Abstract
Background
Pancreatic adenocarcinoma (PCA) is one of the most lethal human malignancies, and radical surgery remains the cornerstone of treatment. After resection, the overall 5-year survival rate is only 10% to 29%. At the time of presentation, however, about 40% of patients generally have distant metastases and another 40% are usually diagnosed with locally advanced cancers. The remaining 20% of patients are indicated for surgery on the basis of the results of preoperative imaging studies; however, about half of these patients are found to be unsuitable for resection during surgical exploration. In the current study, we aimed to determine the clinicopathological characteristics that predict the resectability of PCA and to conduct a prognostic analysis of PCA after resection to identify favorable survival factors.
Methods
We retrospectively reviewed the medical files of 688 patients (422 men and 266 women) who had undergone surgery for histopathologically proven PCA in the Department of Surgery at Chang Gung Memorial Hospital in Taiwan from 1981 to 2006. We compared the clinical characteristics of patients who underwent resection and patients who did not undergo resection in order to identify the predictive factors for successful resectability of PCA, and we conducted prognostic analysis for PCA after resection.
Results
A carbohydrate antigen 19–9 (CA 19–9) level of 37 U/ml or greater and a tumor size of 3 cm or more independently predicted resectability of PCA. In terms of survival after resection, PCA patients with better nutritional status (measured as having an albumin level greater than 3.5 g/dl), radical resection, early tumor stage and better-differentiated tumors were associated with favorable survival.
Conclusions
Besides traditional imaging studies, preoperative CA 19–9 levels and tumor size can also be used to determine the resectability of PCA. Better nutritional status, curative resection, early tumor stage and well-differentiated tumors predict the favorable prognosis of PCA patients after resection.
Similar content being viewed by others
Background
Pancreatic adenocarcinoma (PCA) is one of the most lethal human malignancies and ranks as the eighth and ninth most common causes of cancer-related mortality worldwide for men and women, respectively [1]. In the United States in 2008, 37,680 new cases of PCA were diagnosed, and 34,290 PCA-related deaths occurred [2]. The incidence-to-mortality ratio was nearly 1:1, illustrating the lethality of PCA. The overall 5-year survival rate of patients with PCA is estimated to be approximately 1% to 4%, a percentage range that is likely related to the aggressive characteristics of PCA, such as early local spread and metastasis and resistance to radiotherapy and most systemic chemotherapies [3]. Currently, radical surgical resection is the cornerstone of treatment. After resection, the overall 5-year survival rate is only 10% to 29% [4–6]. However, previous studies have shown that, at the time of presentation, about 40% of patients have distant metastases and another 40% are diagnosed with locally advanced cancers [2, 3, 7]. The remaining 20% of patients are indicated for surgery on the basis of the results of preoperative imaging studies; however, about half of these patients are found to be unsuitable for resection during surgical exploration [8–12]. Unnecessary surgical exploration may, in turn, lead to increased surgical risk and healthcare costs and may delay systemic treatment [13].
Therefore, accurate preoperative prediction of PCA resectability is crucial to facilitating appropriate management of PCA patients. In the past few years, researchers have attempted to address this issue and have found that preoperative measurement of carbohydrate antigen 19–9 (CA 19–9) level, endoscopic ultrasonography (EUS), computed tomography (CT) and staging laparoscopy may enhance the accuracy of prediction of resectability before surgery [14–18].
Herein we retrospectively review the medical files of 688 PCA patients who underwent surgery at our hospital from 1981 to 2006 and identified the predictive factors for resectability of PCA by comparing the clinical characteristics of patients who underwent resection with those of patients who did not undergo resection. Furthermore, we also investigated the prognostic factors for favorable PCA outcomes following resection.
Methods
We retrospectively reviewed the medical files of 688 patients who had undergone surgery for histopathologically proven PCA in the Department of Surgery at Chang Gung Memorial Hospital in Taipei, Taiwan, from 1981 to 2006. This retrospective study was approved by the local institutional review board of Chang Gung Memorial Hospital (clinical study no. 94-955B).
