Abstract
Utilizing RNA interference as an innovative therapeutic strategy has an immense likelihood to generate novel concepts in precision medicine. Several clinical trials are on the way with some positive initial results. Yet, targeting of RNAi payloads such as small interfering RNAs (siRNAs), microRNA (miR) mimetic or anti-miR (antagomirs) into specific cell types remains a challenge. Major attempts are done for developing nano-sized carriers that could overcome systemic, local and cellular barriers. This progress report will focus on the recent advances in the RNAi world, detailing strategies of systemic passive tissue targeting and active cellular targeting, which is often considered as the holy grail of drug delivery.
Similar content being viewed by others
Review
Introduction
RNA interference (RNAi) is an innate cell machinery for regulation of gene expression. This process is preformed by double-stranded ribonucleic acid (dsRNA) that down-regulates the expression of precise genes with matching nucleotide sequences by decaying specific messenger RNA (mRNA) or by physically obstructing mRNA translation. RNAi can be triggered exogenously by uttering short hairpin RNA (shRNA) with virus-like vectors, or by integrating artificial small interfering RNAs (siRNAs) sequences straight into the cell cytoplasm [1–3].
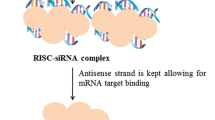
siRNA is a chemically synthesized double stranded RNA (dsRNA) of 19–21 base pairs with 2-nucleotides unpaired in the 5′-phosphorylated ends and unphosphorylated 3′-ends [3–5]. Inside the cell, siRNAs are included into a protein-RNA complex termed rna induced silencing complex (RISC) that segregate the strands of the RNA duplex and junks the passenger strand also known as the sense strand. The antisense strand then guides RISC to anneal and cut the specific mRNA or inhibits its translation [2, 3]. Through reprocessing the target mRNA, the RISC complex includes the anti-sense strand. This process may have a gene knockdown affect that last up to seven days in dividing cells and numerous weeks in non-dividing cells [3, 6]. Moreover, multiple injections of siRNAs can result in steady therapeutic gene silencing [7, 8].
The combination of silencing any preferred gene and the ability to treat various diseases by addressing potential non-druggable targets coupled with an improved safety and the reduced likelihood for meddling to the endogenous microRNA machinery, emphasizes the potential of RNAi to become a new potential modality for precision medicine.
Aside from this potential, employing RNAi molecules as therapeutics is not a marginal assignment. For instance, for siRNAs, the ~ 13.5 kDa and the net negative charge with more than 40 phosphate groups, makes these molecules an obstacle for crossing [9] the plasma membrane and efficiently entering the cell cytoplasm [2, 3, 10]. Intravenous administration of these molecules causes rapid renal clearance and these molecules are susceptible to RNA degradation by RNAses. In addition, naked siRNAs, which are not chemically modified, could be recognized by special receptors of the immune systems that sense nucleic acids termed Toll-Like Receptors (TLRs) [3, 9]. The binding of siRNAs to these receptors may activate the immune system and provoke different responses such as trigger an interferon response, activate the complement system, and induce cytokines. In addition to immune stimulation, these effects can globally inhibit gene expression and generate off-target properties [9–11]. Hence, the need for selective delivery strategies carrying RNAi payloads is essential. This report will focus on the progress of this field, concentrating mainly on systemic applications of siRNA therapeutics. Special highlight will be made on strategies for therapeutic gene silencing in leukocytes in an era of personalized medicine. In precision and personalized medicine, sequencing of the transcriptome of a diseased individual becomes a reality. Thus, the option to design sequence-specific molecules that can interfere with translation of any given protein can be used to manipulate cellular functions and ultimately, might soon become a new therapeutic modality [12, 13].
Cellular siRNA delivery strategies
Common strategies used for delivery of RNAi molecules (siRNA, miRNA mimic or anti-miRNAs) for cellular applications are utilizing conventional transfection techniques. Studies with purely physical methods for example electroporation, gene gun or microinjections [14–17], in addition to studies used calcium phosphate [18], commercial cationic reagents both synthetic and natural [4, 19–24] and cell penetrating peptides (CPPs) [25–29], have been efficiently employed to silence specific genes of interest. Beside for the physical methods, namely electroporation and microinjection, all the other approaches share a common denominator – a cationic charge that enables complexation of the negatively charge RNAi payloads and interact with the negatively charged plasma membrane [30, 31]. In this manner, it is important to note that there are evidences for toxicities of cationic lipids and polymers ([32] and reviewed in [33–35]).
The use of RNAi strategies to silence genes of interest in vitro is an essential tool for studying gene expression in normal and diseased validating new therapeutic targets [36, 37]. Yet, the ability to manipulate gene function in vivo in a disease model combined with the potential to induce therapeutic gene silencing, may open new avenues for exploiting RNAi as a novel therapeutic modality and ultimately may brings closer the era of personalized medicine when transcriptom of patients will be used in order to tailor a specific RNAi drug to their current disease [13, 30].
Although there are large numbers of technologies available for in vitro RNAi delivery shortly represented above, there are still numerous challenges for translating these strategies into clinical practice. The biggest hurdle confronting the translation of siRNAs therapeutic potential into the clinic is the ability to deliver these payloads in a safe- and cell-specific manner [13, 30].
Local and systemic siRNA delivery strategies
Native delivery of siRNAs has been shown in different disease models [6, 28, 30, 38, 39] and a few current clinical trials are utilizing local and topical delivery strategies [2, 9]. Topical and local administration of polymer-free siRNAs or siRNAs that are complexed with lipids or polymers are utilized for local administration. However, this strategy is mainly applicable for subcutaneous tissues, ocular applications and mucosal surfaces.
Systemic delivery of RNAi molecules is currently considered as the ‘Holy Grail’ of the field. Whereas topical and local RNAi delivery strategies have to employ internalization strategies and endosomal release approaches, systemic RNAi delivery strategies need to really on methods to evade the immune system, frame-up within small blood capillaries, uptake by cells of the mononuclear phagocytic system (MPS), degradation by RNAses, renal clearance, anatomical barriers (such as the liver), immune activation, extravasation from blood vessels to target tissues, and permeation within the tissue to name a few [30].
Naked siRNAs can be delivered systemically via hydrodynamic injection. This strategy, with an unknown mechanism, involves rapid intravenous administration of a large volume of siRNAs in physiologic solutions (about 10% of the body weight administered within 5–10 seconds) [30, 40, 41]. Hepatocytes are taken up these siRNAs molecules using this strategy. Several studies were reported to use successfully this strategy, showing efficient gene silencing in the liver [30, 40–43]. Nevertheless, due to volume overload side effects, the hydrodynamic injection approach is not appropriate for therapeutic applications and was only utilized as a proof-of-concept approach [3].
Naked siRNAs can be employed for kidney targeting. Naked siRNAs are known to be eliminated by the glomerulus, which secrete molecules with weights that are below 40 kDa. Free siRNAs are accumulated in the kidney around 30–40 times more than in any other organ [2, 3]. This feature could be utilized for RNAi therapy, but could also introduce novel hurdles in the form of kidney toxicity. Studies performed in rat models of renal injury showed a therapeutic benefit of silencing the proapoptotic gene, p53 that resulted in renal protection, upon single and multiple administrations [3, 44, 45]. QPI-1002 developed by Quark Pharmaceuticals for acute renal injury and delayed graft function is currently under clinical evaluation [3, 45].
Utilizing naked siRNAs for systemic application is appropriate only when the target organ is the kidney. Else, delivery of siRNA payloads for systemic applications must relay on nano-scale delivery platforms. These nano-scale delivery platforms have to be made from materials that are degradable, non-immunogenic and compatible to the biological environment. In addition, the ability to direct these delivery platforms to specific organs and cells will provide them with additional advantage since only diseased cells will be targeted.
