Abstract
Introduction
Rheumatoid arthritis (RA) is a multifactorial autoimmune disease in which genetic and environmental factors interact in the etiology. In this study, we investigated whether smoking and HLA-DRB1 shared-epitope (SE) alleles interact differently in the development of the two major subgroups of rheumatoid arthritis (RA), anti-citrullinated proteins antibody (ACPA)-positive and ACPA-negative disease, in a multiethnic population of Asian descent.
Methods
A case-control study comprising early diagnosed RA cases was carried out in Malaysia between 2005 and 2009. In total, 1,076 cases and 1,612 matched controls participated in the study. High-resolution HLA-DRB1 genotyping was performed for shared-epitope (SE) alleles. All participants answered a questionnaire on a broad range of issues, including smoking habits. The odds ratio (OR) of developing ACPA-positive and ACPA-negative disease was calculated for smoking and the presence of any SE alleles separately. Potential interaction between smoking history (defined as "ever" and "never" smoking) and HLA-DRB1 SE alleles also was calculated.
Results
In our multiethnic study, both the SE alleles and smoking were associated with an increased risk of developing ACPA-positive RA (OR SE alleles, 4.7; 95% confidence interval (CI), 3.6 to 6.2; OR smoking, 4.1; 95% CI, 1.9 to 9.2). SE-positive smokers had an odds ratio of ACPA-positive RA of 25.6 (95% CI, 10.4 to 63.4), compared with SE-negative never-smokers. The interaction between smoking and SE alleles was significant (attributable proportion due to interaction (AP) was 0.7 (95% CI, 0.5 to 1.0)). The HLA-DRB1*04:05 SE allele, which is common in Asian populations, but not among Caucasians, was associated with an increased risk of ACPA-positive RA, and this allele also showed signs of interaction with smoking (AP, 0.4; 95% CI, -0.1 to 0.9). Neither smoking nor SE alleles nor their combination was associated with an increased risk of ACPA-negative RA.
Conclusions
The risk of developing ACPA-positive RA is associated with a strong gene-environment interaction between smoking and HLA-DRB1 SE alleles in a Malaysian multiethnic population of Asian descent. This interaction seems to apply also between smoking and the specific HLA-DRB1*04:05 SE allele, which is common in Asian populations but not in Caucasians.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a multifactorial autoimmune disease in which genetic and environmental factors interact in the etiology of the disease [1, 2]. The strongest gene association is considered to be within the human leukocyte antigen (HLA) region, particularly the HLA-DRB1 genes. Multiple HLA-DRB1 alleles encoding the shared epitope (SE) at amino acid positions 70 to 74 in the third hypervariable region of the DRβ1 molecules are associated with a higher risk for RA [3].
Relatively little is known about environmental factors that may contribute to the disease, except smoking, which is the main environmental factor that has consistently been related to an increased risk of RA [4–11]. Recent data revealed a strong gene-environment interaction between smoking and SE alleles in the risk of ACPA-positive RA. However, the majority of studies undertaken so far have focused on the Caucasian populations, with consistent findings [5–8, 10–13]. In contrast, a cross-sectional study of African Americans with early RA did not find an association between smoking and ACPA-positive RA [14]. A study of an Asian population on prevalent RA cases demonstrated that the combination of SE alleles and smoking was associated with risk of RA, regardless of ACPA status [4]. A gene-environment interaction between smoking and SE alleles was, however, observed only for ACPA-positive RA in this study.
In the Malaysian Epidemiological Investigation of Rheumatoid Arthritis (MyEIRA) case-control study, we recently reported that HLA-DRB1 SE alleles were consistently associated with ACPA-positive RA in three Asian ethnic populations [15]. Furthermore, our group also demonstrated that smoking is associated with RA development and that this effect is restricted to the ACPA-positive RA subset [16]. However, the question whether the HLA-DRB1 SE alleles and smoking interacts in providing an increased risks for ACPA-positive RA remains to be answered in our non-Caucasian population. This question is of particular relevance, as the occurrence of different HLA-DRB1 SE alleles is different between Asian and Caucasian populations.
