physicians had been exposed to WPV during the previous 12 months. The percentage of emergency physicians experiencing any type of WPV was greatly higher than the overall prevalence of WPV against Chinese ED clinicians during the COVID-19 pandemic (29.2%) [19]. Similarly, the prevalence of WPV against Chinese HCWs decreased after the COVID-19 pandemic [23, 24]. The improved doctor–patient relationship and doctor–patient trust during the COVID-19 pandemic may interpret the variation to some degree [24]. The prevalence of any type of WPV was higher than that reported for emergency physicians in Turkey (78.1%) [13], Morocco (70%) [25], and the USA (74.9%) [26]. However, nonphysical violence was markedly less prevalent [27, 28]. The prevalence of verbal sexual harassment (38.13%) was also lower than that reported in other countries [12, 15, 29]. The differences might be due, at least in part, to differences in sample size and the participants’ characteristics, including their socioeconomic status, their geographic region, the practice setting, the definitions and time period of WPV, and the policy for reporting WPV in their national context.
There were significant differences in the prevalence of any form of WPV, nonphysical violence, and physical violence according to gender, consistent with previous studies [30,31,32,33,34]. One explanation for the lower risk of threat and assault for women emergency physicians may be that women are more likely to adopt specific personal risk reduction measurements than their male counterparts [33]. The lower risk may be also associated with differences in patient caseload and work arrangements [35]. The gendered embodiment relates to feminine vulnerability and masculine strength and control in the context of physical and sexual violence from men but also to men’s assumed vulnerability to allegations of sexual abuse from women patients. Thus, male and female physicians might utilize previously developed ways of doing gender to establish measures to manage violence in particular settings [36]. Another possible interpretation is that male physicians are more easily influenced by the work-related aspects of the job, but female physicians are affected more by the job interfering with their family life. Finally, other researchers have explained this gender difference by hypothesizing that males have greater exposure to violent patients or that there may be a tendency for males to feel more protective of female staff [37].
In our study, we found that emergency physicians who had higher professional titles were at higher risk of any type of WPV, physical violence, and nonphysical violence. Similar results were found among hospital HCWs in China, which indicated that professional title was associated with WPV [34]. A higher professional level may mean a heavier workload, which may affect the quality of physicians’ service delivery [10]. In general, patients have much higher expectations of higher ranking physicians [33]. Patients tend to seek high-level medical services even for minor, self-limiting conditions. Thus, the heavy patient load increased the work stress of physicians, contributing to long-term overwork, which may lead to rushing, indifference, and disrespect toward patients; this can lead to a poor relationship between physicians and patients [33, 38].
Emergency physicians who did shift work were prone to experience WPV, which was consistent with the previous studies [13, 19, 34, 39]. Several reasons could explain the effects of shift work on WPV, including the shortage of staff on night shifts, staff exhaustion, and the consequent impact on patient satisfaction [34]. In our study, the majority of respondents had night shift work. It is necessary to have more security personnel during the night shifts.
Similar to the results reported in the literature [12, 14, 16, 17, 40, 41], our study showed that violence was mainly perpetrated by patients themselves and by patients’ families. However, Jia et al. [41] scrutinized medical WPV incidents reported online in Chinese hospitals from 2010 to 2020 and revealed that visitors were more likely to cause serious damage and mortality to the victims than family members of patients. Visitors came to hospitals not to consult a doctor but to seek out relevant healthcare personnel they may retaliate with [41]. In addition, unmet patient needs and long waiting times were two important reasons for WPV. This indicated that when individuals were exposed to critical health conditions and waited for long times until seen by a physician, they and their relatives had a high level of stress, feelings of anger and frustration which in turn manifested in the form of violence against physicians [16, 42]. The causes of violence against physicians in Chinese EDs were similar to those reported in previous studies [16, 25, 40, 43]. To address the ED-related factors, hospital managers can work on reducing wait times through better utilization of resources and can introduce a triage system to prioritize patients and identify those who cannot wait long to be seen. In addition, medical institutions should offer appropriate treatment to control medical costs, and enhance preventive measures (e.g., adding security personnel, repairing cameras and alarm systems) to protect workers from violence. As we identified, physicians who worked in hospitals that had WPV training programs had a lower risk of experiencing WPV, which was in accordance with a previous study [40]. This highlights that it is warranted to enhance education programs to train HCWs on how to deal with aggressive persons and protect themselves from violence.