The parental siRNA delivery strategies can be generally divided into two categories: passive tissue and active cellular-based deliveries. While, passive tissue delivery strategies use the propensity of macromolecules and nanoparticles to accumulate in organs of the MPS. The MPS, an integral part of the immune system, consists of phagocytic cells located in reticular connective tissue, primarily monocytes and macrophages [30, 34]. Cells of the MPS reside in the spleen, liver (kupffer cells) and different lymph nodes and take up materials and particles supposed to viruses, parasites and bacteria of different types, sizes, geometry, surface curvature and charge [30, 46]. Thus, many efforts are still focusing on generating safe delivery strategies targeting hepatocytes. Active, cellular-based RNAi delivery strategies are based on specific natural ligands or ligand mimic that guide the nano-carriers to organs, tissues and subsets of cells [30, 47].
Systemic passive delivery strategies
Stable nucleic acid-lipid particles (SNALP) (Figure 1) are ~ 90 nm in diameter lipid-based particles forming liposomes with amino lipid content that encapsulates RNAi payloads. These amino lipids have lipid pKa of 6.4-6.8 and thus are positively charged in low pH. RNAi payloads such as siRNAs are suspended in acetate buffer pH 4.0 and mixed with the lipids that are dissolved in ethanol to form stable nucleic acid-lipid particles [48]. In addition, these particles compose of a diffusible lipid that is conjugated to polyethylene glycol (lipid-PEG) [49, 50]. This unique lipid coating stabilizes the particle in the process of particle creation and provides a neutral surface charge and hydrophilic coating that endow these particles with long circulation properties and reduction in the clearance from the bloodstream. This special liposomal features that combining fusogenic and amino lipids allow for internalization of the particles and efficient release of the RNAi payloads that induce gene silencing of the desired gene. A distribution study showed that around 30% of the siRNAs carried by these particles were accumulated in the liver (with minimal accumulation (0.3%) in the lungs. SNALPs encapsulated ApoB -siRNA has shown significant reduction in the mRNA levels of this gene. In spite of the use of amino lipids in the SNALP formulations that are known to trigger different types of toxicities [33], in a non-human primates toxicity study no adverse effects except slight elevation of liver enzyme release was observed. Based on these studies, several human trials are conducted these days to examine the potency of these particles to deliver specific RNAi payloads for reducing cholesterol levels and as novel therapeutics in liver cancer [2, 45]. This strategy was also used to deliver siRNAs against the polymerase gene of the Zaire strain of Ebola virus and shown to protect guinea pigs from lethal challenge this virus [51]. Different formulations that used different amino lipids have shown to knockdown effectively genes of interest, but also triggered immune, liver and kidneys toxicities and thus could not be used for human testing.
RNAi delivery systems in development stages include RNAi coupled to cell penetrating molecules such as cholesterol (A); or other low molecular weight molecules (B); conjugated to an aptamer that target a specific cell surface receptor (C); conjugated to cell membrane-penetrating polymer that is linked to targeting small molecules (D), complexed with fusion proteins composed of targeting peptide or a fragment of an antibody coupled to an RNA binding domain that is either protamine (E); or poly-arginine (F); or entrapped within nanoparticles (G); or LNPs (H); bearing targeting moieties. Reprinted with permission from ref. 31 Copyright 2011 Gene Therapy.
Different types of adverse effects have been documented with the use of different amino lipid-based nanoparticles [34, 35, 52, 53] thus, there are some activities to form lipid-based nanoparticles with neutral charge for systemic delivery of RNAi payloads. One example is the use of 1,2-dioleoyl-sn-glycero-3-phosphatidylcholine (DOPC) which do not have PEG on their surface and entrap RNAi payloads targeted against various mRNA in ovarian cancers and melanoma [54, 55]. These lipid-based particles were shown to accumulate in cancerous tissues possibly due to the Enhanced Permeability and Retention (EPR) effect. This phenomena is based on increased fenestrations of the blood vessels in tumors caused by rapid and defective angiogenesis, and dysfunctional lymphatic drainage that retains the accumulated particles [56], see Figure 2[3].
A graphic representation of the potential mechanisms, by which nanoparticles can deliver RNAi to tumors. Multi-functional lipid-based nanoparticles (NPs) co-encapsulated with chemotherapeutic drug (orange dots) and RNAi payloads are shown as illustrative nanoparticles. Passive tissue targeting is achieved by extravasation of nanoparticles through increased permeability of the tumor vasculature and ineffective lymphatic drainage (EPR effect). Active cellular targeting (inset) can be achieved by decorating the surface of nanoparticles with multiple targeting moieties that promote cell-specific recognition and binding. The nanoparticles can reach different tumor subpopulation concomitantly to ensure maximal therapeutic effect and release their contents in close proximity to the target cells, attach to the membrane of the cell and act as an extracellular sustained-release drug depot or internalize into the cell introducing their payload to cell cytoplasm. Red labeled cells – infiltrating macrophages that are acting as ‘nurse-like’ cells aiding the tumor by supplying survival cues to the tumor cells and nutrients for tumor growth.
Lipidoid (synthetic lipid-like molecules)-containing liposomes are additional siRNA delivery strategy that has been shown to induce effective genes silencing ( < 80% reduction in ApoB and Factor VII mice’s mRNAs levels) in the liver [3]. Single intravenous administration of lipidoid-containing lipid-based nanoparticles (LNPs) encapsulate ApoB-siRNA resulted in 50% decrease in the protein level 3 days and lasted up to 2 weeks after the treatment. Although no major immune toxicity was observed, increases in the levels of liver enzymes suggested a potential liver toxicity [3, 57, 58] (Figure 1).
Histidine-Lysine (HK) peptides are an additional, simple and effective RNAi delivery strategy. While lysine is important for binding the RNAi payloads, histidines stabilizes these particles and have an important role in buffering acidic endosomes, thereby enabling endosomal disruption and payload release [30]. HK peptides carrying Raf-1-siRNA or human rhomboid family-1- siRNAs induced significant silencing of target genes and suppress the progression of tumor-bearing mice in a human xenografts models [30, 59, 60].
Atelocollagen (AC) consists of a no- to minimal fraction of pepsin-digested collagen type I from calf dermis. AC is rich in positively charged amino acids such as lysine and hydroxylysine. It condenses the negatively charged RNAi payload and interacts with the plasma membrane, hence helps to incorporate the RNAi into the cells’ cytoplasm [30]. Indeed these biomaterials have not been modified to target specifically cancerous tissues, however, it have been shown that due to the EPR effect an accumulation of AC within tumor vicinity is documented in several tumor xenografts mouse models [27, 30, 61–63].
Systemic active cellular delivery strategies
siRNAs conjugated to different molecules that can aid in cellular targeting is a common strategy for active cellular delivery. One such example is the Cholesterol – siRNA conjugate [3, 30]. This delivery strategy is based on the lipoprotein to which the cholesterol-siRNAs conjugates are attached in the circulation. When the conjugates bind low density lipoprotein (LDL), the particles are mainly taken up by the liver due to the wide expression of LDL-receptors whereas when they bind to high density lipoprotein (HDL), these conjugates accumulate in the gut, the kidney, the liver and steroidogenic organs, all of which express scavenger receptor class B, type I (SR-BI) receptors, which bind HDL [3, 64]. Cholesterol-ApoB-siRNA conjugate as well as α-tocopherol [65] and lithocholic acid or lauric acid conjugated to ApoB-siRNA [66] reduced serum cholesterol and ApoB mRNA levels in the liver [3, 9].
An additional strategy in this category is the dynamic polyconjugates (DP) [3, 67]. This strategy includes membrane-active polymers that when reaching the acidic environment of the endosomes release the RNAi payloads. Using N-acetylgalactosamine, which binds to the asialoglycoprotein receptor, the DP targets preferentially hepatocytes. Like the other strategies that target the liver (e.g. SNALP), these particles have shown to effectively decreased ApoB mRNA levels in the liver when ApoB-siRNAs were used as the RNAi payloads [3].