In the present study, we used the first large Asian case-control study performed in Malaysia involving early RA to investigate the interaction between smoking and HLA-DRB1 SE alleles (including those that are rare in Caucasian populations) regarding risk of disease.
Materials and methods
Study design
The source of data for our investigation was the MyEIRA case-control study, in which the subjects were individuals aged 18 to 70 years in Peninsular Malaysia. The recruitment period for cases and controls was between August 2005 and December 2009.
Identification of cases and controls
The details of the MyEIRA study have been described elsewhere [16]. In brief, patients with early RA were identified from nine centers throughout Peninsular Malaysia. All cases were diagnosed by rheumatologists according to the 1987 revised American College of Rheumatology criteria [17]. The clinical and radiographic data were recorded in a binary fashion (present or absent). For each case, a population control was randomly selected matched by age, sex, and residential area. In addition, hospital-based controls were recruited in the first 2 years of the study period. These were selected among hospital staff, people who accompanied patients, and patients without any underlying autoimmune diseases. Participation in the study was voluntary, and if an eligible control decided not to participate, another control was selected by using the same procedure. Written consent was obtained from all participants. The Medical Research and Ethnics Committee, Ministry of Health, Malaysia, approved the study.
Data collection and blood sampling
Information about environmental exposures was collected from cases and controls by means of an identical questionnaire used in a face-to-face interview by well-trained interviewers. Cases and controls were also asked to provide a blood sample. Of the 1,166 identified early RA cases, 1,076 (92%) completed a questionnaire. In total, 2,112 controls were identified in the study, and the participation proportion was 76%, resulting in 1,612 controls available for analysis. Sera for serologic analysis and cells for DNA preparation were obtained from all the participating subjects.
DNA extraction and HLA-DRB1 genotyping
White cells were separated by using Ficoll Hypaque, and the DNA was extracted by using the QIAamp DNA Blood Mini Kit from Qiagen (Hilden, Germany). All DNA was stored at -20°C until tested. HLA-DRB1 two-digit and 4-digit genotyping were performed by the PCR-SSO method described elsewhere [15]. The overall genotyping success rate was 99.9%. DNA samples from two RA cases were of poor quality in genotyping and therefore excluded from the statistical evaluation. The HLA-DRB1 shared epitope (SE) alleles group was defined by HLA-DRB1*01:01, *01:02, *01:07, *04:01, *04:04, *04:05, *04:08, *04:10, *10:01, and *10:03. More than 95% of the HLA-DRB1*10 subtypes were HLA-DRB1*10:01. A preponderance of HLA-DRB1 SE alleles occurred in the RA cases compared with controls (40% versus 16%). Only 46 (4.4%) of 1,054 RA patients carried two copies of HLA-DRB1 SE alleles. Thus, we decided to limit the analysis to investigate the influence from any SE allele (either one or two copies of SE alleles) on RA risk.
Autoantibody measurements
Anti-citrullinated peptide antibody (ACPA) was quantified by using the anti-CCP ELISA kits (Immunoscan-RA, Malmö, Sweden) for all subjects [15]. An antibody level ≥25 AU/ml was regarded as ACPA positive. For the determination of IgM and IgG rheumatoid factors, we used the ELISA kits of Immuno-Biological Laboratories, Hamburg, Germany. An antibody level > 15 IU/ml was defined as positive.
Definition of smoking status
Cases and controls were classified as "ever-smokers" and "never-smokers," according to their reported smoking habits. In brief, ever-smokers were defined as those who smoked before or during the index year (the time point at which RA symptoms started and the corresponding time point among the matched controls), as described previously [16]. Never-smokers are those who had never smoked before or during the index year.
Statistical analysis
In the analyses, data from cases and their matched controls were used. Twenty cases and 196 controls lacked information from a matched control/case, and therefore in total, 1,056 cases and 1,416 controls (1,056 matched population controls and 360 matched hospital controls) were retained in the analyses. Smoking history was obtained from 1,006 patients with RA (95.3%) and from 1,325 control subjects (93.6%). Of these, 79 of the cases had ever smoked (70 men and nine women), and 65 of the control subjects were ever-smokers (60 men and five women) (Table 1).
