Abstract
Background
Malaria rapid diagnostic tests (RDTs) available as dipsticks or strips, are simple to perform, easily interpretable and do not require electricity nor infrastructural investment. Correct interpretation of and compliance with the RDT results is a challenge to drug sellers. Thus, drug seller interpretation of RDT strips was compared with laboratory scientist re-reading, and PCR analysis of Plasmodium DNA extracted from RDT nitrocellulose strips and fast transient analysis (FTA) cards. Malaria RDT cassettes were also assessed as a potential source of Plasmodium DNA.
Methods
A total of 212 children aged between 2 and 60 months, 199 of whom had complete records at two study drug shops in south western Uganda participated in the study. Duplicate 5 μL samples of capillary blood were picked from the 212 children, dispensed onto the sample well of the CareStart™ Pf-HRP2 RDT cassette and a FTA, Whatman™ 3MM filter paper in parallel. The RDT strip was interpreted by the drug seller within 15–20 min, visually re-read centrally by laboratory scientist and from it; Plasmodium DNA was recovered and detected by PCR, and compared with FTA recovered P. falciparum DNA PCR detection.
Results
Malaria positive samples were 62/199 (31.2%, 95% CI 24.9, 38.3) by drug seller interpretation of RDT strip, 59/212 (27.8%, 95% CI 22.2, 34.3) by laboratory scientist, 55/212 (25.9%, 95% CI 20.0, 32.6) by RDT nitrocellulose strip PCR and 64/212 (30.2%, 95% CI 24.4, 37.7). The overall agreement between the drug seller interpretation and laboratory scientist re-reading of the RDT strip was 93.0% with kappa value of 0.84 (95% CI 0.75, 0.92). The drug seller compliance with the reported RDT results was 92.5%. The performance of the three diagnostic strategies compared with FTA-PCR as the gold standard had sensitivity between 76.6 and 86.9%, specificity above 90%, positive predictive values ranging from 79.0 to 89.8% and negative predictive values above 90%.
Conclusion
Drug sellers can use RDTs in field conditions and achieve acceptable accuracy for malaria diagnosis, and they comply with the RDT results. Plasmodium DNA can be recovered from RDT nitrocellulose strips even in the context of drug shops. Future malaria surveillance and diagnostic quality control studies with RDT cassette as a source of Plasmodium DNA are recommended.
Similar content being viewed by others
Background
A global increase of 5 million malaria cases in 2016 as compared to the year before [1] calls for improved deployment of available malaria interventions. Up to 445,000 out of an estimated 216 million malaria cases died in 2016 [1]. Prompt diagnosis and case management remains a mainstay of malaria control efforts. It promotes detection of non-malaria illnesses, prevents progression to severe disease or death and halts malaria parasite transmission.
Although, most people who seek treatment for malaria in the government health system receive accurate diagnosis and effective medicines [1, 2], coverage remains low [2]. Only a third (34%) of febrile children are taken to a medical provider in the government-run health sector in sub Saharan countries such as Uganda [1]. The remaining proportion of febrile children seeks care at the community level, from drug sellers and informal health providers.
The global malaria policy of universal testing and treatment aims to detect malaria cases in the first 24 h [3]. Although, blood smear microscopy is the gold standard for malaria diagnosis [4], it is cumbersome, requires experienced technical expertise and consistent availability of consumables and power supply [5]. Thus, it is largely inaccessible for majority of suspected malaria cases in remote rural areas and government health facilities [4, 5]. However, malaria rapid diagnostic tests (RDTs) available as dipsticks or strips can fill this gap [4,5,6,7,8]. They are simple to perform, easily-interpretable and do not require electricity or infrastructural investment [5, 6, 8]. Individuals with no or minimal health training, such as community health workers and some drug sellers can use them [9, 10]. For these reasons, RDTs have been incorporated into the integrated community case management (iCCM) intervention, a WHO/UNICEF recommended community level strategy [10,11,12] to target antimalarial medicines to parasite confirmed febrile cases. Proper diagnosis of malaria reduces antimalarial drug pressure [4, 7] and triggers the necessity to detect and treat bacterial infections, both of importance in combating antimicrobial resistance [13].
Malaria RDTs are based on immunochromatographic assays with coloured detecting antibodies impregnated on nitrocellulose membranes [5, 6, 8]. They detect specific malaria parasite antigens present in blood of infected or recently infected people [6, 8]. Most widely available RDTs target the histidine-rich protein 2 (HRP2), an antigen that is unique and thus specific to Plasmodium falciparum [6, 14]. Other malaria RDTs target parasite-specific lactate dehydrogenase (pLDH) and aldolase [6]. The Pf-HRP2 RDTs have better sensitivity and greater thermal stability than pLDH-detecting RDTs [6]. They are suitable for use in malaria endemic areas in sub-Saharan Africa where malaria cases are predominantly due to P. falciparum [15].
Correct interpretation of the RDT reading and compliance with the observed result is important to their appropriate use [4, 14]. Studies among drug sellers in Ghana [16], Nigeria (community pharmacies) [17], Uganda [18,19,20,21,22,23], Tanzania [24], and Myanmar [25] report that RDTs can be safely used, are highly sensitive but have low specificity. For instance, Ansah et al. reports RDT specificity of 30%, 31% and 52% [16], and Mbonye et al., 63.1% [21]. Two studies including one by the authors report a higher positivity rate from RDTs than microscopy, 47% versus 9.3% in South West Uganda [23] and 41% versus 13% in Tanzanian Morogoro region [24], respectively. Mbonye et al. shows one-third of RDT positive cases are malaria negative on expert microscopy and a monthly RDT positivity rate consistently higher than that of microscopy over the 1-year study period [21]. It is not clear whether these observations are due to drug sellers’ conflict of interest for sale of artemisinin-based combination medicines, performance characteristics of the RDT under field conditions or failure of the drug seller to interpret RDT lines. One study reports that community health workers who are traders have six times the odds of prescribing artemisinin-based combination medicines to RDT-negative children than farmers [26]. Also, with the exception of one study in a high malaria transmission setting [21], drug seller interpretation of the RDT reading has not been investigated, especially in the context of low malaria transmission setting. If not addressed, the RDT false positive rates can undermine confidence in the results and diminish the perceived importance of the test and treat guidelines [27].