Polyethyleneimine (PEI) complexes carrying RNAi payloads have also shown to trigger in vivo gene silencing when administrated subcutaneously into human tumors implented in nude mice. These PEI complexes composed of RGD (Arg-Gly-Asp) tripeptide that endow them specificty to integrins (adhesion receptors highly expressed on tumor cells and extracellular materix around the tumor) and coupled via PEG (aimed at longer circulation half-life, and reduced immunogenicity) to PEI (a cationic polymer that in addition to its ability to condense nucleic acids, its pH-buffering property disrupts endosomes, thus enabling to reach the cytoplasm) [3]. When RGD-PEG-PEI are complexed with RNAi payloads, they form a polyplex that target tumor vasculature and some cancerous tissues expressing integrins (αvβ3 and αvβ5) [68].
cyclodextrin-containing polycation (CDP) particles have been successfully used for siRNAs delivery into mice’s subcutaneous tumors [69] and have shown promise in clinical trials [70]. CDP is a polymer with a cyclic glucose backbone that when complexed with nucliec acids assembles into a colloidal 50–70 nm in diameter particle. To attain targeting capabilities, transferin (Tf)-coupled PEG is attached to the surface of the particles exploiting the upregulation of Tf receptors in many types of tumors. CDP is considered non-toxic compared with conventional cationic polymers. Safety experiments performed with non-human primates revealed that in the highest concentration tested, administration of CDP-based particles induced increase in blood urea (could be a sign of kidney toxicity), slight elevation of liver enzyme levels in the serum and a mild increase in IL-6 levels [3, 71, 72]. In addition, repeating intravenous administration of the CDP-based particles provoked the formation of antibodies to human-Tf. Despite those disadvantages, the efficacy of Tf-coupled CDP containing siRNAs for ovarian cancer treatment is evaluated nowadays in a clinical trial [3, 70, 71].
An innovative platform strategy based on a fusion protein carrier having a specific ligand (mAb fragment) fused to human trucated protamine (RNA condenser) was developed to deliver RNAi payloads in a receptor-specific manner [73] (Figure 1). Protamines are 5–8 kDa proteins and highly basic composed of 55-79% arginine residues [74]. Positively charged, protamine interacts with the negatively charged RNAi payload, hence stabilizes, neutralizes and condenses the RNAi payloads. As a proof-of-concept, anti-Her 2 (ErbB2)-human truncated protamine fusion protein in complex with siRNA significantly suppresses the growth of breast cancer cells [3, 73].
Aptamer-siRNA chimeras (Figure 1) are RNA-based nanostructures for specific delivery of siRNAs. This strategy is based on the ability of organized RNAs to bind proteins with high specificity and affinity. The chimera comprise of a targeting entity, the aptamer, and an siRNA component. These chimeras have shown to bind and deliver specifically siRNAs into human xenograft prostate cancer model. The aptamer itself bind to PSMA, a cell-surface receptor overexpressed in many types of prostate cancer cells and tumor vascular endothelium, whereas the siRNAs decrease the expression of survival genes [3, 75]. This strategy reduced adverse effects therefore these chimeras have low immunogenicity. In addition, these chimeras can be easily scaled up at a relatively low cost and posses smaller dimensions compared with that of monoclonal antibodies (<15 kDa versus 150 kDa), which should endorses improve tissue penetration [3, 30].
Various approaches of targeted amino-based LNPs serve for targeting of stellate cells in the liver. These cells are involved in the formation of scar tissue in response to liver damage such as fibrosis or as nurse-like cells in the case of a liver cancer (hepatoma) [30]. These specilized macrophages express unique receptors for retinol binding protein which uptake vitamin A. Using this approach, intravenous administration of amino-LNPs coupled to vitamin A and complexed with siRNA to a murine key fibrogenesis factor (gp46) into cirrhotic mice, knockdown specific gene in mice’ liver and resolved fibrosis [30, 76]. 1,2-dioleoyl-3-trimethylammonium-propane (DOTAP) bearing LNPs encapsulating HER2-siRNAs and containing HK peptides (to enhance the escape from the endosomes) coupled to a single-chain antibody fragment (scFv) that binds to transferrin receptors (elevated on the surface of many cancerous cells), have been targeted to tumor xenograft and inhibited tumor progression [30, 77]. Anisamid-PEG-Liposomes-polycation-DNA (anisamid-PEG-LPDs) are unilamellar amino-LNPs coated with PEG-linked anisamide (a small-molecule compound that binds sigma receptors) on their surface, and protamine-condensed mixture of siRNAs and a carrier calf thymus DNA in their core. Encapsulating EGFR-siRNA, anismaide-PEG-LPDs administrated systemically into mice bearing tumors, have been shown to increase mice’s sensitivity to chemotherapy [30, 78]. These interesting LNPs triggered the realase of cytokines in robust manner which could hamper their immediate translation into clinical practice. Yet, induction of cytokine response is not always poisonous and there are substential cases when triggering an immune response (mostly pro-inflammatory response) could augment the therapeutic response.
Manipulating leukocytes with RNAi via targeted strategies
Manipulating gene profiling in leukocytes holds great promise for drug discovery and for enhancing the development of new therapeutic modalities for leukocytes implicated diseases such as inflammation, hematological malignancies, and leukocytes-tropic viral infections. Yet, systemic delivery of RNAi to leukocytes has proven to be extremely challenging since leukocytes are intrinsically resistance to conventional transfection mechanisms and since they are dispersed in the body and thus need specific cell surface markers to be used as targeting moieties [30, 47].
siRNAs that are linked (by chemical synthesis) to a CpG oligonucleotide agonist of Toll Like Receptor (TLR)9 for targeting myeloid cells and B cells (both are key components of tumor microenvironment) that express this receptor were reported by Kortylewski et al. [79]. These conjugates knockdown the expression of the gene stat3 by using the RNAi payload and simultaneously activated TLRs responses using its agonist. Consequently, the tumor microenvironment was changed from pro-oncogenic environment to an anti-oncogenic (by causing activation of tumor-associated immune cells and potent antitumor immune responses) [30].
An interesting strategy simillar to the protamine fusion protein startegy was developed to treat viral-tropic infections. scFv against CD7, a surface antigen present on the majority of human T cells was modified to include a Cys residue for conjugation to a 9 arginine (R) residue. The concept was that the scFv will target a specific cell surface receptor while the 9R will aid in complexing the RNAi payload. This elegant strategy was utilized for specific delivery of CCR5 (a chemokine receptor that function as co-receptor for HIV) and Vif/Tat (HIV replication proteins) -siRNAs payloads into T cells, and had shown to suppress HIV infection in humanized mice without inducing toxicity in target cells [3, 80, 81]. The same strategy was used for trying to treat dengue virus infected cells. This study utilized DC3, a 12-mer peptide that targets dendritic cells coupled to 9R. TNF-α siRNAs was used to decrease the mRNA levels. In dengue pathogenesis TNF-α plays a pivotal role and is highly conserved sequence in the viral envelope. These complexes significantly reduced virus-induced production of TNF-α and succeeded to suppress the viral replication in monocytes derived dendritic cells and macrophages in vitro. In vivo, treatment of mice with intravenous injection of DC3-9dR-complexes carried TNF-α–siRNAs, effectively suppressed this cytokine production by dendritic cells [3, 82].
The strategy we developed for targeting subsets of leukocytes is based on leukocytes’ integrins, which are the most characterized cell adhesion molecules that mediate cell-cell and cell-matrix interactions [3, 83]. Utilizing the lymphocyte function associated antigen-1 (LFA-1) integrin, which is expressed in all leukocytes’ subtypes, we developed scFv-protamine fusion proteins for selective targeting. The use of LFA-1 for targeting leukocytes is supported by its exclusive expression on leukocytes, its constitutive internalization and recycling activity and its ability to undergo activation-dependent conformational changes. Using those antibody-protamine fusion proteins we have shown specific delivery of RNAi payloads into leukocytes in vitro and in vivo. Prominently, lymphocytes activation or interferon response was not observed making this strategy a safe option for therapeutic intervention. In addition, a high-affinity conformation reagent that target LFA-1 only in activated lymphocytes was prepared and characterized [84, 85]. We showed a superior selectivity towards activated lymphocytes, which could provide a way to overcome the undesirable immune activation on bystander immune cells. Additionally, due to the prevalent of aberrant affinity modulation of integrins in a variety of leukocyte-implication diseases [86, 87], targeting the high-affinity conformation of LFA-1 is expected to be very effective therapeutic strategy [3, 47, 85].