Resection was defined as pancreatectomy (Whipple operation or distal pancreatectomy), regardless of the status of pancreatic resection margin. The patients comprised 422 men and 266 women with a median age of 64 years (range, 14 to 93 years). Of these patients, 230 underwent resection (the resection group), and the remaining 458 patients were unable to undergo resection because of portal vein invasion or carcinomatosis (the no-resection group). Surgical mortality was defined as death within 1 month of surgery. Laboratory tests were conducted 1 day before surgery. Serum CA 19–9 and carcinoembryonic antigen (CEA) levels were measured by radioimmunoassay. Tumors were preoperatively evaluated by abdominal ultrasonography, endoscopic retrograde cholangiopancreatography (ERCP), percutaneous transhepatic cholangiography (PTC), CT, magnetic resonance imaging with cholangiopancreatography (MRCP) and angiography, as appropriate. Tumor stage was defined according to the pathological tumor node metastasis (pTNM) classification proposed by the Union for International Cancer Control (UICC). Stages I and II represent early-stage PCA, and stages III and IV represent advanced-stage PCA. Patients with a tumoral resection margin or lymph node metastasis were given adjuvant chemotherapy consisting of a systemic 5-fluorouracil- or gemcitabine-based regimen. Adjuvant radiotherapy was conducted by intraoperative radiotherapy, external beam radiotherapy and/or brachytherapy in patients with either a positive section margin or local recurrence. The follow-up period ranged from 1 to 169.4 months, and, during follow-up, abdominal CT, chest X-ray, MRCP and tumor marker measurement were performed as appropriate. In terms of tumor size, we chose 3 cm as the cutoff value to investigate its impact on the resectablity of pancreatic cancer based on our own experience.
Statistical analysis
All data are presented as the proportion (%) of patients or as means with standard deviations. Numerical data were compared using independent Student’s t-tests. Nominal data were compared using Pearson’s χ2 test or forward stepwise multiple logistic regression, as appropriate. Survival rates were calculated and plotted using the Kaplan-Meier method. Clinicopathological variables, including demographic data, laboratory data, clinical features, pathological features and operative findings, were selected for survival analysis. We performed survival analysis using the logrank test and multivariate analysis using the Cox proportional hazards model. All statistical analyses were performed using the SPSS computer software package (version 10.0; Chicago, IL, USA). A P-value less than 0.05 was considered statistically significant.
Results
Survival of PCA patients
The median follow-up time for all patients in this study was 6.5 months (range, 1 to 169.4 months). For the resection group, the median follow-up time was 13 months (range, 1 to 169.4 months) and, for the no-resection group, the median follow-up time was 4.9 months (range, 1 to 65.7 months). Ninety-seven patients were excluded from the survival analysis because of lack of follow-up data or death within 1 month of surgery. The overall 1-, 3- and 5-year survival rates for the remaining 591 PCA patients were 29.7%, 8.8% and 5.1%, respectively. Patients in the resection group showed significantly better survival than patients in the no-resection group (Figure 1). The overall 3-year survival rate was significantly higher in the resection group (22.6%) than in the no-resection group (1.1%) (P < 0.0001). In addition, the PCA resection rate has increased significantly in our hospital over the past 3 decades, from, respectively, 16% to 27.7% to 48.8% for 1981 to 1999, 1991 to 2000 and 2001 to 2006 (P < 0.0001).
Predictive factors for resectability of PCA
Table 1 summarizes the clinicopathological features of the 688 PCA patients. There were 230 patients in the resection group and 458 patients in the no-resection group. The mean age in the resection group was significantly lower than that in the no-resection group (P = 0.047), and the resection group had a greater proportion of patients ages 65 years or younger (P = 0.015). The gender ratio in the two groups was similar. No differences were observed between the two groups with regard to preoperative physical examination findings, but patients in the no-resection group tended to be asymptomatic before the operation (P = 0.018). Tumor distribution (head or of the pancreas or not) was also similar in the two groups. Patients in the resection group showed higher albumin levels than those in the no-resection group (3.77 ± 0.65 g/dl versus 3.63 ± 0.17 g/dl; P = 0.025). Furthermore, the proportion of patients with albumin levels greater than 3.5 g/dl in the resection group was higher than that in the no-resection group (P = 0.02). The average of preoperative aspartate aminotransferase (AST) level was higher in the resection group than in the no-resection group. The bilirubin levels were similar in both groups. With regard to the serum levels of the tumor marker CA 19–9, we found lower mean CA 19–9 levels in the resection group than in the no-resection group, but the difference was not statistically significant. In addition, the proportion of patients with CA 19–9 levels above 37.0 U/ml in the no-resection group was higher than that in the resection group (P = 0.007). Similarly, CEA levels were higher in the no-resection group, and a higher proportion of patients in the no-resection group had CEA levels greater than 5 ng/ml. The mean tumor size in the no-resection group was 6.2 ± 3.5 cm, and that in the resection group was 4.61 ± 3.6 cm. Because we had set 3 cm as the cutoff value for tumor size, the no-resection group obviously showed a higher rate of tumors over 3 cm than the resection group. Moreover, the no-resection group had shorter operation times, fewer postoperative complications and lower mortality rates than the resection group did.