Additionally, the variation in the observed adherence to RDT results increases the uncertainty about the drug sellers’ ability to interpret RDTs and their performance under field conditions. Although appropriate treatment is moderate (55%) in Nigeria [17] to high (80–99%) in Uganda [19, 21, 23], compliance with negative test results is low. Up to 32% of RDT negative cases in the Ghanaian [16], 37.4% [21] and 45% [20] in the Ugandan, and 51.6% in the Myanmar is studies [25] receive anti-malarial medicines. In the Tanzanian study [24], only 7% of the test negative cases received artemisinin-based combination therapy (ACT).
Therefore, this study was conducted to compare drug seller interpretation of RDTs in the field with the laboratory scientist repeat reading and to assess drug seller compliance with the observed RDT results. The performances of drug seller interpretation and laboratory scientist re-reading of the malaria RDT strips were also compared against polymerase chain reaction (PCR) analysis of Plasmodium DNA recovered from dry blood spotted FTA cards. PCR analysis of Plasmodium DNA is superior to RDT and is ten times more sensitive [28]. Since Plasmodium DNA can be recovered from malaria RDT nitrocellulose strips [28,29,30,31], the authors retrieved the RDTs from the study drug shops, extracted DNA from their nitrocellulose strips and analysed it by PCR. The authors argue that this provides an opportunity to incorporate quality assurance into the drug sellers’ use of RDTs.
Methods
Participants
The study population consisted of children aged 2–60 months presenting with fever or history of fever, acute respiratory illness and diarrhoeal diseases at two drug shops in Mbarara district. For the purpose of the study each child provided paired blood samples obtained by a finger-prick.
Setting
Mbarara district is located in South Western Uganda, perceived as a relatively low malaria transmission setting, with malaria parasite prevalence by microscopy among healthy children in the community, averaging between 4.1% [32] and 9.3% [33]. Drug shops in rural areas of Mbarara district were part of a prospective evaluation of the iCCM intervention for paediatric illness in registered drug shops from February 2014 to September 2015. The drug sellers were trained to assess and classify febrile children using clinical signs and symptoms according to the iCCM algorithm. They were given access to anti-malarial drugs (ACT), amoxicillin tablets, zinc sulfate tablets and oral rehydration salts at subsidized prices, RDTs and respiratory count timers free of charge. The iCCM intervention also had a community sensitization component and monthly support supervision by a clinical officer or pharmacist. Details of the iCCM intervention and effects on the health system in Mbarara district have been published elsewhere [23, 34]. Out of a total of 61 drug shops that participated in the iCCM intervention in Mbarara district, two drug shops that recorded most attendance by children less than 5 years were enrolled into the current study, several months after the end of the iCCM intervention, from December 2015 to April 2016.
Specimen collection
Drug sellers at the study drug shops were trained on how to perform the RDTs according to the revised iCCM intervention guidelines and to collect a blood spot on fast transient analysis (FTA), Whatman™ 3MM filter paper. A child presenting with fever or history of fever was assessed by drug seller to undergo malaria diagnostic testing using the iCCM sick child job aid. A total of 212 duplicate samples of capillary blood were picked from each child, one sample, approximately 5 μL was dispensed into the sample well of the CareStart™ Pf-HRP2 RDT cassette (ACCESS BIO, INC. Ethiopian Branch, Yeka, Addis Ababa, Ethiopia), followed by a drop of diluent/buffer into the diluent well, as stated in the manufacturer’s instructions. The drug seller had been instructed to read and interpret the result off the RDT strip after 15–20 min, as stated in the manufacturer’s instructions. The second blood sample, approximately 5 μL, was spotted on a fast transient analysis (FTA), Whatman™ 3MM filter paper in parallel. The blood spotted RDT strips and FTA filter papers were left to dry in open air for up to 30 min, after which they were packaged and stored in transparent zip-lockable polythene bags, labelled with name of under-five (U5) child, drug shop name and date of sample collection.
Drug sellers collected the blood samples as the procedures involved do not require highly trained individuals and equipment such as centrifuge, deep freezer and needles [35, 36]. This technique is advantageous when taking biologic fluid samples from children as it requires small quantities of blood and can use capillary instead of venous blood. Since, dried blood spots on RDT strips and FTA filter paper are stable in tropical climates [36, 37], they were kept at normal working temperatures for up to 2 months before being transferred to the molecular laboratory at the Department of Medical Microbiology, Makerere University College of Health Science. The specimen were protected from adverse conditions of extreme cold or hot [> 40 °C (°Celsius)] temperatures and moisture.
Nested PCR for detection of Plasmodium falciparum
Plasmodium DNA was extracted from blood spot collected on FTA card and RDT strips using Chelex method [30] and QIAamp blood kit (QIAGEN, Inc., Chatsworth, CA), following manufacturer’s instructions. The quantity and quality of the extracted DNA was assessed using Nano Spectrophotometry and QIAxcel advanced automated capillary electrophoresis following the manufacturer’s guideline.
Detection of P. falciparum was done using nested PCR that employed two sets of primers that targeted 18S rRNA gene to confirm the genus and species. Nested PCR was performed according to the protocol developed by Snounou et al. in two sequential steps [38]. The first round PCR was performed in 50 µL volume consisting of 1 × of Taq 2× Master Mix (New England BioLabs, Massachusetts, USA) of 10 pmol/μL each, of the forward and reverse genus specific outer primers (Table 1), PCR grade water and 5.0 μL of 50 ng/μL template DNA. The reaction was performed with an initial denaturation at 95 °C for 5 min, followed by 35 cycles of 1 min at 94 °C, 2 min at 58 °C, and 2 min at 72 °C, and final extension at 72 °C for 10 min in using a Thermal cycler (Bio-Rad, T100; Singapore).
Two micro litres (µL) of the first round PCR amplicons were subjected to second PCR using the same amplification conditions and a P. falciparum-specific internal primer. The PCR products were analysed using QIAxcel automated capillary electrophoresis. Detection of a 205 bp fragment indicated presence of P. falciparum. For each run, DNA from reference P. falciparum 3D7 strain and nuclease free water were used as positive and negative controls, respectively. Details of the primers used for nested PCR of 18S rRNA gene in malaria parasites are provided in Additional file 1.
Costs
The main inputs into the study were RDT cassettes and FTA cards at a cost of $0.5 and $1 per collected sample, respectively. The PCR analysis for P falciparum DNA was done at $20 per sample. These costs were met by the research project.
Variables
The variables included diagnostic test results of samples obtained from U5 children who attended study drug shops during the study period. The blood samples were analysed according to four diagnostics strategies, as shown in Table 1.