To substantially enlarge the amount of the RNAi payload and attain a superior and more selective gene silencing, we have formed LNPs decorated with anti-integrin mAb termed ‘Integrin-targeted stabilized nanoparticles (I-tsNP)’ that successfully delivered RNAi payloads into subsets of leukocytes involved in gut inflammation [88]. These particles are made from neutral liposomes to form multilamellar vesicles (MLV) are extruded to ~80 nm in diameter unilamellar vesicles (ULV) are covalently coated with hyaluronan (HA), a naturally-occuring glycosaminoglycan, for stabilization of the particles during RNAi encapsulation. HA also prolong the in vivo half-life in the circulation. Targeting capabilities is formed by coupling a mAb against the β7 integrin (which is highly expressed in gut leukocytes) to the HA [89]. Utilizing this strategy, we found a new, unknown role for cyclin D1 as a potential anti-inflammatory therapeutic target controlling some of the pro-inflammatory cytokines. These leukocytes-targeted- LNPs offer one of the safest platforms for nucleic acids delivery, preventing cytokine induction, interferon response and complement activation as well as liver and kidneys toxicities. This strategy was also utilized for delivery of CCR5 -siRNAs to human lymphocytes and monocytes with an anti-LFA-1 mAb. LFA-1 I-tsNPs entrapping CCR5-siRNAs protected mice from HIV challenge [90] and did not induce secretion of TNF-α (one of the major players in inflammation) nor did it trigger interferon response, hence reinforces the vast potential for clinical translation. Since this strategy is a platform, it is very likely that by exchanging the mAb on the surface, for example, against B cell malignancies (anti-CD19 or CD20) it will be possible to target many types of B-cells malignancies such as mantle cell lymphoma (MCL), and chronic lymphocytic leukemia (CLL) in a specific and efficient manner. In addition, by using activated –dependent conformational reagent such as AL-57 [85] – it will be possible to target activated cells such as multiple myeloma cells (MM) while leaving naïve B cells untouched.
Clinical translation of siRNA nanomedicines
Several RNAi-based clinical trials utilize naked RNAi molecules with local delivery (Table 1), yet, a great promise for the entire RNAi field is based on systemic administration and vast progress has been made using non-human primate models [49, 91–95].
The first sets of clinical evaluations introduced naked siRNAs to patients suffering from age-related macular degeneration (AMD) and diabetic macular edema (DME). The administration of these siRNAs was done intraviteral and the siRNAs were against vascular endothelial growth factor (VEGF). Other local strategies to deliver RNAi payloads were conducted, but many of these strategies were ended because of safety issues [96, 97]. Since then, tremendous efforts were done to refine and advance these local strategies and adjust them for systemic administration (Table 1) [9].
The first-in-human systemic administration trial engaging the use of targeted NPs for RNAi payloads to solid tumors – named CALAA-01, was conducted in 2008 [70, 71]. CALAA-01 product is based on the Tf-CDP NPs previously described in mice and non-human primates [69, 94], which form a 70 nm in diameter particle, formulating the an anti- ribonucleotide reductase subunit 2 (RRM2) siRNAs [71]. Biopsies taken from melanoma patients that were given intravenous injections of Tf-CDP-NPs showed intracellular accumulation of the Tf-CDP in the cancerous tissues and not in neighboring tissues in a dose-dependent manner. Moreover, reduction in both RRM2 mRNA and RRM2 protein levels after several cycles of dosing was demonstrated providing promise and hope to the field of systemic RNAi delivery strategies [70].
Meanwhile several other systemic delivery strategies entered the clinical trials, six are based on SNALP strategy [9, 48]. A remarkable achievement was done in 2008, when SNALP-based systems formulated two different RNAi payloads against VEGF and kinesin spindle protein (KSP) in a single vehicle and systemically given to patients with liver cancer and transthyretin (TTR)-mediated amyloidosis (ATTR) [48]. This therapy was well tolerated and induced anti-tumor effects in most patients. In 2009, three novel drugs entered clinical evaluation, two of which, ALN-TTR01 and TKM-ApoB were SNALP-based delivery systems targeting hepatocytes and formulated with anti- Transthyretin (TTR) and anti-ApoB siRNAs in ATTR and hypercholesterolemia patients, respectively [9]. A single administration of ALN-TTR01 resulted in a significant reduction in amyloid deposits in the desired tissues as well as in the serum level of the TTR protein in a dose-dependent manner [9]. TKM-ApoB trial was terminated possibly since only some patients responded. In addition, several patients experienced flu-like syndrome usually known as a cytokine storm at the highest dose administrated. A year later, a novel formulation based on the SNALP system and targeting polo-like kinase 1 (PLK1) was evaluated in patients with advanced solid tumors and lymphoma that were unaffected by other conservative treatments. This therapeutic strategy is aimed to suppress cell-cycle progression and induce apoptosis in the cancerous tissue.
Another intriguing therapeutic strategy, which was clinically tested in patients with advanced colon cancer, targets Protein Kinase N3 (PKN3), an important mediator of the PI3K pathway. To deliver PKM3-siRNAs, Atu027 lipoplexes were used. Atu027 was reported to activate the complement system in clinical trials, and thus needs to be further optimized for future clinical testing. A novel strategy targeted against Ebola virus (TKM-EBOLA) and a strategy to reduce hypercholestrolemia (ALN-PCS02), both SNALP-based formulations entered clinical evaluation in 2011 (Table 1) [9, 97].
Conclusion
The promise of RNAi to manipulate the function of virtually any gene in the human genome open new avenues to personalized the treatment of many types of diseases. This potential coupled with the development of selective and safe nano-scale delivery strategies generated the basis for targeted therapy in many types of illnesses such as cancer (solid and blood), inflammation, and viral infections. Yet, the lack of in deep understanding of molecular pathways in health and diseases together with general toxicities related to engineered nanomedicines can hamper the full potential for precision RNAi-based medicine and restrain the development of clinically approved novel RNAi modalities.
Although the great progress achieved towards personalizing disease care, the current personalized therapies targets a single specific molecular marker on tumor cells and thus neglecting the vast heterogeneity presents within the primary tumor, between different metastases, within each metastasis and between tumors of different patients. Consequently, current treatment usually results in apparent partial or complete responses, which in most cases follow by a resistant tumor relapse and mortality of the patients. Therefore, personalized treatment requires multi-layer characterization of the molecular signatures of tumor cell subpopulations together with individualized pharmacotyping (identify specific sequence alternations in potential therapeutic targets, enzymes that metabolized drugs as well as drug transporters that may alter the efficacy, specificity and sides effects) to achieve maximal efficacy.
We envision that the growing efforts for fine-tuning NPs design, optimizing intracellular payload release, successful approaches in minimizing adverse effects, and functionalizing the NPs with selective targeting moieties, along with the comprehensive understanding of our genome and transcriptome, would collectively tile the way for specific, safe and targeted NPs that carry RNAi payloads for precision medicine.