Strengths and limitations
This is the first investigation of the prevalence of WPV and the relevant determinants among emergency physicians in China. The large sample size significantly increased the statistical power to detect determinates of violence. In addition, as WPV is increasingly prevalent in modern society, the results of our study can not only provide baseline data for violence interventional strategies and program assessment in China but can also provide a reference for international comparisons. Third, the survey was anonymous and self-administered, which probably made respondents provide more valid responses, especially regarding sensitive issues such as sexual harassment in addition to eliminating interviewer bias.
Our study had some limitations. First, this study has a cross-sectional design, and we cannot infer causality from the results. Second, all information was collected from a self-report questionnaire and response bias was, therefore, unavoidable. Third, there may be other potential influencing factors for WPV beyond those we investigated; we thus failed to identify all such factors. Fourth, we did not investigate the characteristics of perpetrators, reasons for taking no action among emergency physicians, and subsequent actions of managers or union regarding WPV against emergency physicians, which need to be further assessed in future studies. Finally, we should acknowledge the possibility of underreporting due to time-consuming incident reporting procedures, fear of stigmatization, or a belief that reporting violent incidents will not lead to any positive changes.
Implications for research and practice
Further research is needed to examine the impact of violence on job satisfaction, burnout, and retention. Interventional studies that examine the impact of measures or programs on decreasing WPV are also needed. Prevention measures might include developing education and training programs to help emergency physicians better manage WPV. It may also be beneficial to increase public awareness of the magnitude of the phenomenon of WPV against emergency physicians through mass media campaigns.
Conclusions
This survey suggests that violence occurs frequently in EDs in China. The most prevalent type of violence is verbal aggression, followed by threat, physical assault, sexual harassment, and sexual assault. Patients’ families are the main perpetrators of these incidents. Unmet needs of patients, taking drugs or drinking, and long waiting times are the main reasons for violence. Chinese health authorities should establish measures to prevent WPV in healthcare settings, since WPV could threaten the health care system’s sustainability.
Availability of data and materials
Data may be made available by contacting the corresponding author.
Abbreviations
- BMI:
-
Body mass index
- CHD:
-
Coronary heart disease
- CI:
-
Confidence interval
- EDs:
-
Emergency departments
- HCWs:
-
Healthcare workers
- ORs:
-
Odds ratios
- SD:
-
Standard deviation
- SPSS:
-
Statistical Package for Social Sciences
- WPV:
-
Workplace violence
- WVS:
-
Workplace Violence Scale
References
International Labour Office, International Council of Nurses, World Health Organization, Public Services International. Framework guidelines for addressing workplace violence in the health sector. Geneva: World Health Organization; 2002.
Liu J, Gan Y, Jiang H, Li L, Dwyer R, Lu K, et al. Prevalence of workplace violence against healthcare workers: a systematic review and meta-analysis. Occup Environ Med. 2019;76:927–37.
Aljohani B, Burkholder J, Tran QK, Chen C, Beisenova K, Pourmand A. Workplace violence in the emergency department: a systematic review and meta-analysis. Public Health. 2021;196:186–97.
Wirth T, Peters C, Nienhaus A, Schablon A. Interventions for workplace violence prevention in emergency departments: a systematic review. Int J Environ Res Public Health. 2021;18(16):8459.
Kumari A, Kaur T, Ranjan P, Chopra S, Sarkar S, Baitha U. Workplace violence against doctors: characteristics, risk factors, and mitigation strategies. J Postgrad Med. 2020;66:149–54.
Ashton RA, Morris L, Smith I. A qualitative meta-synthesis of emergency department staff experiences of violence and aggression. Int Emerg Nurs. 2018;39:13–9.
Nikathil S, Olaussen A, Gocentas RA, Symons E, Mitra B. Review article: workplace violence in the emergency department: a systematic review and meta analysis. Emerg Med Australas. 2017;29:265–75.
Cabilan CJ, Johnston AN. Review article: identifying occupational violence patient risk factors and risk assessment tools in the emergency department: a scoping review. Emerg Med Australas. 2019;31:730–40.