Background characteristics of the study population, namely, sex, age, if U5 child presented with diarrhoea and fever or history of fever or any child danger sign were collected. For U5 children presenting with cough, their respiratory rate was recorded. Also data on if U5 child was prescribed oral rehydration salts, zinc-sulfate tablets, dispersible amoxicillin tablets and artemether/lumefantrine tablets by the drug seller was obtained.
Data analysis
The sample size was estimated using the Buderer formula [39] for research studies designed to evaluate diagnostic tests. This formula takes into account values of sensitivity and the estimated prevalence which were hypothesized to be 95% and 40%, respectively. A 5% level of statistical significance was assumed, which gave a total sample size of 183 research participants. The sample size was further adjusted for 10% incompleteness rate, hence a total of 203 research participants. Blood samples were obtained from a total of 212 U5 children in the current study. Data for 199 children was available from drug shop registries and only 186 observations were complete for the comparison of drug seller interpretation and laboratory re-reading of RDTs.
Data were double-entered into Epidata software version 3.1 (The EpiData Association, Odense, Denmark), cleaned, checked, coded and then transferred to Stata version 13.0 (Stata Corp., College Station, TX, USA) for analysis. First, categorical characteristics of the U5 children enrolled into the study including sex, if U5 child presented with diarrhea and fever or history of fever or any child danger sign, if U5 child was prescribed any child medicines by the drug seller, were summarized as frequencies and proportions. The numerical variable of age of child was summarized by the median and range. The malaria test results observed on all the four diagnostic strategies; namely, drug seller interpretation of RDT strip (Drug seller), laboratory scientist reading of dried and stored RDT strip (Laboratory scientist), PCR analyses of P. falciparum DNA extracted from the RDT nitrocellulose strip (RDT-PCR) and FTA card (FTA-PCR), were also presented as frequencies and proportions. Second, drug seller compliance to RDT results was assessed based on the drug seller treatment decision for the febrile or malaria case. Third, the authors calculated sensitivity, specificity, positive predictive values (PPV) and negative predictive values (NPV) [with 95% confidence intervals (CI)] of the three diagnostic strategies; namely, drug seller, laboratory scientist and RDT-PCR strategies compared to the FTA-PCR strategy as the reference method.
Fourth, inter-diagnostic strategy variations for both positive and negative readings were expressed by the percentage of overall agreement and Cohen’s kappa (κ) statistic. A 95% confidence interval (95% CI) was calculated for each κ value using the Stata “KAPPA” module [40].
Results
Background characteristics
A total of 212 children aged between 2 and 60 months provided samples for malaria diagnostic testing in the current study. Of these, 103 children presented with cough and were assessed for fast breathing. Data available for 199 U5 children was extracted from the drug shop registries. The median age was 24 months, and slightly more than half (52%) were male. Up to 93% presented with fever or history of fever and 21% presented with diarrhoea (Table 2).
A total of 212 RDT strips were re-read by laboratory scientist. Of these, 13 RDT strip repeat readings by laboratory scientist were not conclusive. Of the remaining 199 malaria RDT strips, 13 cases did not have corresponding drug seller interpretation record, respectively. Hence, data analysis to compare the drug seller interpretation and laboratory scientist re-reading of RDT strips was done on the 186 cases, excluding a total of 26 child cases (13 child cases that did not have record of the drug seller interpretation and an additional 13 child cases that were not conclusive according to the laboratory scientist re-reading) (Table 3).
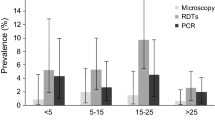
The proportion of the study population reported positive for malaria parasites were 62/199 (31.2%) by drug seller, 59/212 (27.8%) by laboratory scientist, 55/212 (25.9%) by RDT-PCR and 64/212 (30.2%) by FTA-PCR diagnostic strategies, respectively. For the laboratory scientist diagnostic strategy, 6.1% (13/212) (95% CI 3.6, 10.3) RDT strips could not be classified (see Fig. 1).
Comparison between drug seller interpretation and laboratory scientist re-reading of the RDT strips
The overall agreement between the drug seller interpretation and laboratory scientist re-reading of the RDT strip was 93% (n = 186) with kappa value of 0.84 (95% CI 0.75, 0.92) (Table 3). The kappa value was 0.81 (95% CI 0.61, 1.00) among malaria positive cases and 0.41 (95% CI 0.11, 0.70) for negative cases, tested by the FTA-PCR diagnostic strategy (the gold standard) (Table 4).
Of the five cases reported negative by drug seller but positive by laboratory scientist, three tested positive and two negative by FTA-PCR (the gold standard), respectively. Only one out of these five cases was prescribed ACT medicines by drug seller. All the eight cases reported positive by drug seller but negative by laboratory scientist, tested negative by FTA-PCR. Four of these eight cases were prescribed ACT medicines by the drug seller.
Additionally, Table 5 presents the comparison of the two diagnostic strategies of drug seller and laboratory scientist, including the 13 RDT strips that were inconclusive according to the laboratory scientist diagnostic strategy. The agreement between the drug seller and laboratory scientist diagnostic strategy decreased from 93% (95% CI, 88.3, 96.2) to 86.9% (95% CI, 81.4, 91.3). The kappa value decreased from 0.84 (95% CI, 0.75, 0.92) to 0.72 (95% CI, 0.61, 0.83).
Among the 13 child cases that were inconclusive by the laboratory scientist diagnostic strategy, 9 tested malaria positive and 4 were malaria negative by the drug seller diagnostic strategy. However, when tested by the FTA-PCR diagnostic strategy, 10 child cases tested negative while 3 cases tested positive for malaria parasites.
Drug seller compliance with the reported RDT results
The drug seller compliance with the reported RDT results was 92.5% (Table 6). Compliance among malaria positive cases was 91.9% while that among negative cases was 92.7%, respectively. Up to 8.1% malaria positive cases did not receive ACT medicines, while 7.3% negative cases received ACT medicines.