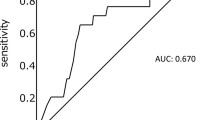
All significant predictive factors obtained in the univariate analysis (Table 1) were included in our multivariate analysis, which was performed using a logistic regression method. Only CA 19–9 level < 37 and tumor size < 3 cm were independent predictive factors for resectability of PCA.
Factors influencing the survival of PCA patients after resection
Univariate analysis (Table 2) indicated that women had a better prognosis than men (P = 0.02), with overall 3- and 5-year survival rates of 29.9% and 23.1%, respectively, for women and 3- and 5-year overall survival rates of 18.3% and 8.6%, respectively, for men. An albumin level greater than 3.5 g/dl was a favorable prognostic factor for survival after PCA resection (P = 0.024). Other factors, such as nontumoral resection margin, bilirubin levels of 1.3 mg/dl or less, CA 19–9 levels of 37 U/ml or less, no lymph node metastasis, early pTNM stage and well-differentiated tumors, were also associated with a better prognosis. On the other hand, age, preoperative physical examination findings and preoperative biochemical data (including levels of amylase, lipase and the tumor marker CEA) were not associated with patient survival after resection of PCA. Interestingly, we found that tumor location, operative procedure and portal vein resection were not related to patient survival after PCA resection.
In the analysis of the significant factors using the multivariate Cox proportional hazards method, we identified albumin levels greater than 3.5 g/dl (Figure 2a), nontumoral resection margin (Figure 2b), well-differentiated tumors (Figure 2c) and early pTNM stage (Figure 2d) as favorable prognostic factors after resection of PCA.
Discussion
Pancreatic cancer ranks as the fifth most common cause of cancer-related mortality worldwide, and patients with PCA generally have a very poor prognosis [3]. Radical surgical resection is the most effective treatment for PCA, because pancreatic tumors tend to respond poorly to both radiotherapy and chemotherapy. According to the results of previous studies, however, only 20% of PCA patients are considered suitable for resection prior to surgical exploration, and during surgical exploration, half of these patients are found to be unsuitable for resection because of the advanced stage of the tumor [7].
Recent improvements in radiological imaging techniques have decreased the rate of unnecessary surgical exploration; however, the current state of PCA resectability prediction remains unsatisfactory [19–21]. Thus far the method of choice for diagnosing and staging PCA is thin-section, contrast-enhanced, triple-phase CT [22, 23]. This method can result in a 90% to 100% predictive value for the unresectability of PCA [14, 24–26], but only a 52% to 96% predictive value for resectability has been reported [8, 11, 24, 27, 28]. Other methods, such as EUS or 2-18F]-fluoro-2-deoxy-d-glucose positron emission tomography (FDG-PET) is also unable to provide satisfactory predictive value regarding resectablity before surgery [16, 29–32]. Taken together, these studies demonstrate that no imaging studies can yet provide a complete picture of the preoperative status of PCA to clinical physicians, and thus further investigation of potential ancillary predictive factors is warranted.
In this study, we identified the clinicopathological features of PCA patients that may be useful for predicting the resectability of PCA. Physicians can use these ancillary predictive factors, in combination with traditional imaging studies, to determine the resectability of PCA with increased accuracy.
In the current study, patients in the resection group were, on average, 2 years younger than those in the no-resection group (62 versus 64 years old; P = 0.047), and the resection group comprised a greater proportion of patients ages 65 years or younger (P = 0.015). This observation suggests that there may be a 2-year period during which PCA progresses from being resectable to becoming unresectable. We also found that CA 19–9 level 37 U/ml or less and tumor size 3 cm or less were independent factors predicting the resectability of PCA. Furthermore, patients in the resection group had longer operation times. The results of our study suggest that both CA 19–9 (≤37 U/ml) and tumor size (≤3 cm) could be used as ancillary parameters to determine the resectability of PCA (odds ratios, 2.458 and 3.155, respectively).