The odds ratio (OR) and 95% confidence interval (95% CI) of developing ACPA-positive RA, ACPA-negative RA, and RA in total, associated with smoking habits and the presence of SE alleles, were calculated by using conditional logistic regression. Never-smokers without SE-alleles were used as reference group. HLA-DRB1*04:05 is the most common allele within the HLA-DRB1*04 group in our Malaysian population (the allelic frequency was 15.5% among cases and 5.7% among controls). Subsequently, we performed additional analyses by stratifying the SE-positive individuals into two groups: the HLA-DRB1*04:05 group and the non-HLA-DRB1*04:05 group (defined by HLA-DRB1*01:01, *01:02, *01:07, *04:01, *04:04, *04:08, *04:10, *10:01, and *10:03). Cases (n = 13) and controls (n = 1) carrying HLA-DRB1*04:05 as first allele and a non-HLA-DRB1*04:05 SE as second allele were not included in this analysis.
Interaction between smoking habits and the presence of SE alleles was evaluated as a departure from the additivity of effects and was estimated by calculating the attributable proportion due to interaction (AP) together with the 95% CI [18].
Potential confounding factors (that is, formal educational level (categorized as no formal education, primary education, secondary education or college/university)) and ethnicity (categorized as Malay, Chinese, Indian, and Others), were adjusted for in all analyses. The SAS software, version 9.2 (SAS Institute, Cary, NC, USA) was used for computations.
Results
Characteristics of the subjects
In this report, the 2,110 participants (n = 905 RA cases and 1,205 controls) were women, and 362 were men (n = 151 RA cases and n = 211 controls). The median duration of time from disease onset to inclusion in the study was 1 year, with an interquartile range (IQR) of 2 years for both men and women. Radiographic data were recorded as presence or absence of hand-joint erosions. In total, 974 radiographic erosion data were available in the present study. Of these, 169 (17.4%) of 974 patients had erosive RA. Extraarticular features were present in 114 (11.7%) patients with RA: 52 (5.3%) patients had sicca syndrome; 28 (2.9%) patients had lung fibrosis; 19 (2.0%) patients had rheumatoid nodules; 14 (1.4%) patients had secondary Sjögren syndrome; and one patient had vasculitis. Ever-smoking was more frequent in men for both cases (48%) and controls (28%), as compared with women (1% among cases and 0.4% among controls). In total, 64% of the cases were ACPA positive, and 40% of the cases were carriers of SE alleles. Of the 680 ACPA-positive RA cases, 344 (51%) individuals carried SE alleles; 51.2% and 51.7% of RA patients were IgM RF-positive and IgG RF-positive, respectively. The distribution of ethnic groups (Malays, Chinese, Indians, and other subethnicities) is presented in Table 1. Men were slightly older than women. The proportion with higher education was higher among the controls than the cases (74% versus 66%, data not shown).
Smoking and the risk of ACPA-positive/-negative RA
The odds ratio of developing ACPA-positive RA was 4.1 (95% CI, 1.9 to 9.2), among ever-smokers compared with never-smokers (Table 2). This increased risk was seen in both men and women, but the number of smokers among women was small. No association was found between smoking and the risk of developing ACPA-negative RA (OR = 0.7; 95% CI, 0.3 to 2.0).
HLA-DRB1 SE alleles and the risk of ACPA-positive/negative RA
Carriers of HLA-DRB1 SE alleles had an increased risk of developing ACPA-positive RA (OR = 4.7; 95% CI, 3.6 to 6.2), compared with those without SE alleles (Table 3). When the HLA-DRB1*04:05 allele group was analyzed separately, this subgroup also showed an association with an increased risk of ACPA-positive RA (OR = 6.5; 95% CI, 4.9 to 8.7). No increased risk of ACPA-negative RA was found in individuals carrying any SE allele (OR = 1.2; 95% CI, 0.8 to 1.7), or the HLA-DRB1*04:05 allele when this was investigated separately (OR = 1.2; 95% CI, 0.8 to 1.9).