Comparison of the diagnostic strategies against PCR analysis for detection of P. falciparum DNA extracted from FTA card
The sensitivity of the drug seller, laboratory scientist and RDT-PCR diagnostic strategies when compared to FTA-PCR strategy for P. falciparum detection varied from 77% (95% CI 64.3, 86.2) for RDT-PCR to 87% (95% CI 75.8, 94.2) for the laboratory scientist strategy. The specificity of the three diagnostic strategies was > 90% when compared to the gold standard (FTA-PCR). The positive predictive values were 89% for both RDT-PCR and laboratory scientist and 79% for the drug seller strategy. The negative predictive values were > 90% with the highest being 94.3% (95% CI 89.1, 97.5) for the laboratory scientist strategy. The three diagnostic strategies of drug seller, laboratory scientist and RDT-PCR showed high measure of overall agreement > 87% with the gold standard and κ value (kappa statistic) between 0.70 and 0.85 (Table 7). Details of the formulae and numbers used to calculate the sensitivity, specificity, predictive values and likelihood ratios of the diagnostic strategies are provided as supplementary material (Additional file 2). The kappa statistic for the average agreement over all pairs of the diagnostic strategies was 0.74 (95% CI 0.71, 0.76).
Discussion
The findings from this study demonstrate that drug seller interpretation has high concordance with laboratory scientist re-reading of the malaria RDT strips. This finding is similar to that of another Ugandan study [21] that reports 95% agreement between drug seller and research team reading of RDT strips, despite a higher malaria transmission setting than that of the current study. Furthermore, the laboratory scientist diagnostic strategy used as a reference in the current study performs acceptably well against a proven more sensitive diagnostic method—the PCR analysis of P. falciparum DNA extracted from FTA card (FTA-PCR). The high agreement between drug seller and the laboratory scientist strategies in the current study is probably a result of the drug sellers having undergone training in the iCCM intervention study [23]. The iCCM intervention involved hands-on training of the drug sellers on the use of RDT strips to detect presence of malaria parasites, monthly support supervision by a clinical officer or pharmacist and an enhanced diagnostics and medicines supply mechanism [23]. Other studies among community health workers acknowledge that successive practice improves RDT use [41]. Given the relatively low malaria transmission setting, the authors of the current study had hypothesized a higher rate of false positives by drug sellers so as to rationalize their sale of anti-malarials.
The current study also demonstrates high compliance to the RDT results by the drug sellers. This is probably due to the implementation of co-interventions in the drug shops prior to the current study. In addition to drug seller training and support supervision, enhanced supply mechanism and subsidies, communities were sensitized on importance of accepting the RDT test outcomes, as part of the iCCM intervention conducted from February 2014 to September 2015 [23, 34]. The high compliance observed is possibly a residual effect. These findings are consistent with those from similar studies conducted among drug sellers [21, 23], especially for RDT-positive cases [16, 20, 22, 24]. Also studies among community health workers in Tanzania [42], Malawi, Senegal [43] report similarly high compliance levels to RDT results. However, some drug seller studies report variable inappropriate treatment of RDT-negative cases with anti-malarial medicines: 45% [20], 10% [22], 1.5% [21] in each Ugandan study, 7% in Tanzania [24] and 3% in Ghana [16] of the RDT-negative cases are given anti-malarials, respectively. In community health worker studies, greater than 10% of the RDT negative results [10, 11, 44, 45] and up to 20% [46], 30% [47] and 58% [48] were prescribed ACT. Clinical judgement by community health worker is advanced to justify giving ACT to test negative cases [47].
Compliance with observed malaria RDTs results in the current study is also higher than 83% (95% CI 80, 86) reported by Kabaghe et al. in a systematic review that analysed pooled findings from 14 studies involving clinicians and community health workers [49]. In that study, compliance among the malaria positive cases is higher 97% (95% CI 94, 99) while that among negative cases is lower 78% (95% CI 66, 89) [49] than reported in the current study, respectively. The difference in these findings is probably a result of less trained health cadres being more trusting in RDT results while clinicians rely more on symptoms and past experience [50]. For instance, Kabaghe et al. also reports a higher compliance, 95% (95% CI 92, 98) among RDT negative cases among community health workers than 75% (95% 58, 89) among clinicians [49].
In the context of the current study, the drug seller interpretation of the RDTs and subsequent prescription or non-prescription of ACT, does not appear to have been substantially influenced by the drug seller motive to maximize sales. As chronicled in a related publication [34], their primary interest for using the RDTs was the improved reputation within the community as a result of the increased trust in the healthcare provided to the U5 children.
The drug seller diagnostic strategy showed a sensitivity of 82% and specificity of 91% when using the FTA-PCR strategy as a gold standard. PCR is an ideal gold standard as it is based on identification of Plasmodium genus and species specific markers [51]. It has capability to detect malaria parasites at densities as low as 0.002 parasites/µL [52, 53] as compared to RDTs whose detection level varies from 100 to 200 parasites/µL [54]. The lower sensitivity of the drug seller diagnostic strategy observed in the current study could be due to low parasitaemia in some of the study participants. However, individuals with low parasitaemia remain a public health threat as they can contribute to P. falciparum transmission dynamics [52, 53]. Similarly, the sensitivity and specificity of laboratory scientist re-reading of RDT strips though higher than those of drug seller interpretation were 87% and 96%, respectively, when compared to FTA-PCR as a gold standard. The better performance of the laboratory scientist is likely due to differences in health provider characteristics. For instance, subjective interpretation by [55] and poor eye sight of [45] the health provider can lead to poor performance.
In the current study, the observed sensitivity of the laboratory scientist strategy is higher than estimates from similar studies [56, 57]. An evaluation of Pf-HRP2 RDT (CareStart™) using samples from suspected malaria cases aged 1–81 years using PCR as the reference, reports sensitivities ranging from 71% [56], 72% to 75% [57] as compared to 87% in the current study. The difference in findings could be explained by the inclusion of study participants of all ages yet the current study analysed samples taken from children 5 years old or less. Getnet et al. reports that sensitivity of RDTs when compared to PCR as reference is higher in study population under 18 years than older ages [56]. On the contrary, an evaluation of Pf-HRP2 malaria RDTs (MAKROmed™) against PCR as reference among 853 women in Burkina Faso reports almost similar sensitivity of 90% [58] as the current study. The specificity of the laboratory scientist re-reading of the RDT strips against PCR as reference in the current study is the same as observed in north-west Ethiopia (95%) [56], but higher than estimates from western Kenya (82%) [57] and Burkina Faso (65%) [58].