Serological markers of malignancy are widely used as adjuncts to the results of imaging studies for diagnosing malignancy and predicting prognosis. CA 19–9, initially detected by Koprowaki et al. [33], is the most well-established tumor marker for PCA, with higher sensitivity and specificity than CEA, CA 50, and CA 242 [34–36]. Some recent studies have emphasized the importance of preoperative CA 19–9 levels in determining the resectability of PCA [15, 37]. Maithel et al. recommended staging laparoscopy for patients whose CA 19–9 levels exceeded 130.0 U/ml and who were diagnosed with resectable PCA as indicated by radiography [17]. In our study, a lower percentage of patients in the resection group had preoperative CA 19–9 levels greater than 37 U/ml, while CEA levels failed to independently predict the resectability of PCA, an observation that is in line with previous reports [34–36]. Although many studies have investigated the relationship between tumor size and prognosis in PCA [38–40], few studies have associated tumor size with resectability. In the current study, we found that tumor size (cutoff value, 3 cm) could be used to predict the resectability of PCA independently.
For decades, researchers have attempted to determine the factors predictive of favorable outcomes after resection of PCA. In contrast to the study conducted by Schmidt et al., our present study did not show that CEA level could be used as a prognostic factor for PCA following tumor resection [41]; however, researchers in other studies have reported findings similar to ours [38, 42]. CA 19–9 level has been widely reported to be a prognostic factor for PCA after tumor resection [40, 43, 44]. Schmidt et al. [41] also demonstrated that increased bilirubin predicted unfavorable survival outcomes after PCA resection. In our study CEA, however, neither CA 19–9 nor bilirubin independently indicated a worse outcome after PCA resection. Interestingly, in addition to well-established indicators of survival, such as resection margin status, tumor stage and histological differentiation, we identified serum albumin as an independent prognostic factor after resection of PCA in our study. Albumin has previously been shown to be related to the prognosis of cancer patients [45, 46]. In pancreatic cancer, Ruiz-Tovar et al. reported that the preoperative serum albumin level (with the cutoff value set at 2.8 g/dl) could be used as a prognostic factor for PCDA [47]. Malnutrition has long been deemed a severe problem involving complex mechanisms in cancer patients [48]. The lower serum albumin concentration in advanced cancer patients may be due to the release of some cytokines such as interleukin 6 or TNF, to suppression of hepatocyte production of albumin, or to increased capillary permeability to albumin by the tumor or its surrounding tissues [46, 49]. For example, in conditions of liver metastasis existing, Kupffer cells in the liver would be stimulated to produce interleukin 6 and TNF. Taken together, serum albumin could be deemed a good indicator of cancer survival. In this study, albumin levels greater than 3.5 g/dl were found to be associated with a better prognosis for PCA survival after resection.
Conclusion
On the basis of our study results, we propose that preoperative CA 19–9 levels and tumor size less than 3 cm can be used as auxiliary parameters, in combination with traditional imaging studies, to determine the resectability of PCA. Furthermore, albumin levels, resection margin status, tumor stage and histological differentiation can be used as prognostic factors for survival after resection of PCA.
Consent statement
This study has been approved by Chang Gung memorial hospital IRB board. The approved IRB number is 94-955B. A copy of the approval of IRB is available for review by the Editor-in-Chief of this journal.
Foundation
This work was supported by Chang Gung Medical Research Program (CMRP) grant 280271G and 280272G to Dr. Kun-Chun Chiang.
Abbreviations
- TNF:
-
Tumor necrosis factor.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D: Global cancer statistics. CA Cancer J Clin. 2011, 61: 69-90. 10.3322/caac.20107.
American Cancer Society: Cancer Facts & Figures 2008. 2008, Atlanta: American Cancer Society,http://www.cancer.org/acs/groups/content/@nho/documents/document/2008cafffinalsecuredpdf.pdf,
Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ: Cancer statistics, 2007. CA Cancer J Clin. 2007, 57: 43-66. 10.3322/canjclin.57.1.43.
Trede M, Schwall G, Saeger HD: Survival after pancreatoduodenectomy: 118 consecutive resections without an operative mortality. Ann Surg. 1990, 211: 447-458. 10.1097/00000658-199004000-00011.
Yeo CJ, Cameron JL, Sohn TA, Lillemoe KD, Pitt HA, Talamini MA, Hruban RH, Ord SE, Sauter PK, Coleman J, Zahurak ML, Grochow LB, Abrams RA: Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, and outcomes. Ann Surg. 1997, 226: 248-260. 10.1097/00000658-199709000-00004.