References
Sledz CA, Williams BR: RNA interference in biology and disease. Blood. 2005, 106 (3): 787-794. 10.1182/blood-2004-12-4643. PubMed PMID: 15827131. Pubmed Central PMCID: 1895153. Epub 2005/04/14. eng
de Fougerolles A, Vornlocher HP, Maraganore J, Lieberman J: Interfering with disease: a progress report on siRNA-based therapeutics. Nat Rev Drug Discov. 2007, 6 (6): 443-453. 10.1038/nrd2310. PubMed PMID: 17541417. Epub 2007/06/02. eng
Peer D: Induction of therapeutic gene silencing in leukocyte-implicated diseases by targeted and stabilized nanoparticles: a mini-review. J Control Release. 2010, 148 (1): 63-68. 10.1016/j.jconrel.2010.06.029. PubMed PMID: 20624432. Epub 2010/07/14. eng
Elbashir SM, Harborth J, Lendeckel W, Yalcin A, Weber K, Tuschl T: Duplexes of 21-nucleotide RNAs mediate RNA interference in cultured mammalian cells. Nature. 2001, 411 (6836): 494-498. 10.1038/35078107. PubMed PMID: 11373684. Epub 2001/05/25. eng
Amarzguioui M, Rossi JJ, Kim D: Approaches for chemically synthesized siRNA and vector-mediated RNAi. FEBS Lett. 2005, 579 (26): 5974-5981. 10.1016/j.febslet.2005.08.070. PubMed PMID: 16199038. Epub 2005/10/04. eng
Palliser D, Chowdhury D, Wang QY, Lee SJ, Bronson RT, Knipe DM: An siRNA-based microbicide protects mice from lethal herpes simplex virus 2 infection. Nature. 2006, 439 (7072): 89-94. 10.1038/nature04263. PubMed PMID: 16306938
Bartlett DW, Davis ME: Insights into the kinetics of siRNA-mediated gene silencing from live-cell and live-animal bioluminescent imaging. Nucleic Acids Res. 2006, 34 (1): 322-333. 10.1093/nar/gkj439. PubMed PMID: 16410612. Pubmed Central PMCID: 1331994. Epub 2006/01/18. eng
Manjunath N, Dykxhoorn DM: Advances in synthetic siRNA delivery. Discov Med. 2010, 9 (48): 418-430. PubMed PMID: 20515610. Epub 2010/06/03. eng
Daka A, Peer D: RNAi-based nanomedicines for targeted personalized therapy. Adv Drug Deliv Rev. 2012, 64 (13): 1508-1521. 10.1016/j.addr.2012.08.014. PubMed PMID: 22975009
Robbins M, Judge A, Ambegia E, Choi C, Yaworski E, Palmer L: Misinterpreting the therapeutic effects of small interfering RNA caused by immune stimulation. Hum Gene Ther. 2008, 19 (10): 991-999. 10.1089/hum.2008.131. PubMed PMID: 18713023. Epub 2008/08/21. eng
Kleinman ME, Yamada K, Takeda A, Chandrasekaran V, Nozaki M, Baffi JZ: Sequence- and target-independent angiogenesis suppression by siRNA via TLR3. Nature. 2008, 452 (7187): 591-597. 10.1038/nature06765. PubMed PMID: 18368052. Pubmed Central PMCID: 2642938. Epub 2008/03/28. eng
Moghimi SM, Peer D, Langer R: Reshaping the future of nanopharmaceuticals: ad iudicium. ACS Nano. 2011, 5 (11): 8454-8458. 10.1021/nn2038252. PubMed PMID: 21992178. Epub 2011/10/14. eng
Rosenblum D, Peer D: Omics-based nanomedicine: the future of personalized oncology. Cancer Lett. 2013, PubMed PMID: 23941830
Ma M, Zhou L, Guo X, Lv Z, Yu Y, Ding C: Decreased cofilin1 expression is important for compaction during early mouse embryo development. Biochim Biophys Acta. 2009, 1793 (12): 1804-1810. 10.1016/j.bbamcr.2009.09.009. PubMed PMID: 19751773. eng
Bose S, Leclerc GM, Vasquez-Martinez R, Boockfor FR: Administration of connexin43 siRNA abolishes secretory pulse synchronization in GnRH clonal cell populations. Mol Cell Endocrinol. 2010, 314 (1): 75-83. 10.1016/j.mce.2009.08.016. PubMed PMID: 19716855. Pubmed Central PMCID: 2783823. Epub 2009/09/01. eng
Wiese M, Castiglione K, Hensel M, Schleicher U, Bogdan C, Jantsch J: Small interfering RNA (siRNA) delivery into murine bone marrow-derived macrophages cells by electroporation. J Immunol Methods. 2010, 353 (1-2): 102-10. 10.1016/j.jim.2009.12.002. PubMed PMID: 20006615. Epub 2009/12/17. Eng
Honjo K, Takahashi KA, Mazda O, Kishida T, Shinya M, Tokunaga D: MDR1a/1b gene silencing enhances drug sensitivity in rat fibroblast-like synoviocytes. J Gene Med. 2010, 12 (2): 219-27. PubMed PMID: 19950109. Epub 2009/12/02. Eng
Donze O, Picard D: RNA interference in mammalian cells using siRNAs synthesized with T7 RNA polymerase. Nucleic Acids Res. 2002, 30 (10): e46-10.1093/nar/30.10.e46. PubMed PMID: 12000851. eng
Tsubouchi A, Sakakura J, Yagi R, Mazaki Y, Schaefer E, Yano H: Localized suppression of RhoA activity by Tyr31/118-phosphorylated paxillin in cell adhesion and migration. The J of cell Biol. 2002, 159 (4): 673-683. 10.1083/jcb.200202117. PubMed PMID: 12446743. eng
Huang YZ, Zang M, Xiong WC, Luo Z, Mei L: Erbin suppresses the MAP kinase pathway. J Biol Chem. 2003, 278 (2): 1108-1114. 10.1074/jbc.M205413200. PubMed PMID: 12379659. eng
Zhang M, Bai CX, Zhang X, Chen J, Mao L, Gao L: Downregulation enhanced green fluorescence protein gene expression by RNA interference in mammalian cells. RNA Biol. 2004, 1 (1): 74-77. PubMed PMID: 17194936. eng
Gosain AK, Machol JA, Gliniak C, Halligan NL: TGF-beta1 RNA interference in mouse primary dura cell culture: downstream effects on TGF receptors, FGF-2, and FGF-R1 mRNA levels. Plast Reconstr Surg. 2009, 124 (5): 1466-1473. 10.1097/PRS.0b013e3181b98947. PubMed PMID: 20009832. eng
Cheng SQ, Wang WL, Yan W, Li QL, Wang L, Wang WY: Knockdown of survivin gene expression by RNAi induces apoptosis in human hepatocellular carcinoma cell line SMMC-7721. World J Gastroenterol. 2005, 11 (5): 756-759. PubMed PMID: 15655839. eng
Baker BE, Kestler DP, Ichiki AT: Effects of siRNAs in combination with Gleevec on K-562 cell proliferation and Bcr-Abl expression. J Biomed Sci. 2006, 13 (4): 499-507. 10.1007/s11373-006-9080-z. PubMed PMID: 16547768. eng
Crombez L, Charnet A, Morris MC, Aldrian-Herrada G, Heitz F, Divita G: A non-covalent peptide-based strategy for siRNA delivery. Biochem Soc Trans. 2007, 35 (1): 44-46. 10.1042/BST0350044. PubMed PMID: 17233597. eng
Muratovska A, Eccles MR: Conjugate for efficient delivery of short interfering RNA (siRNA) into mammalian cells. FEBS Lett. 2004, 558 (1–3): 63-68. PubMed PMID: 14759517. eng
Minakuchi Y, Takeshita F, Kosaka N, Sasaki H, Yamamoto Y, Kouno M: Atelocollagen-mediated synthetic small interfering RNA delivery for effective gene silencing in vitro and in vivo. Nucleic Acids Res. 2004, 32 (13): e109-10.1093/nar/gnh093. PubMed PMID: 15272050. eng