The variability in sensitivity and specificity of Pf-HRP2 RDTs as observed in the current study and other studies [56,57,58,59] warrants a larger scale examination of the magnitude of the misclassification with current RDTs. Moreover, these field estimates are below the minimum WHO thresholds for sensitivity and specificity of 95 and 90% for all malaria species, respectively [60]. Possible explanatory factors for this variation include genetic variation in the histidine rich proteins, batch quality variations [54], Pf-HRP2 persistence in blood following parasite clearance [61], and Pf-HRP2 gene deletions [15, 62, 63]. Other predictors are parasite density, environmental and several host factors, inter-lot variability and performance deterioration, that could result from storage or transportation conditions [6, 8, 54]. Therefore, an external quality assurance scheme for RDT use under field conditions, to detect any failures early and minimize adverse effects of misdiagnosis of malaria is urgently needed. RDT cassettes in routine practice can form the basis of such a scheme as they are an excellent source of Plasmodium DNA especially in the context of drug shops [29,30,31].
The findings show high PPVs of 79% for the drug seller strategy, and 89% each for the laboratory scientist and RDT-PCR diagnostic strategies. The observed PPVs in the current study are consistent with findings from a Tanzanian study in which RDTs of samples from febrile children 2–59 months were compared with PCR as a [64]. However, the PPVs for laboratory scientist and RDT-PCR strategies are higher than 82% that is reported in Wanja et al., except for the PPV of the drug seller strategy which is the same [57]. The NPVs for drug seller, laboratory scientist and RDT-PCR diagnostic strategies in the current study are high (> 90), and above 73–76% that is reported by a Kenyan study [57], but lower than 98.5% that was observed in the Tanzanian study [64]. The difference between predictive values in the current study and other similar studies could be due to differences in the underlying malaria prevalence [65], which in turn is affected by seasonal variations. Given that the prevalence of malaria parasites in the current study population is between 25 and 31% (Fig. 1), the observed predictive values are high and indicative of the probability of disease given the observed results of the test for each of the diagnostic strategies.
The RDT-PCR diagnostic strategy showed low sensitivity of 77% and high specificity of 96% as compared to FTA-PCR strategy. This lower sensitivity of the RDT-PCR could be a result of loss of parasite DNA when the blood sample is lysed and diluted before migration on the nitrocellulose membrane in the RDT cassette [28]. Additional loss could be due to the dispersion on the blotting paper [28]. The amount of DNA recovered is also dependent on the region of the nitrocellulose strip considered for the extraction reaction. Studies show that DNA is concentrated in the region approximately half way between the blood application site and the result lines [66]. Regardless, findings from the current study support the use of RDT cassettes as a source of parasite DNA in place of dry blood spots on FTA cards/filter paper, for an external quality assurance scheme of RDT use in drug shops. Routine collection and PCR analysis of dried RDTs can thus be introduced as part of quality control. In comparison to recovery of Plasmodium DNA from blood smears where contamination can occur during staining, microscopic examination or storage, the risk of contaminating RDT cassettes is minimal [67].
This study has notable limitations. First, the current study compared the RDT based on detection of P. falciparum-specific HRP2 antigen in blood with PCR detection of Plasmodium DNA extracted from dried blood spots. The two diagnostic strategies have inherent differences in their mechanism of detection. Additionally, sensitivity of the Pf-HRP2 RDT decreases at parasite densities below 500 parasites per microlitre of blood [5, 68], while PCR analysis remains sensitive at parasite densities as low as 10 parasites per microliter of blood [69]. Despite this, the authors observed substantial agreement between PCR analysis of Plasmodium DNA from FTA card and drug seller interpretation of RDT strip of 72%, and laboratory scientist re-reading of 83%. The difference in agreement could have been a result of the discrepancy in the mechanism of parasite detection explained above. However, a higher agreement between our initial comparator (laboratory scientist re-reading) and the more sensitive PCR analysis of parasite DNA lends credence to the authors’ approach to evaluating performance of RDT by drug sellers in field conditions.
Second, the nature and context of the encounters between the U5 children who provided blood samples and the drug sellers in the current study is not representative of the typical drug shop setting. The drug sellers in the current study were trained on how to use the malaria RDT, the iCCM treatment algorithm and were monitored and supervised on a monthly basis for 20 months before the evaluation of these malaria diagnostic strategies [23]. This implies that the competency of drug sellers in the current study to interpret and comply with RDT results is probably higher [41] than what would be observed among the typical drug sellers described in other studies [70, 71]. Potentially, drug sellers in the current study were not prone to errors in testing procedures which could have led to poor performance of RDTs [18]. Lastly, health providers in private sector in poor rural settings are heterogeneous, context-specific and operate in constantly changing environments [34].
Third, the current study did not perform malaria microscopy and hence parasite density is not reported. The authors argue that the study setting is homogenous with a relatively low malaria transmission. Hence, no observations can be made about the performance of RDTs at different parasite densities or malaria transmission levels. Other studies have shown that the sensitivity of the RDTs lowers with a decrease in parasite densities [64] and the predictive values for a positive test are affected by the prevalence of the disease [65]. The current study excluded Plasmodium species differentiation and evaluated only the performance of malaria diagnostic strategies in detecting P. falciparum malaria. Since 99% of the malaria infection in Uganda is due to P. falciparum [1, 72], the need for species differentiation was minimal.
Conclusion
Malaria RDTs in the hands of drug sellers in field conditions diagnose malaria among U5 children with acceptable accuracy. Additionally, drug sellers comply with the RDT results, especially when supported with other co-interventions as present in the iCCM intervention. However, the good drug seller performance in malaria diagnosis and compliance to RDT results can be undermined by the high false positivity rate due to low specificity implicit to the Pf-HRP2 RDT platform or caused by drug seller related factors. Further research to test an external quality assurance scheme for RDT use under field conditions based on nucleic acid amplification of Plasmodium DNA recovered from the RDT nitrocellulose strip is, therefore, warranted.
Abbreviations
- ACT:
-
artemisinin-based combination therapy
- CHWs:
-
community health workers
- DNA:
-
deoxyribonucleic acid
- FTA:
-
fast transient analysis
- HRP2:
-
histidine rich protein 2 antigen
- IEC:
-
information, education and communication
- iCCM:
-
integrated community case management intervention
- MoH:
-
Uganda Ministry of Health
- NMCP:
-
National Malaria Control Programme
- NPV:
-
negative predictive value
- ORS:
-
oral rehydration salts
- PCR:
-
polymerase chain reaction
- pLDH:
-
parasite-specific lactate dehydrogenase
- PPV:
-
positive predictive value
- RDT:
-
rapid diagnostic test
- SDG:
-
Sustainable Development Goals
- U5:
-
under-five
- UNICEF:
-
United Nations Children’s Fund
- VHTs:
-
Village Health Teams
- WHO:
-
World Health Organization
- oC:
-
degrees Celsius
References
WHO. World malaria report 2017. Geneva: World Health Organization Global Malaria Programme; 2017.