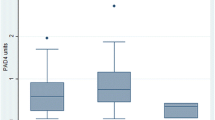
Interaction between smoking and SE alleles in relation to ACPA-positive/-negative RA
We observed an increased risk of ACPA-positive RA among ever-smokers without SE alleles (OR = 3.1; 95% CI, 1.7 to 5.7), compared with never-smokers without SE alleles (Table 4). In never-smokers with SE alleles, the OR for ACPA-positive RA was 4.4 (95% CI, 3.5 to 5.6); compared with never-smokers without the SE allele. A dramatically increased risk for ACPA-positive RA was seen in individuals who were both smokers and HLA-DRB1 SE positive (OR = 25.6; 95% CI, 10.4 to 63.4), and here we also observed a statistically significant gene-environment interaction between smoking and the HLA-DRB1 SE (AP = 0.7; 95% CI, 0.5 to 1.0; Figure 1). The combination of smoking and the HLA-DRB1*04:05 SE allele was also associated with an increased risk of ACPA-positive RA (OR = 12.9; 95% CI, 4.7 to 35.3; Table 5), and signs of interaction were seen, albeit statistically insignificant (AP = 0.4; 95% CI, -0.1 to 0.9).
The same pattern of interaction was observed when RF (IgM and IgG) was used for the subdivision of RA cases: HLA-DRB1 SE alleles were found to interact significantly with smoking only for RF-positive RA (for IgM RF, OR = 23.5; 95% CI, 9.5 to 57.8; AP = 0.7, 95% CI, 0.6 to 0.9; and for IgG RF, OR = 19.4; 95% CI, 7.9 to 47.8; AP = 0.7, 95% CI, 0.5 to 0.9), but not for the RF-negative RA subgroup (data not shown).
We also separately analyzed data only from the largest ethnic group in our study, the Malays. Smokers carrying SE alleles had a remarkably increased risk of ACPA-positive RA (OR = 32.0; 95% CI, 8.7 to 117.9; AP = 0.8; 95% CI, 0.5 to 1.1), compared with SE-negative never-smokers. The results for the two other major ethnic groups, Chinese and Indians, showed the same pattern but, because of the small number of observations, the precision was very low.
Discussion
Two principal findings are presented in this case-control study. First, both smoking and the SE alleles were associated mainly with an increased risk of ACPA-positive RA. Second, we demonstrated a strong gene-environment interaction between smoking and SE alleles, which was restricted to only ACPA-positive RA in a multiethnic Malaysian population of Asian descent. Interestingly, this interaction seems to appear also between smoking and the SE allele HLA-DRB1*04:05, common in Asian but not among Caucasian subjects. Thus, our data extend previous results based on the Caucasian populations [6, 7, 10, 11, 13] to be observed also in an Asian population.
Our current study was designed as a case-control study with primarily early RA cases with the aim of investigating the impact of environmental, life-style, and genetic factors on the development of RA in an Asian population. The study was performed with the Swedish EIRA study as prototype [11] and has the advantage of being a large case-control study involving RA cases with short disease duration. A possible disadvantage with a case-control study using retrospectively collected data is the risk of recall bias, which occurs if the cases recall their previous exposure differently from the controls. Therefore, we included only cases with short disease duration to facilitate more-accurate information about their smoking habits before disease onset. Furthermore, in a previous report on smoking and the risk of RA, we performed a separate analysis on cases with symptom durations of less than 1 year to investigate possible recall bias [16]. In that analysis, ever-smoking was associated with an increased risk of ACPA-positive RA, which was in accordance with the results for which information from all cases was used.
In this report, we included both hospital- and population-based controls. Hospital controls might introduce selection bias if they do not reflect the smoking habits in the study base that generated the cases in our study. To elucidate this potential bias, we conducted separate analyses based on hospital and population controls, respectively. The results between these analyses were consistent, and thus we decided to merge the two control groups into one control group in the analyses to increase the power.