Nowrouzi-Kia B, Chai E, Usuba K, Nowrouzi-Kia B, Casole J. Prevalence of type II and type III workplace violence against physicians: a systematic review and meta-analysis. Int J Occup Environ Med. 2019;10:99–110.
Lu L, Dong M, Wang SB, Zhang L, Ng CH, Ungvari GS, et al. Prevalence of workplace violence against health-care professionals in china: a comprehensive meta-analysis of observational surveys. Trauma Violence Abuse. 2020;21:498–509.
Hofmann T, Hachenberg T. Violence in the emergency medicine (emergency rescue service and emergency departments)—current situation in Germany. Anasth Intensiv Notf. 2019;54:146–54.
HedayatiEmam G, Alimohammadi H, ZolfaghariSadrabad A, Hatamabadi H. Workplace violence against residents in emergency department and reasons for not reporting them; a cross sectional study. Emerg. 2018;6:e7.
Bayram B, Çetin M, ÇolakOray N, Can İ. Workplace violence against physicians in Turkey’s emergency departments: a cross-sectional survey. BMJ Open. 2017;7:e013568.
Zafar W, Khan UR, Siddiqui SA, Jamali S, Razzak JA. Workplace violence and self-reported psychological health: coping with post-traumatic stress, mental distress, and burnout among physicians working in the emergency departments compared to other specialties in Pakistan. J Emerg Med. 2016;50:167-77.e161.
Schnapp BH, Slovis BH, Shah AD, Fant AL, Gisondi MA, Shah KH, et al. Workplace violence and harassment against emergency medicine residents. West J Emerg Med. 2016;17:567–73.
Abdellah RF, Salama KM. Prevalence and risk factors of workplace violence against health care workers in emergency department in Ismailia. Egypt Pan Afr Med J. 2017;26:21.
Cannavò M, La Torre F, Sestili C, La Torre G, Fioravanti M. Work related violence as a predictor of stress and correlated disorders in emergency department healthcare professionals. Clin Ter. 2019;170:e110–23.
Al-Sahlawi KS, Zahid MA, Shahid AA, Hatim M, Al-Bader M. Violence against doctors: 1. A study of violence against doctors in accident and emergency departments. Eur J Emerg Med. 1999;6:301–4.
Liu R, Li Y, An Y, Zhang L, An FR, Luo J, et al. Workplace violence against frontline clinicians in emergency departments during the COVID-19 pandemic. PeerJ. 2021;9:e12459.
Zhang Y. Study on the current situation and coping strategies of workplace violence for emergency nurses in general hospital. Chongqing Medical University. 2017.
Phillips JP. Workplace violence against health care workers in the United States. N Engl J Med. 2016;374:1661–9.
Wang P, Wang M, Hu G, Wang Z, Lan Y, Jiang J, et al. Study on the relationship between workplace violence and work ability among health care professionals in Shangqiu City. J Hygiene Res. 2006;35(4):472–5.
Qi M, Hu X, Liu J, Wen J, Hu X, Wang Z, et al. The impact of the COVID-19 pandemic on the prevalence and risk factors of workplace violence among healthcare workers in China. Front Public Health. 2022;10:938423.
Zhou Y, Chen S, Liao Y, Wu Q, Ma Y, Wang D, et al. General perception of doctor-patient relationship from patients during the COVID-19 pandemic in China: a cross-sectional study. Front Public Health. 2021;9:646486.
Belayachi J, Berrechid K, Amlaiky F, Zekraoui A, Abouqal R. Violence toward physicians in emergency departments of Morocco: prevalence, predictive factors, and psychological impact. J Occup Med Toxicol. 2010;5:27.
Kowalenko T, Walters BL, Khare RK, Compton S. Workplace violence: a survey of emergency physicians in the state of Michigan. Ann Emerg Med. 2005;46:142–7.
Pich JV, Kable A, Hazelton M. Antecedents and precipitants of patient-related violence in the emergency department: results from the Australian VENT Study (Violence in Emergency Nursing and Triage). Australas Emerg Nurs J. 2017;20:107–13.
Miedema B, Hamilton R, Lambert-Lanning A, Tatemichi SR, Lemire F, Manca D, et al. Prevalence of abusive encounters in the workplace of family physicians: a minor, major, or severe problem? Can Fam Physician. 2010;56:e101–8.
Gates DM, Ross CS, McQueen L. Violence against emergency department workers. J Emerg Med. 2006;31:331–7.