UNICEF & RBM. Malaria and children: progress in intervention coverage. New York: UNICEF, Division of Communication; 2007.
WHO. Guidelines for the treatment of malaria. 2nd ed. Geneva: World Health Organization; 2010.
WHO. Universal access to malaria diagnostic testing: an operational manual. Geneva: World Health Organization; 2011.
Wongsrichanalai C, Barcus MJ, Muth S, Sutamihardja A, Wernsdorfer WH. A review of malaria diagnostic tools: microscopy and rapid diagnostic test (RDT). Am J Trop Med Hyg. 2007;77:119–27.
Mouatcho JC, Goldring JP. Malaria rapid diagnostic tests: challenges and prospects. J Med Microbiol. 2013;62:1491–505.
Foundation for Innovative New Diagnostics. Malaria rapid diagnostic tests: an implementation guide. Geneva: FIND; 2013.
Miller E, Sikes HD. Addressing barriers to the development and adoption of rapid diagnostic tests in global health. Nanobiomedicine (Rij). 2015;2:e6.
Ajayi IO, Nsungwa-Sabiiti J, Siribie M, Falade CO, Serme L, Balyeku A, et al. Feasibility of malaria diagnosis and management in Burkina Faso, Nigeria, and Uganda: a community-based observational study. Clin Infect Dis. 2016;63:S245–55.
Mukanga D, Tiono AB, Anyorigiya T, Källander K, Konate AT, Oduro AR, et al. Integrated community case management of fever in children under five using rapid diagnostic tests and respiratory rate counting: a multi-country cluster randomized trial. Am J Trop Med Hyg. 2012;87:21–9.
Hamer DH, Brooks ET, Semrau K, Pilingana P, MacLeod WB, Siazeele K, et al. Quality and safety of integrated community case management of malaria using rapid diagnostic tests and pneumonia by community health workers. Pathog Glob Health. 2012;106:32–9.
Phiri TB, Kaunda-Khangamwa BN, Bauleni A, Chimuna T, Melody D, Kalengamaliro H, et al. Feasibility, acceptability and impact of integrating malaria rapid diagnostic tests and pre-referral rectal artesunate into the integrated community case management programme. A pilot study in Mchinji district, Malawi. Malar J. 2016;15:177.
Mendelson M, Rottingen JA, Gopinathan U, Hamer DH, Wertheim H, Basnyat B, et al. Maximising access to achieve appropriate human antimicrobial use in low-income and middle-income countries. Lancet. 2016;387:188–98.
WHO. The use of malaria rapid diagnostic tests; recommendations from the Joint WHO/USAID informal consultation. Geneva: World Health Organization; 2004.
WHO Global Malaria Programme, Malaria Policy Advisory Committee Meeting. Proposal for an Evidence Review Group on field-based quality control of malaria rapid diagnostic tests and investigations into suspected product failure. Geneva: World Health Organization; 2016.
Ansah EK, Narh-Bana S, Affran-Bonful H, Bart-Plange C, Cundill B, Gyapong M. The impact of providing rapid diagnostic malaria tests on fever management in the private retail sector in Ghana: a cluster randomized trial. BMJ. 2015;350:h1019.
Ikwuobe JO, Faragher BE, Alawode G, Lalloo DG. The impact of rapid malaria diagnostic tests upon anti-malarial sales in community pharmacies in Gwagwalada, Nigeria. Malar J. 2013;12:380.
Cohen J, Fink G, Berg K, Aber F, Jordan M, Maloney K, Dickens W. Feasibility of distributing rapid diagnostic tests for malaria in the retail sector: evidence from an implementation study in Uganda. PLoS ONE. 2012;7:e48296.
Awor P, Wamani H, Tylleskar T, Jagoe G, Peterson S. Increased access to care and appropriateness of treatment at private sector drug shops with integrated management of malaria, pneumonia and diarrhoea: a quasi-experimental study in Uganda. PLoS ONE. 2014;9:e115440.
Cohen J, Fink G, Maloney K, Berg K, Jordan M, Svoronos T, et al. Introducing rapid diagnostic tests for malaria to drug shops in Uganda: a cluster-randomized controlled trial. Bull World Health Organ. 2015;93:142–51.
Mbonye AK, Magnussen P, Lal S, Hansen KS, Cundill B, Chandler C, et al. A cluster randomised trial introducing rapid diagnostic tests into registered drug shops in Uganda: impact on appropriate treatment of malaria. PLoS ONE. 2015;10:e0129545.
Awor P, Wamani H, Tylleskar T, Peterson S. Drug seller adherence to clinical protocols with integrated management of malaria, pneumonia and diarrhoea at drug shops in Uganda. Malar J. 2015;14:277.
Kitutu FE, Kalyango JN, Mayora C, Selling KE, Peterson S, Wamani H. Integrated community case management by drug sellers influences appropriate treatment of paediatric febrile illness in South Western Uganda: a quasi-experimental study. Malar J. 2017;6:425.
Maloney K, Ward A, Krenz B, Petty N, Bryson L, Dolkart C, et al. Expanding access to parasite-based malaria diagnosis through retail drug shops in Tanzania: evidence from a randomized trial and implications for treatment. Malar J. 2017;16:6.
Aung T, White C, Montagu D, McFarland W, Hlaing T, Khin HS, et al. Improving uptake and use of malaria rapid diagnostic tests in the context of artemisinin drug resistance containment in eastern Myanmar: an evaluation of incentive schemes among informal private healthcare providers. Malar J. 2015;14:105.
Singlovic J, Ajayi IO, Nsungwa-Sabiiti J, Siribie M, Sanou AK, Jegede AS, et al. Compliance with malaria rapid diagnostic testing by community health workers in 3 malaria-endemic countries of sub-Saharan Africa: an observational study. Clin Infect Dis. 2016;63:S276–82.
Boyce MR, O’Meara WP. Use of malaria RDTs in various health contexts across sub-Saharan Africa: a systematic review. BMC Public Health. 2017;17:470.
Veron V, Carme B. Recovery and use of Plasmodium DNA from malaria rapid diagnostic tests. Am J Trop Med Hyg. 2006;74:941–3.