We previously demonstrated a profound interaction between smoking and SE alleles concerning risk of developing ACPA-positive RA in the Swedish EIRA population-based case-control study. We also provided evidence that cigarette smoking may induce citrullination in cells from the lungs [11]. Subsequent studies replicated and extended these findings, although mainly among Caucasians [5, 6, 8–10, 19]. Similarly, smoking and SE alleles were also associated with the risk of developing RA, irrespective of RF or ACPA status in a Korean case-control study based on prevalent RA cases. However, interaction between smoking and SE alleles was statistically significant only for autoantibody-positive RA [4].
The genetic heterogeneity in our multiethnic study population is a major concern. We therefore performed stratified analyses by ethnicity, but the number of observations was too small to permit a meaningful analysis, except for the Malays. However, all the ethnic groups were showing similar trends toward the risk developing RA. Therefore, we decided to analyze them together to raise the statistical power for analyzing the exposures in question. As a result, we demonstrated a strong gene-environment interaction between smoking and SE alleles in ACPA-positive RA. These results are in accordance with those of other studies [10, 11, 13]. Nevertheless, these data are also in line with our previously reported hypothesis that cigarette smoking modulates the loss of tolerance to citrullinated autontigens occurring in SE-positive individuals [11].
Intriguingly, comparisons of populations with different genetic backgrounds but similar environmental exposure (smoking) can shed light on the general influence of non-genetic factors. Some SE alleles, like HLA-DRB1*04:05 and HLA-DRB1*10:01, are common in Asia [15] but not in Caucasian populations, in which instead HLA-DRB1*04:01 and HLA-DRB1*04:04 are common. An article recently published by our group demonstrated that, regardless of fine specificity, all HLA-DRB1 SE alleles strongly interacted with smoking in the development of ACPA-positive RA in the Swedish Caucasian population [7]. The HLA-DRB1*04:05 allele is the most common SE-encoding HLA-DRB1*04 subtype associated with RA reported in Asian populations, but is rare in Caucasian populations [15, 20–22]. However, we are not aware of any published studies on interaction between smoking and distinct SE alleles in the development of RA defined by ACPA-subsets in multiethnic Asian populations. We observed that ever-smokers carrying the HLA-DRB1*04:05 allele had a 12.9-fold increased risk of ACPA-positive RA, and that signs of interaction were found between smoking and HLA-DRB1*04:05, although the interaction was not statistically significant (AP = 0.4; 95% CI, -0.1 to -0.9). Additional studies are needed for replication of these findings in other populations.
Several studies have reported positive interaction between SE and the cumulative dose of smoking and RA risk [9, 19]. In this report, that kind of interaction analysis was not possible to perform because of small number of heavy smokers with SE alleles.
Finally, in the Swedish EIRA study, we found that smoking was responsible for approximately 35% of the ACPA-positive RA cases [23]. Although the female smoking prevalence was much lower in the present study, we estimated that smoking was responsible for approximately 8% of the ACPA-positive RA cases (1% for women, 45% for men). Because an increasing smoking trend is found in women in Asia, public health measures to prevent smoking are of importance.
Conclusions
In conclusion, our findings indicate a gene-environment interaction between smoking and SE alleles in the development of ACPA-positive RA, but not in the development of ACPA-negative RA in a multiethnic population of Asian descent. This interaction also seems to apply between smoking and an HLA-DRB1 SE allele (HLA-DRB1*04:05) common in Asian populations but not in Caucasians. Our data are in accordance with previous findings among Caucasians and thus extend the basis for RA pathogenesis hypothesis involving genetic and environmental factors. Taken together, these findings may provide a new insight into the interplay between two major RA-susceptible risk factors (smoking and SE alleles) along one or more biologic pathways, which are common for the RA disease itself regardless of population origins.