Tiruneh BT, Bifftu BB, Tumebo AA, Kelkay MM, Anlay DZ, Dachew BA. Prevalence of workplace violence in Northwest Ethiopia: a multivariate analysis. BMC Nurs. 2016;15:42.
Algwaiz WM, Alghanim SA. Violence exposure among health care professionals in Saudi public hospitals. A preliminary investigation. Saudi Med J. 2012;33:76–82.
Campbell JC, Messing JT, Kub J, Agnew J, Fitzgerald S, Fowler B, et al. Workplace violence: prevalence and risk factors in the safe at work study. J Occup Environ Med. 2011;53:82–9.
Gan Y, Li L, Jiang H, Lu K, Yan S, Cao S, et al. Prevalence and risk factors associated with workplace violence against general practitioners in Hubei, China. Am J Public Health. 2018;108:1223–6.
Tian Y, Yue Y, Wang J, Luo T, Li Y, Zhou J. Workplace violence against hospital healthcare workers in China: a national WeChat-based survey. BMC Public Health. 2020;20:582.
Elston MA, Gabe J. Violence in general practice: a gendered risk? Sociol Health Illn. 2016;38:426–41.
Chesney-Lind M. Gender, Heterosexuality, and Youth Violence. Theor Criminol. 2013;17:134–6.
Shields M, Wilkins K. Factors related to on-the-job abuse of nurses by patients. Health Rep. 2009;20:7–19.
Hesketh T, Wu D, Mao L, Ma N. Violence against doctors in China. BMJ. 2012;345: e5730.
Abou-ElWafa HS, El-Gilany AH, Abd-El-Raouf SE, Abd-Elmouty SM, El-Sayed RS. Workplace violence against emergency versus non-emergency nurses in Mansoura university hospitals, Egypt. J Interpers Violence. 2015;30:857–72.
Hamdan M, Abu HA. Workplace violence towards workers in the emergency departments of Palestinian hospitals: a cross-sectional study. Hum Resour Health. 2015;13:28.
Jia C, Han Y, Lu W, Li R, Liu W, Jiang J. Prevalence, characteristics, and consequences of verbal and physical violence against healthcare staff in Chinese hospitals during 2010–2020. J Occup Health. 2022;64: e12341.
Behnam M, Tillotson RD, Davis SM, Hobbs GR. Violence in the emergency department: a national survey of emergency medicine residents and attending physicians. J Emerg Med. 2011;40:565–79.
Alameddine M, Kazzi A, El-Jardali F, Dimassi H, Maalouf S. Occupational violence at Lebanese emergency departments: prevalence, characteristics and associated factors. J Occup Health. 2011;53:455–64.
Acknowledgements
We would like to thank the study participants and all staff members involved in this study for their efforts in the data collection.
Funding
This study was funded by the Hainan Provincial Key Research and Development Project (ZDYF2020112), Key Laboratory of Emergency and Trauma of Ministry of Education (Hainan Medical University) (Grant. KLET-202101), Hainan Provincial Natural Science Foundation of China (818MS148), and Key Laboratory of Emergency and Trauma of Ministry of Education (Hainan Medical University) (Grant. KLET-202103).
Author information
Authors and Affiliations
Contributions
SJY, JF, YG, and CZL conceived and designed the study. SJY, JF, YG, RXW, XYS, and ZQL participated in the acquisition of data. JF and YG analyzed the data. XYS gave advice on methodology. SJY and YG drafted the manuscript, and SJY, JF, YG, XYS, XTH, and CZL revised the manuscript. CZL is the guarantor of this work and had full access to all the data in the study and takes responsibility for its integrity and the accuracy of the data analysis. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Ethics Board of the Second Affiliated Hospital of Hainan Medical University, Haikou, China (HYLL-2018-035). Written informed consent was obtained from all survey participants.
Consent for publication
Not applicable.
Competing interests
We declare that we have no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Distribution of provinces/autonomous regions/municipalities, per capita disposable income in 2018, socioeconomic development level, and geographic region.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yan, S., Feng, J., Gan, Y. et al. Prevalence and predictors of workplace violence against emergency physicians in China: a cross-sectional study. Hum Resour Health 21, 8 (2023). https://doi.org/10.1186/s12960-022-00784-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12960-022-00784-3