Morris U, Aydin-Schmidt B, Shakely D, Martensson A, Jornhagen L, Ali AS, et al. Rapid diagnostic tests for molecular surveillance of Plasmodium falciparum malaria-assessment of DNA extraction methods and field applicability. Malar J. 2013;12:106.
Ishengoma DS, Lwitiho S, Madebe RA, Nyagonde N, Persson O, Vestergaard LS, et al. Using rapid diagnostic tests as source of malaria parasite DNA for molecular analyses in the era of declining malaria prevalence. Malar J. 2011;10:6.
Engwa GA, Achundoh OA, Mbacham WF. Rapid Diagnostic Test Cassette: a source of DNA for malaria diagnosis by PCR and a quality control tool for the test performance. Acad J Interdisciplinary Studies. 2013;2:69–75.
Uganda Bureau of Statistics (UBOS), ICF International. Uganda malaria indicator survey 2014–15: key Indicators. Kampala and Rockville: Uganda Bureau of Statistics (UBOS) and ICF International; 2015.
Kamya MR, Arinaitwe E, Wanzira H, Katureebe A, Barusya C, Kigozi SP, et al. Malaria transmission, infection, and disease at three sites with varied transmission intensity in Uganda: implications for malaria control. Am J Trop Med Hyg. 2015;92:903–12.
Kitutu FE, Mayora C, Johansson EW, Peterson S, Wamani H, Bigdeli M, et al. Health system effects of implementing integrated community case management (iCCM) intervention in private retail drug shops in South Western Uganda: a qualitative study. BMJ Glob Health. 2017;2:1–13.
Baidjoe A, Stone W, Ploemen I, Shagari S, Grignard L, Osoti V, et al. Combined DNA extraction and antibody elution from filter papers for the assessment of malaria transmission intensity in epidemiological studies. Malar J. 2013;12:272.
Choi EH, Lee SK, Ihm C, Sohn YH. Rapid DNA extraction from dried blood spots on filter paper: potential applications in biobanking. Osong Public Health Res Perspect. 2014;5:351–7.
Cnops L, Boderie M, Gillet P, Van Esbroeck M, Jacobs J. Rapid diagnostic tests as a source of DNA for Plasmodium species-specific real-time PCR. Malar J. 2011;10:67.
Hwang S-Y, Kim S-H, Lee G-Y, Hang VTT, Moon C-S, Shin JH, et al. A novel real-time PCR assay for the detection of Plasmodium falciparum and Plasmodium vivax malaria in low parasitized individuals. Acta Trop. 2011;120:40–5.
Buderer NM. Statistical methodology: I. Incorporating the prevalence of disease into the sample size calculation for sensitivity and specificity. Acad Emerg Med. 1996;3:895–900.
Gould WW. stata49: interrater agreement. Stata Technical Bull. 1998;7:20–8.
Harvey SA, Jennings L, Chinyama M, Masaninga F, Mulholland K, Bell DR. Improving community health worker use of malaria rapid diagnostic tests in Zambia: package instructions, job aid and job aid-plus-training. Malar J. 2008;7:160.
Masanja IM, Selemani M, Amuri B, Kajungu D, Khatib R, Kachur S, et al. Increased use of malaria rapid diagnostic tests improves targeting of anti-malarial treatment in rural Tanzania: implications for nationwide rollout of malaria rapid diagnostic tests. Malar J. 2012;11:221.
Ruizendaal E, Dierickx S, Peeters Grietens K, Schallig HD, Pagnoni F, Mens PF. Success or failure of critical steps in community case management of malaria with rapid diagnostic tests: a systematic review. Malar J. 2014;13:229.
Yeboah-Antwi K, Pilingana P, Macleod WB, Semrau K, Siazeele K, Kalesha P, Hamainza B, Seidenberg P, Mazimba A, Sabin L, et al. Community case management of fever due to malaria and pneumonia in children under five in Zambia: a cluster randomized controlled trial. PLoS Med. 2010;7:e1000340.
Mukanga D, Babirye R, Peterson S, Pariyo GW, Ojiambo G, Tibenderana JK, et al. Can lay community health workers be trained to use diagnostics to distinguish and treat malaria and pneumonia in children? Lessons from rural Uganda. Trop Med Int Health. 2011;16:1234–42.
Ndiaye Y, Ndiaye JL, Cisse B, Blanas D, Bassene J, Manga IA, et al. Community case management in malaria: review and perspectives after four years of operational experience in Saraya district, south-east Senegal. Malar J. 2013;12:240.
Elmardi KA, Malik EM, Abdelgadir T, Ali SH, Elsyed AH, Mudather MA, et al. Feasibility and acceptability of home-based management of malaria strategy adapted to Sudan’s conditions using artemisinin-based combination therapy and rapid diagnostic test. Malar J. 2009;8:39.
Chinkhumba J, Skarbinski J, Chilima B, Campbell C, Ewing V, San Joaquin M, et al. Comparative field performance and adherence to test results of four malaria rapid diagnostic tests among febrile patients more than five years of age in Blantyre, Malawi. Malar J. 2010;9:209.
Kabaghe AN, Visser BJ, Spijker R, Phiri KS, Grobusch MP, van Vugt M. Health workers’ compliance to rapid diagnostic tests (RDTs) to guide malaria treatment: a systematic review and meta-analysis. Malar J. 2016;15:163.
Mubi M, Kakoko D, Ngasala B, Premji Z, Peterson S, Bjorkman A, et al. Malaria diagnosis and treatment practices following introduction of rapid diagnostic tests in Kibaha District, Coast Region, Tanzania. Malar J. 2013;12:293.
Singh B, Bobogare A, Cox-Singh J, Snounou G, Abdullah MS, Rahman HA. A genus- and species-specific nested polymerase chain reaction malaria detection assay for epidemiologic studies. Am J Trop Med Hyg. 1999;60:687–92.
Harris I, Sharrock WW, Bain LM, Gray KA, Bobogare A, Boaz L, et al. A large proportion of asymptomatic Plasmodium infections with low and sub-microscopic parasite densities in the low transmission setting of Temotu Province, Solomon Islands: challenges for malaria diagnostics in an elimination setting. Malar J. 2010;9:254.
Okell LC, Ghani AC, Lyons E, Drakeley CJ. Submicroscopic infection in Plasmodium falciparum-endemic populations: a systematic review and meta-analysis. J Infect Dis. 2009;200:1509–17.