Takei Y, Kadomatsu K, Yuzawa Y, Matsuo S, Muramatsu T: A small interfering RNA targeting vascular endothelial growth factor as cancer therapeutics. Cancer Res. 2004, 64 (10): 3365-3370. 10.1158/0008-5472.CAN-03-2682. PubMed PMID: 15150085. eng
Puebla I, Esseghir S, Mortlock A, Brown A, Crisanti A, Low W: A recombinant H1 histone-based system for efficient delivery of nucleic acids. J Biotechnol. 2003, 105 (3): 215-226. 10.1016/j.jbiotec.2003.07.006. PubMed PMID: 14580793. eng
Weinstein S, Peer D: RNAi nanomedicines: challenges and opportunities within the immune system. Nanotechnology. 2010, 21 (23): 1-13. PubMed PMID: ISI:000277746900002. English
Peer D, Lieberman J: Special delivery: targeted therapy with small RNAs. Gene Ther. 2011, 18 (12): 1127-1133. 10.1038/gt.2011.56. PubMed PMID: 21490679. Epub 2011/04/15. eng
Kedmi R, Ben-Arie N, Peer D: The systemic toxicity of positively charged lipid nanoparticles and the role of Toll-like receptor 4 in immune activation. Biomaterials. 2010, 31 (26): 6867-6875. 10.1016/j.biomaterials.2010.05.027. PubMed PMID: 20541799. Epub 2010/06/15. eng
Lv H, Zhang S, Wang B, Cui S, Yan J: Toxicity of cationic lipids and cationic polymers in gene delivery. J Control Release. 2006, 114 (1): 100-109. 10.1016/j.jconrel.2006.04.014. PubMed PMID: 16831482. eng
Peer D: Immunotoxicity derived from manipulating leukocytes with lipid-based nanoparticles. Adv Drug Deliv Rev. 2012, 64 (15): 1738-1748. 10.1016/j.addr.2012.06.013. PubMed PMID: 22820531
Vorup-Jensen T, Peer D: Nanotoxicity and the importance of being earnest. Adv Drug Deliv Rev. 2012, 64 (15): 1661-1662. 10.1016/j.addr.2012.09.002. PubMed PMID: 23000008
Weinstein S, Emmanuel R, Jacobi AM, Abraham A, Behlke MA, Sprague AG: RNA inhibition highlights cyclin D1 as a potential therapeutic target for mantle cell lymphoma. PLoS One. 2012, 7 (8): e43343-10.1371/journal.pone.0043343. PubMed PMID: 22905260. Pubmed Central PMCID: 3419170
Emmanuel R, Weinstein S, Landesman-Milo D, Peer D: eIF3c: a potential therapeutic target for cancer. Cancer Lett. 2013, 336 (1): 158-166. 10.1016/j.canlet.2013.04.026. PubMed PMID: 23623922
Bitko V, Musiyenko A, Shulyayeva O, Barik S: Inhibition of respiratory viruses by nasally administered siRNA. Nat Med. 2005, 11 (1): 50-55. 10.1038/nm1164. PubMed PMID: 15619632. Epub 2004/12/28. eng
Kim B, Tang Q, Biswas PS, Xu J, Schiffelers RM, Xie FY: Inhibition of ocular angiogenesis by siRNA targeting vascular endothelial growth factor pathway genes: therapeutic strategy for herpetic stromal keratitis. Am J Pathol. 2004, 165 (6): 2177-2185. 10.1016/S0002-9440(10)63267-1. PubMed PMID: 15579459. eng
Zender L, Kubicka S: Suppression of apoptosis in the liver by systemic and local delivery of small-interfering RNAs. Methods Mol Biol. 2007, 361: 217-226. PubMed PMID: 17172714. Epub 2006/12/19. eng
De Souza AT, Dai X, Spencer AG, Reppen T, Menzie A, Roesch PL: Transcriptional and phenotypic comparisons of Ppara knockout and siRNA knockdown mice. Nucleic Acids Res. 2006, 34 (16): 4486-4494. 10.1093/nar/gkl609. PubMed PMID: 16945951. Pubmed Central PMCID: 1636368. Epub 2006/09/02. eng
Saito Y, Kon S, Fujiwara Y, Nakayama Y, Kurotaki D, Fukuda N: Osteopontin small interfering RNA protects mice from fulminant hepatitis. Hum Gene Ther. 2007, 18 (12): 1205-1214. 10.1089/hum.2007.069. PubMed PMID: 17988193. Epub 2007/11/09. eng
Lewis DL, Wolff JA: Systemic siRNA delivery via hydrodynamic intravascular injection. Adv Drug Deliv Rev. 2007, 59 (2–3): 115-123. PubMed PMID: 17442446. Epub 2007/04/20. eng
Molitoris BA, Dagher PC, Sandoval RM, Campos SB, Ashush H, Fridman E: siRNA targeted to p53 attenuates ischemic and cisplatin-induced acute kidney injury. J Am Soc Nephrol. 2009, 20 (8): 1754-1764. 10.1681/ASN.2008111204. PubMed PMID: 19470675. Pubmed Central PMCID: 2723992. Epub 2009/05/28. eng
Drug E, Landesman-Milo D, Belgorodsky B, Ermakov N, Frenkel-Pinter M, Fadeev L: Enhanced bioavailability of polyaromatic hydrocarbons in the form of mucin complexes. Chem Res Toxicol. 2011, 24 (3): 314-320. 10.1021/tx100426s. PubMed PMID: 21332130. Epub 2011/02/22. eng
Howard KA, Peer D: Providing the full picture: a mandate for standardizing nanoparticle-based drug delivery. Nanomedicine (Lond). 2013, 8 (7): 1031-1033. 10.2217/nnm.13.95. PubMed PMID: 23837825
Peer D: A daunting task: manipulating leukocyte function with RNAi. Immunol Rev. 2013, 253 (1): 185-197. 10.1111/imr.12044. PubMed PMID: 23550647
Tam YY, Chen S, Cullis PR: Advances in Lipid Nanoparticles for siRNA Delivery. Pharmaceutics. 2013, 5 (3): 498-507. 10.3390/pharmaceutics5030498. PubMed PMID: 24300520. Pubmed Central PMCID: 3836621
Zimmermann TS, Lee AC, Akinc A, Bramlage B, Bumcrot D, Fedoruk MN: RNAi-mediated gene silencing in non-human primates. Nature. 2006, 441 (7089): 111-114. 10.1038/nature04688. PubMed PMID: 16565705. Epub 2006/03/28. eng
Morrissey DV, Lockridge JA, Shaw L, Blanchard K, Jensen K, Breen W: Potent and persistent in vivo anti-HBV activity of chemically modified siRNAs. Nat Biotechnol. 2005, 23 (8): 1002-1007. 10.1038/nbt1122. PubMed PMID: 16041363. Epub 2005/07/26. eng
Geisbert TW, Hensley LE, Kagan E, Yu EZ, Geisbert JB, Daddario-DiCaprio K: Postexposure protection of guinea pigs against a lethal ebola virus challenge is conferred by RNA interference. J Infect Dis. 2006, 193 (12): 1650-1657. 10.1086/504267. PubMed PMID: 16703508. Epub 2006/05/17. eng
Solmesky LJ, Shuman M, Goldsmith M, Weil M, Peer D: Assessing cellular toxicities in fibroblasts upon exposure to lipid-based nanoparticles: a high content analysis approach. Nanotechnology. 2011, 22 (49): 494016-10.1088/0957-4484/22/49/494016. PubMed PMID: 22101838. Epub 2011/11/22. Eng
Goldsmith M, Mizrahy S, Peer D: Grand challenges in modulating the immune response with RNAi nanomedicines. Nanomedicine (Lond). 2011, 6 (10): 1771-1785. 10.2217/nnm.11.162. PubMed PMID: 22122585. Epub 2011/11/30. eng