Abbreviations
- ACPAs:
-
anti-citrullinated protein antibodies
- ACR:
-
American College of Rheumatology
- anti-CCP:
-
anti-cyclic citrullinated peptide antibody
- AP:
-
attributable proportion
- AU:
-
arbitrary unit
- CI:
-
confidence interval
- DNA:
-
deoxyribonucleic acid
- ELISA:
-
enzyme-linked immunosorbent assay
- HLA-DRB1 :
-
human leukocyte antigen-DR beta chain 1
- IQR:
-
interquartile range
- MyEIRA:
-
Malaysian Epidemiological Investigation of Rheumatoid Arthritis
- OR:
-
odds ratio
- PCR-SSO:
-
polymerase chain reaction-sequence-specific oligonucleotide
- RA:
-
rheumatoid arthritis
- SAS:
-
statistical analysis system
- SE:
-
shared epitope
- Swedish EIRA:
-
Swedish Epidemiological Investigation of Rheumatoid Arthritis.
References
Klareskog L, Gregersen PK, Huizinga TW: Prevention of autoimmune rheumatic disease: state of the art and future perspectives. Ann Rheum Dis. 2010, 69: 2062-2066.
Klareskog L, Padyukov L, Rönnelid J, Alfredsson L: Genes, environment and immunity in the development of rheumatoid arthritis. Curr Opin Immunol. 2006, 18: 650-655.
Bowes J, Barton A: Recent advances in the genetics of RA susceptibility. Rheumatology (Oxford). 2008, 47: 399-402.
Bang SY, Lee KH, Cho SK, Lee HS, Lee KW, Bae SC: Smoking increases rheumatoid arthritis susceptibility in individuals carrying the HLA-DRB1 shared epitope, regardless of rheumatoid factor or anti-cyclic citrullinated peptide antibody status. Arthritis Rheum. 2010, 62: 369-377.
Lee HS, Irigoyen P, Kern M, Lee A, Batliwalla F, Khalili H, Wolfe F, Lum RF, Massarotti E, Weisman M, Bombardier C, Karlson EW, Criswell LA, Vlietinck R, Gregersen PK: Interaction between smoking, the shared epitope, and anti-cyclic citrullinated peptide: a mixed picture in three large North American rheumatoid arthritis cohorts. Arthritis Rheum. 2007, 56: 1745-1753.
Linn-Rasker SP, van der Helm-van Mil AH, van Gaalen FA, Kloppenburg M, de Vries RR, le Cessie S, Breedveld FC, Toes RE, Huizinga TW: Smoking is a risk factor for anti-CCP antibodies only in rheumatoid arthritis patients who carry HLA-DRB1 shared epitope alleles. Ann Rheum Dis. 2006, 65: 366-371.
Lundström E, Källberg H, Alfredsson L, Klareskog L, Padyukov L: Gene-environment interaction between the DRB1 shared epitope and smoking in the risk of anti-citrullinated protein antibody-positive rheumatoid arthritis: all alleles are important. Arthritis Rheum. 2009, 60: 1597-1603.
Michou L, Teixeira VH, Pierlot C, Lasbleiz S, Bardin T, Dieude P, Prum B, Cornelis F, Petit-Teixeira E: Associations between genetic factors, tobacco smoking and autoantibodies in familial and sporadic rheumatoid arthritis. Ann Rheum Dis. 2008, 67: 466-470.
Mikuls TR, Sayles H, Yu F, Levan T, Gould KA, Thiele GM, Conn DL, Jonas BL, Callahan LF, Smith E, Brasington R, Moreland LW, Reynolds RJ, Bridges SL: Associations of cigarette smoking with rheumatoid arthritis in African Americans. Arthritis Rheum. 2010, 62: 3560-3568.
Pedersen M, Jacobsen S, Garred P, Madsen HO, Klarlund M, Svejgaard A, Pedersen BV, Wohlfahrt J, Frisch M: Strong combined gene-environment effects in anti-cyclic citrullinated peptide-positive rheumatoid arthritis: a nationwide case-control study in Denmark. Arthritis Rheum. 2007, 56: 1446-1453.