WHO. Malaria rapid diagnostic test performance: summary results of WHO MALARIA RDT product testing: rounds 1–6 (2008–2015). Geneva: World Health Organization; 2011.
Counihan H, Harvey SA, Sekeseke-Chinyama M, Hamainza B, Banda R, Malambo T, et al. Community health workers use malaria rapid diagnostic tests (RDTs) safely and accurately: results of a longitudinal study in Zambia. Am J Trop Med Hyg. 2012;87:57–63.
Getnet G, Getie S, Srivastava M, Birhan W, Fola AA, Noedl H. Diagnostic performance of rapid diagnostic tests for the diagnosis of malaria at public health facilities in north-west Ethiopia. Trop Med Int Health. 2015;20:1564–8.
Wanja EW, Kuya N, Moranga C, Hickman M, Johnson JD, Moseti C, et al. Field evaluation of diagnostic performance of malaria rapid diagnostic tests in western Kenya. Malar J. 2016;15:456.
Singer LM, Newman RD, Diarra A, Moran AC, Huber CS, Stennies G, et al. Evaluation of a malaria rapid diagnostic test for assessing the burden of malaria during pregnancy. Am J Trop Med Hyg. 2004;70:481–5.
Laurent A, Schellenberg J, Shirima K, Ketende SC, Alonso PL, Mshinda H, et al. Performance of HRP-2 based rapid diagnostic test for malaria and its variation with age in an area of intense malaria transmission in southern Tanzania. Malar J. 2010;9:294.
WHO. New perspectives: malaria diagnosis. Report of joint WHO/USAID informal consultation 25–27 October 1999. Report No. WHO/CDS/RBM/2000.14, WHO/MAL/2000.1091. Geneva: World Health Organization; 1999.
Dalrymple U, Arambepola R, Gething PW, Cameron E. How long do rapid diagnostic tests remain positive after anti-malarial treatment? Malar J. 2018;17:228.
Cheng Q, Gatton ML, Barnwell J, Chiodini P, McCarthy J, Bell D, et al. Plasmodium falciparum parasites lacking histidine-rich protein 2 and 3: a review and recommendations for accurate reporting. Malar J. 2014;13:283.
Berhane A, Russom M, Bahta I, Hagos F, Ghirmai M, Uqubay S. Rapid diagnostic tests failing to detect Plasmodium falciparum infections in Eritrea: an investigation of reported false negative RDT results. Malar J. 2017;16:105.
Mahende C, Ngasala B, Lusingu J, Yong TS, Lushino P, Lemnge M, et al. Performance of rapid diagnostic test, blood-film microscopy and PCR for the diagnosis of malaria infection among febrile children from Korogwe District, Tanzania. Malar J. 2016;15:391.
Fletcher RH, Fletcher SW. Diagnosis. In: Fletcher RH, Fletcher SW, editors. Clinical epidemiology: the essentials. 4th ed. USA: Lippincott Williams & Wilkins; 2005. Chapt 3:35–58.
WWARN. Molecular module—preparation of rapid diagnostic tests (RDTs) for DNA extraction. vol. v1.1. 2011. World Wide Antimalarial Resistance Network (WWARN). http://www.wwarn.org. Accessed 22 May 2018.
Aubouy A, Carme B. Plasmodium DNA contamination between blood smears during Giemsa staining and microscopic examination. J Infect Dis. 2004;190:1335–7.
Forney JR, Wongsrichanalai C, Magill AJ, Craig LG, Sirichaisinthop J, Bautista CT, et al. Devices for rapid diagnosis of Malaria: evaluation of prototype assays that detect Plasmodium falciparum histidine-rich protein 2 and a Plasmodium vivax-specific antigen. J Clin Microbiol. 2003;41:2358–66.
Hanscheid T, Grobusch MP. How useful is PCR in the diagnosis of malaria? Trends Parasitol. 2002;18:395–8.
Awor P, Wamani H, Bwire G, Jagoe G, Peterson S. Private sector drug shops in integrated community case management of malaria, pneumonia, and diarrhea in children in Uganda. Am J Trop Med Hyg. 2012;87:92–6.
Liow E, Kassam R, Sekiwunga R. How unlicensed drug vendors in rural Uganda perceive their role in the management of childhood malaria. Acta Trop. 2016;164:455–62.
Talisuna AO, Noor AM, Mundia CW, Otieno V, Mitto B, Amratia P, et al. An epidemiological profile of malaria and its control in Uganda. Analysis and report funded by Roll Back Malaria and Department for International Development-UK, September 2013.
Authors’ contributions
FEK, HW, SP and AM designed and conceptualized the study. FEK and FAK conducted the experiments. FEK entered, cleaned, prepared, and conducted preliminary analysis of the data. FEK, SP and AM interpreted data and contributed to data analysis. FEK, KES and AM contributed to interpretation of findings. FEK wrote the first draft of the paper. FEK, HW, KES, FAK, RBK, SP, JNK and AM reviewed, revised and contributed to writing to the paper. FEK, HW, KES, FAK, RBK, SP, JNK and AM read and met the ICMJE criteria for authorship. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank drug shop owners, attendants and care-seekers who participated in the study, district health team of Mbarara district and the staff of the molecular laboratory at the department of medical microbiology, Makerere University for supporting the implementation of the study.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets during and/or analysed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The research and ethics committees at Makerere University School of Public Health (IRB00011353), Uganda National Council of Science and Technology (HS1385) and World Health Organization reviewed and approved the study. Informed consent was obtained from drug sellers and a waiver of written informed consent was granted for care-seekers and under-five children.
Funding
The study was supported by WHO Alliance for Health Policy and Systems Research, Einhorn Family Foundation, Pehr Lagermans Family, Sweden, Swedish Science Council and Uppsala University. These organizations had no role in the design, implementation interpretation nor reporting of the findings. FEK, HW FAK, RBK and JNK receive salary support from Makerere University while KES, FEK and AM received salary support from Uppsala University.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1.
Primers for nested PCR of 18S rRNA gene in malaria parasites.
Additional file 2.
The calculations of sensitivity, specificity, predictive values and likelihood ratios of the diagnostic strategies and respective formulae used.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kitutu, F.E., Wamani, H., Selling, K.E. et al. Can malaria rapid diagnostic tests by drug sellers under field conditions classify children 5 years old or less with or without Plasmodium falciparum malaria? Comparison with nested PCR analysis. Malar J 17, 365 (2018). https://doi.org/10.1186/s12936-018-2508-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-018-2508-x