Villares GJ, Zigler M, Wang H, Melnikova VO, Wu H, Friedman R: Targeting melanoma growth and metastasis with systemic delivery of liposome-incorporated protease-activated receptor-1 small interfering RNA. Cancer Res. 2008, 68 (21): 9078-9086. 10.1158/0008-5472.CAN-08-2397. PubMed PMID: 18974154. Pubmed Central PMCID: 2597081. Epub 2008/11/01. eng
Landen CN, Chavez-Reyes A, Bucana C, Schmandt R, Deavers MT, Lopez-Berestein G: Therapeutic EphA2 gene targeting in vivo using neutral liposomal small interfering RNA delivery. Cancer Res. 2005, 65 (15): 6910-6918. 10.1158/0008-5472.CAN-05-0530. PubMed PMID: 16061675. Epub 2005/08/03. eng
Peer D, Karp JM, Hong S, Farokhzad OC, Margalit R, Langer R: Nanocarriers as an emerging platform for cancer therapy. Nat Nanotechnol. 2007, 2 (12): 751-760. 10.1038/nnano.2007.387. PubMed PMID: 18654426. Epub 2008/07/26. eng
Anderson DG, Akinc A, Hossain N, Langer R: Structure/property studies of polymeric gene delivery using a library of poly (beta-amino esters). Mol Ther. 2005, 11 (3): 426-434. 10.1016/j.ymthe.2004.11.015. PubMed PMID: 15727939. Epub 2005/02/25. eng
Akinc A, Zumbuehl A, Goldberg M, Leshchiner ES, Busini V, Hossain N: A combinatorial library of lipid-like materials for delivery of RNAi therapeutics. Nat Biotechnol. 2008, 26 (5): 561-569. 10.1038/nbt1402. PubMed PMID: 18438401. Epub 2008/04/29. eng
Leng Q, Scaria P, Lu P, Woodle MC, Mixson AJ: Systemic delivery of HK Raf-1 siRNA polyplexes inhibits MDA-MB-435 xenografts. Cancer Gene Ther. 2008, 15 (8): 485-495. 10.1038/cgt.2008.29. PubMed PMID: 18483501. Epub 2008/05/17. eng
Yan Z, Zou H, Tian F, Grandis JR, Mixson AJ, Lu PY: Human rhomboid family-1 gene silencing causes apoptosis or autophagy to epithelial cancer cells and inhibits xenograft tumor growth. Mol Cancer Ther. 2008, 7 (6): 1355-1364. 10.1158/1535-7163.MCT-08-0104. PubMed PMID: 18524845. Epub 2008/06/06. eng
Honma K, Iwao-Koizumi K, Takeshita F, Yamamoto Y, Yoshida T, Nishio K: RPN2 gene confers docetaxel resistance in breast cancer. Nat Med. 2008, 14 (9): 939-948. 10.1038/nm.1858. PubMed PMID: 18724378. Epub 2008/08/30. eng
Fujii T, Saito M, Iwasaki E, Ochiya T, Takei Y, Hayashi S: Intratumor injection of small interfering RNA-targeting human papillomavirus 18 E6 and E7 successfully inhibits the growth of cervical cancer. Int J Oncol. 2006, 29 (3): 541-548. PubMed PMID: 16865269. eng
Mu P, Nagahara S, Makita N, Tarumi Y, Kadomatsu K, Takei Y: Systemic delivery of siRNA specific to tumor mediated by atelocollagen: combined therapy using siRNA targeting Bcl-xL and cisplatin against prostate cancer. Int J Cancer. 2009, 125 (12): 2978-2990. 10.1002/ijc.24382. PubMed PMID: 19422046. Epub 2009/05/08. eng
Wolfrum C, Shi S, Jayaprakash KN, Jayaraman M, Wang G, Pandey RK: Mechanisms and optimization of in vivo delivery of lipophilic siRNAs. Nat Biotechnol. 2007, 25 (10): 1149-1157. 10.1038/nbt1339. PubMed PMID: 17873866. Epub 2007/09/18. eng
Nishina K, Unno T, Uno Y, Kubodera T, Kanouchi T, Mizusawa H: Efficient in vivo delivery of siRNA to the liver by conjugation of alpha-tocopherol. Mol Ther. 2008, 16 (4): 734-740. 10.1038/mt.2008.14. PubMed PMID: 18362929. eng
Lorenz C, Hadwiger P, John M, Vornlocher HP, Unverzagt C: Steroid and lipid conjugates of siRNAs to enhance cellular uptake and gene silencing in liver cells. Bioorg Med Chem Lett. 2004, 14 (19): 4975-4977. 10.1016/j.bmcl.2004.07.018. PubMed PMID: 15341962. Epub 2004/09/03. eng
Rozema DB, Lewis DL, Wakefield DH, Wong SC, Klein JJ, Roesch PL: Dynamic PolyConjugates for targeted in vivo delivery of siRNA to hepatocytes. Proc Natl Acad Sci U S A. 2007, 104 (32): 12982-12987. 10.1073/pnas.0703778104. PubMed PMID: 17652171. Pubmed Central PMCID: 1941806. Epub 2007/07/27. eng
Schiffelers RM, Ansari A, Xu J, Zhou Q, Tang Q, Storm G: Cancer siRNA therapy by tumor selective delivery with ligand-targeted sterically stabilized nanoparticle. Nucleic Acids Res. 2004, 32 (19): e149-10.1093/nar/gnh140. PubMed PMID: 15520458. Pubmed Central PMCID: 528817. Epub 2004/11/03. eng
Hu-Lieskovan S, Heidel JD, Bartlett DW, Davis ME, Triche TJ: Sequence-specific knockdown of EWS-FLI1 by targeted, nonviral delivery of small interfering RNA inhibits tumor growth in a murine model of metastatic Ewing’s sarcoma. Cancer Res. 2005, 65 (19): 8984-8992. 10.1158/0008-5472.CAN-05-0565. PubMed PMID: 16204072. eng
Davis ME, Zuckerman JE, Choi CH, Seligson D, Tolcher A, Alabi CA: Evidence of RNAi in humans from systemically administered siRNA via targeted nanoparticles. Nature. 2010, 464 (7291): 1067-1070. 10.1038/nature08956. PubMed PMID: 20305636. Pubmed Central PMCID: 2855406. Epub 2010/03/23. eng
Davis ME: The first targeted delivery of siRNA in humans via a self-assembling, cyclodextrin polymer-based nanoparticle: from concept to clinic. Mol Pharm. 2009, 6 (3): 659-668. 10.1021/mp900015y. PubMed PMID: 19267452. Epub 2009/03/10. eng
Chang C: The immune effects of naturally occurring and synthetic nanoparticles. J of Autoimmun. 2010, 34 (3): J234-246. 10.1016/j.jaut.2009.11.009. PubMed PMID: 19995678. Epub 2009/12/10. eng
Song E, Zhu P, Lee SK, Chowdhury D, Kussman S, Dykxhoorn DM: Antibody mediated in vivo delivery of small interfering RNAs via cell-surface receptors. Nat Biotechnol. 2005, 23 (6): 709-717. 10.1038/nbt1101. PubMed PMID: 15908939. Epub 2005/05/24. eng
Andrabi SM: Mammalian sperm chromatin structure and assessment of DNA fragmentation. J Assist Reprod Genet. 2007, 24 (12): 561-569. 10.1007/s10815-007-9177-y. PubMed PMID: 18008155. Epub 2007/11/17. eng
McNamara JO, Andrechek ER, Wang Y, Viles KD, Rempel RE, Gilboa E: Cell type-specific delivery of siRNAs with aptamer-siRNA chimeras. Nat Biotechnol. 2006, 24 (8): 1005-1015. 10.1038/nbt1223. PubMed PMID: 16823371. Epub 2006/07/11. eng
Sato Y, Murase K, Kato J, Kobune M, Sato T, Kawano Y: Resolution of liver cirrhosis using vitamin A-coupled liposomes to deliver siRNA against a collagen-specific chaperone. Nat Biotechnol. 2008, 26 (4): 431-442. 10.1038/nbt1396. PubMed PMID: 18376398. eng
Pirollo KF, Rait A, Zhou Q, Hwang SH, Dagata JA, Zon G: Materializing the potential of small interfering RNA via a tumor-targeting nanodelivery system. Cancer Res. 2007, 67 (7): 2938-2943. 10.1158/0008-5472.CAN-06-4535. PubMed PMID: 17409398. eng