Klareskog L, Stolt P, Lundberg K, Källberg H, Bengtsson C, Grunewald J, Rönnelid J, Harris HE, Ulfgren AK, Rantapaa-Dahlqvist S, Eklund A, Padyukov L, Alfredsson L: A new model for an etiology of rheumatoid arthritis: smoking may trigger HLA-DR (shared epitope)-restricted immune reactions to autoantigens modified by citrullination. Arthritis Rheum. 2006, 54: 38-46.
Willemze A, van der Woude D, Ghidey W, Levarht EW, Stoeken-Rijsbergen G, Verduyn W, de Vries RR, Houwing-Duistermaat JJ, Huizinga TW, Trouw LA, Toes RE: The interaction between HLA shared epitope alleles and smoking and its contribution to autoimmunity against several citrullinated antigens. Arthritis Rheum. 2011, 63: 1823-1832.
Källberg H, Padyukov L, Plenge RM, Rönnelid J, Gregersen PK, van der Helm-van Mil AH, Toes RE, Huizinga TW, Klareskog L, Alfredsson L: Gene-gene and gene-environment interactions involving HLA-DRB1, PTPN22, and smoking in two subsets of rheumatoid arthritis. Am J Hum Genet. 2007, 80: 867-875.
Mikuls TR, Hughes LB, Westfall AO, Holers VM, Parrish L, van der Heijde D, van Everdingen M, Alarcon GS, Conn DL, Jonas B, Callahan LF, Smith EA, Gilkeson G, Howard G, Moreland LW, Bridges SL: Cigarette smoking, disease severity and autoantibody expression in African Americans with recent-onset rheumatoid arthritis. Ann Rheum Dis. 2008, 67: 1529-1534.
Chun-Lai T, Padyukov L, Dhaliwal JS, Lundström E, Yahya A, Muhamad NA, Klareskog L, Alfredsson L, Larsson PT, Murad S: Shared epitope alleles remain a risk factor for anti-citrullinated proteins antibody (ACPA)-positive rheumatoid arthritis in three Asian ethnic groups. PLoS One. 2011, 6: e21069-
Yahya A, Bengtsson C, Too CL, Larsson PT, Mustafa AN, Abdullah NA, Muhamad NA, Hussein H, Klareskog L, Alfredsson L, Murad S: Smoking is associated with an increased risk of developing ACPA-positive but not ACPA-negative rheumatoid arthritis in Asian populations: evidence from the Malaysian MyEIRA case-control study. Mod Rheumatol. 2011, DOI 10.1007/s10165-011-0544-2
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS, Medsger TA, Mitchell DM, Neustadt DH, Pinals RS, Schaller JG, Sharp JT, Wilder RL, Hunder GG: The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988, 31: 315-324.
Greenland SRK, Lash TL: Measures of effect and measures of association. Modern Epidemiology. Edited by: Rothman KJ, Greenland S, Lash TL. 2008, Philadelphia: Lippincott-Raven, 74-83. 3
Karlson EW, Chang SC, Cui J, Chibnik LB, Fraser PA, De Vivo I, Costenbader KH: Gene-environment interaction between HLA-DRB1 shared epitope and heavy cigarette smoking in predicting incident rheumatoid arthritis. Ann Rheum Dis. 2010, 69: 54-60.
Lee HS, Lee KW, Song GG, Kim HA, Kim SY, Bae SC: Increased susceptibility to rheumatoid arthritis in Koreans heterozygous for HLA-DRB1*0405 and *0901. Arthritis Rheum. 2004, 50: 3468-3475.
Ohmura K, Terao C, Maruya E, Katayama M, Matoba K, Shimada K, Murasawa A, Honjo S, Takasugi K, Tohma S, Matsuo K, Tajima K, Yukawa N, Kawabata D, Nojima T, Fujii T, Yamada R, Saji H, Matsuda F, Mimori T: Anti-citrullinated peptide antibody-negative RA is a genetically distinct subset: a definitive study using only bone-erosive ACPA-negative rheumatoid arthritis. Rheumatology (Oxford). 2010, 49: 2298-2304.
Liu SC, Chang TY, Lee YJ, Chu CC, Lin M, Chen ZX, Liu HF, Dang CW, Chang SC, Lee CS, Cheng TL, Huang CH: Influence of HLA-DRB1 genes and the shared epitope on genetic susceptibility to rheumatoid arthritis in Taiwanese. J Rheumatol. 2007, 34: 674-680.
Källberg H, Ding B, Padyukov L, Bengtsson C, Rönnelid J, Klareskog L, Alfredsson L, EIRA Study Group: Smoking is a major preventable risk factor for rheumatoid arthritis: estimations of risks after various exposure to cigarette smoke. Ann Rheum Dis. 2011, 70: 508-511.
Acknowledgements
The authors thank the Director General of Health, Ministry of Health, Malaysia, for supporting the work described in this article and for permission to publish this article. The authors are also indebted to patients and controls for their kind participation. We gratefully acknowledge Associate Professor Johan Rönnelid for his insightful comments on the manuscript. We also thank Hanjeet Kaur, Yuslina Mat Yusoff, Kee Chee Cheong, Kasthoori Supramaniam, Maizun Mohd Zain, Masita Arip, Fatimah Karmila Abu Bakar, Ahneez Abdul Hameed, Norhazlin Mustafa, Ainur Yusniza Yusoff, Mohd Hazrik Nor Osman, Norziyana Idris, Laily Murat Saffie, Fadzilah Hana Mahpot, Fazilah Hanim Kornain, Mohd Arif Abd Aziz, Nor Hamimah Md Non, and Salwa Hanim Zainal Alam for the collection of data, the MyEIRA study group members: Heselynn Hussein, Nor Shuhaila Shahril, M Eashwary (Putrajaya Hospital, Putrajaya), Wahinuddin Sulaiman (Tengku Bainun Hospital, Ipoh, Perak), Muhaini Othman (Serdang Hospital, Selangor), Azmillah Rosman (Selayang Hospital, Selangor), Suk Chyn Gun (Seremban Hospital, Negeri Sembilan), Mohd Shahrir (Universiti Kebangsaan Malaysia Hospital), Ing Soo Lau (Sultanah Aminah Hospital, Johor) and Ainon Mokhtar (Tengku Ampuan Afzan Hospital, Pahang) for practical help and assistance at the hospitals, and Nor Ashikin Jinah, Irda Yasmoon Awang, Salawati Mansor, Siti Nafisyah Harun and Lee Yin Yin for their technical assistance in the laboratory and at site. This study was financially supported by Ministry of Health, Malaysia: MRG 7/2005, JPP-IMR 07-046, JPP-IMR 08-012, and JPP-IMR 08-006, and by the Swedish Medical Research Council (DNR 348-2009-6468) and Swedish Combine program.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
TCL and AY had full access to all of the data in this study and take responsibility for the integrity of the data and the accuracy of the data analysis. TCL and AY drafted the manuscript and performed statistical analysis and manuscript preparation. TCL, AY, SM, JSD, NAM, NAA, ANM, PTL, LK, LA, LP, and CB conceived the study and participated in the design of the study and manuscript editing. TCL, JSD, and LP performed serologic and molecular genetics assay. NAM and NAA contributed through the assessment of clinical aspects. TCL, AY, LP, and CB take responsibility for the acquisition of data and the analysis and interpretation of data. All authors were involved in drafting or revising the manuscript critically for important intellectual content, and all authors approved the final version to be published.
Chun Lai Too, Abqariyah Yahya contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Too, C.L., Yahya, A., Murad, S. et al. Smoking interacts with HLA-DRB1 shared epitope in the development of anti-citrullinated protein antibody-positive rheumatoid arthritis: results from the Malaysian Epidemiological Investigation of Rheumatoid Arthritis (MyEIRA). Arthritis Res Ther 14, R89 (2012). https://doi.org/10.1186/ar3813
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar3813