Li SD, Chen YC, Hackett MJ, Huang L: Tumor-targeted delivery of siRNA by self-assembled nanoparticles. Mol Ther. 2008, 16 (1): 163-169. 10.1038/sj.mt.6300323. PubMed PMID: 17923843. Pubmed Central PMCID: 2739987. Epub 2007/10/10. eng
Kortylewski M, Swiderski P, Herrmann A, Wang L, Kowolik C, Kujawski M: In vivo delivery of siRNA to immune cells by conjugation to a TLR9 agonist enhances antitumor immune responses. Nat Biotechnol. 2009, 27 (10): 925-932. 10.1038/nbt.1564. PubMed PMID: 19749770. Epub 2009/09/15. eng
Kumar P, Ban HS, Kim SS, Wu H, Pearson T, Greiner DL: T cell-specific siRNA delivery suppresses HIV-1 infection in humanized mice. Cell. 2008, 134 (4): 577-586. 10.1016/j.cell.2008.06.034. PubMed PMID: 18691745. Epub 2008/08/12. eng
Kim SS, Subramanya S, Peer D, Shimaoka M, Shankar P: Antibody-mediated delivery of siRNAs for anti-HIV therapy. Methods Mol Biol. 2011, 721: 339-353. 10.1007/978-1-61779-037-9_21. PubMed PMID: 21431696. Epub 2011/03/25. eng
Subramanya S, Kim SS, Abraham S, Yao J, Kumar M, Kumar P: Targeted delivery of siRNA to human dendritic cells to suppress Dengue viral infection and associated proinflammatory cytokine production. J Virol. 2010, 84 (5): 2490-501. 10.1128/JVI.02105-08. PubMed PMID: 20015996. Epub 2009/12/18. Eng
Shimaoka M, Takagi J, Springer TA: Conformational regulation of integrin structure and function. Annu Rev Biophys Biomol Struct. 2002, 31: 485-516. 10.1146/annurev.biophys.31.101101.140922. PubMed PMID: 11988479. eng
Shimaoka M, Kim M, Cohen EH, Yang W, Astrof N, Peer D: AL-57, a ligand-mimetic antibody to integrin LFA-1, reveals chemokine-induced affinity up-regulation in lymphocytes. Proc Natl Acad Sci U S A. 2006, 103 (38): 13991-13996. 10.1073/pnas.0605716103. PubMed PMID: 16963559. Pubmed Central PMCID: 1599901. Epub 2006/09/12. eng
Peer D, Zhu P, Carman CV, Lieberman J, Shimaoka M: Selective gene silencing in activated leukocytes by targeting siRNAs to the integrin lymphocyte function-associated antigen-1. Proc Natl Acad Sci U S A. 2007, 104 (10): 4095-4100. 10.1073/pnas.0608491104. PubMed PMID: 17360483. Pubmed Central PMCID: 1820714. Epub 2007/03/16. eng
Cauli A, Yanni G, Pitzalis C, Challacombe S, Panayi GS: Cytokine and adhesion molecule expression in the minor salivary glands of patients with Sjogren’s syndrome and chronic sialoadenitis. Ann Rheum Dis. 1995, 54 (3): 209-215. 10.1136/ard.54.3.209. PubMed PMID: 7748018. eng
Tanaka Y, Mine S, Figdor CG, Wake A, Hirano H, Tsukada J: Constitutive chemokine production results in activation of leukocyte function-associated antigen-1 on adult T-cell leukemia cells. Blood. 1998, 91 (10): 3909-3919. PubMed PMID: 9573029. Epub 1998/06/20. eng
Peer D, Park EJ, Morishita Y, Carman CV, Shimaoka M: Systemic leukocyte-directed siRNA delivery revealing cyclin D1 as an anti-inflammatory target. Science. 2008, 319 (5863): 627-630. 10.1126/science.1149859. PubMed PMID: ISI:000252772000043. English
Peer D, Park EJ, Morishita Y, Carman CV, Shimaoka M: Systemic leukocyte-directed siRNA delivery revealing cyclin D1 as an anti-inflammatory target. Science. 2008, 319 (5863): 627-630. 10.1126/science.1149859. PubMed PMID: 18239128. Pubmed Central PMCID: 2490797. Epub 2008/02/02. eng
Kim SS, Peer D, Kumar P, Subramanya S, Wu H, Asthana D: RNAi-mediated CCR5 Silencing by LFA-1-targeted Nanoparticles Prevents HIV Infection in BLT Mice. Mol Ther. 2010, 18 (2): 370-6. 10.1038/mt.2009.271. PubMed PMID: 19997090. Epub 2009/12/10. Eng
Akinc A, Zumbuehl A, Goldberg M, Leshchiner ES, Busini V, Hossain N: A combinatorial library of lipid-like materials for delivery of RNAi therapeutics. Nat Biotechnol. 2008, 26 (5): 561-569. 10.1038/nbt1402. PubMed PMID: ISI:000255756800029. English
Semple SC, Akinc A, Chen J, Sandhu AP, Mui BL, Cho CK: Rational design of cationic lipids for siRNA delivery. Nat Biotechnol. 2010, 28 (2): 172-176. 10.1038/nbt.1602. PubMed PMID: 20081866. Epub 2010/01/19. eng
Geisbert TW, Lee ACH, Robbins M, Geisbert JB, Honko AN, Sood V: Postexposure protection of non-human primates against a lethal Ebola virus challenge with RNA interference: a proof-of-concept study. Lancet. 2010, 375 (9729): 1896-1905. 10.1016/S0140-6736(10)60357-1. PubMed PMID: ISI:000278628800031. English
Heidel JD, Yu ZP, Liu JYC, Rele SM, Liang YC, Zeidan RK: Administration in non-human primates of escalating intravenous doses of targeted nanoparticles containing ribonucleotide reductase subunit M2 siRNA. Proc Natl Acad Sci U S A. 2007, 104 (14): 5715-5721. 10.1073/pnas.0701458104. PubMed PMID: ISI:000245657600005. English
Frank-Kamenetsky M, Grefhorst A, Anderson NN, Racie TS, Bramlage B, Akinc A: Therapeutic RNAi targeting PCSK9 acutely lowers plasma cholesterol in rodents and LDL cholesterol in nonhuman primates. Proc Natl Acad Sci U S A. 2008, 105 (33): 11915-11920. 10.1073/pnas.0805434105. PubMed PMID: ISI:000258723800060. English
Haussecker D: The Business of RNAi Therapeutics in 2012. Mol Ther Nucleic Acids. 2012, 2 (8): 1-e8. doi:10.1038/mtna.2011.9
Lares MR, Rossi JJ, Ouellet DL: RNAi and small interfering RNAs in human disease therapeutic applications. Trends Biotechnol. 2010, 28 (11): 570-579. 10.1016/j.tibtech.2010.07.009. PubMed PMID: ISI:000283703300005. English
Acknowledgments
This work was supported in part by grants from the NIH (5R01CA139444-09), The Lewis Family Trust, Israel Science Foundation (Award #181/10), the I-CORE Program of the Planning and Budgeting Committee and The Israel Science Foundation (grant No 41/11) and the FTA: Nanomedicines for Personalized Theranostics of the Israeli National Nanotechnology Initiative and by The Leona M. and Harry B. Helmsley Nanotechnology Research Fund awarded to D.P.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interest
DP has financial interests in Quiet Therapeutics Ltd.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Peer, D. Harnessing RNAi nanomedicine for precision therapy. Mol and Cell Ther 2, 5 (2014). https://doi.org/10.1186/2052-8426-2-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2052-8426-2-5