Nitecki SS, Sarr MG, Colby TV, van Heerden JA: Long-term survival after resection for ductal adenocarcinoma of the pancreas. Is it really improving?. Ann Surg. 1995, 221: 59-66. 10.1097/00000658-199501000-00007.
Haller DG: New perspectives in the management of pancreas cancer. Semin Oncol. 2003, 30: 3-10.
Ellsmere J, Mortele K, Sahani D, Maher M, Cantisani V, Wells W, Brooks D, Rattner D: Does multidetector-row CT eliminate the role of diagnostic laparoscopy in assessing the resectability of pancreatic head adenocarcinoma?. Surg Endosc. 2005, 19: 369-373. 10.1007/s00464-004-8712-5.
Gulliver DJ, Baker ME, Cheng CA, Meyers WC, Pappas TN: Malignant biliary obstruction: efficacy of thin-section dynamic CT in determining resectability. AJR Am J Roentgenol. 1992, 159: 503-507.
Prokesch RW, Chow LC, Beaulieu CF, Bammer R, Jeffrey RB: Isoattenuating pancreatic adenocarcinoma at multi-detector row CT: secondary signs. Radiology. 2002, 224: 764-768. 10.1148/radiol.2243011284.
Saldinger PF, Reilly M, Reynolds K, Raptopoulos V, Chuttani R, Steer ML, Matthews JB: Is CT angiography sufficient for prediction of resectability of periampullary neoplasms?. J Gastrointest Surg. 2000, 4: 233-237. 10.1016/S1091-255X(00)80071-2.
Spitz FR, Abbruzzese JL, Lee JE, Pisters PW, Lowy AM, Fenoglio CJ, Cleary KR, Janjan NA, Goswitz MS, Rich TA, Evans DB: Preoperative and postoperative chemoradiation strategies in patients treated with pancreaticoduodenectomy for adenocarcinoma of the pancreas. J Clin Oncol. 1997, 15: 928-937.
Parsons CM, Sutcliffe JL, Bold RJ: Preoperative evaluation of pancreatic adenocarcinoma. J Hepatobiliary Pancreat Surg. 2008, 15: 429-435. 10.1007/s00534-007-1240-7.
Clarke DL, Thomson SR, Madiba TE, Sanyika C: Preoperative imaging of pancreatic cancer: a management-oriented approach. J Am Coll Surg. 2003, 196: 119-129. 10.1016/S1072-7515(02)01609-5.
Zhang S, Wang YM, Sun CD, Lu Y, Wu LQ: Clinical value of serum CA19-9 levels in evaluating resectability of pancreatic carcinoma. World J Gastroenterol. 2008, 14: 3750-3753. 10.3748/wjg.14.3750.
Ho JM, Eysselein VE, Stabile BE: The value of endoscopic ultrasonography in predicting resectability and margins of resection for periampullary tumors. Am Surg. 2008, 74: 1026-1029.
Maithel SK, Maloney S, Winston C, Gonen M, D’Angelica MI, Dematteo RP, Jarnagin WR, Brennan MF, Allen PJ: Preoperative CA 19–9 and the yield of staging laparoscopy in patients with radiographically resectable pancreatic adenocarcinoma. Ann Surg Oncol. 2008, 15: 3512-3520. 10.1245/s10434-008-0134-5.
Klauss M, Mohr A, von Tengg-Kobligk H, Friess H, Singer R, Seidensticker P, Kauczor HU, Richter GM, Kauffmann GW, Grenacher L: A new invasion score for determining the resectability of pancreatic carcinomas with contrast-enhanced multidetector computed tomography. Pancreatology. 2008, 8: 204-210. 10.1159/000128557.
Varadhachary GR, Tamm EP, Crane C, Evans DB, Wolff RA: Borderline resectable pancreatic cancer. Curr Treat Options Gastroenterol. 2005, 8: 377-384. 10.1007/s11938-005-0040-x.
Takhar AS, Palaniappan P, Dhingsa R, Lobo DN: Recent developments in diagnosis of pancreatic cancer. BMJ. 2004, 329: 668-673. 10.1136/bmj.329.7467.668.
Misek DE, Patwa TH, Lubman DM, Simeone DM: Early detection and biomarkers in pancreatic cancer. J Natl Compr Canc Netw. 2007, 5: 1034-1041.
Delbeke D, Pinson CW: Pancreatic tumors: role of imaging in the diagnosis, staging, and treatment. J Hepatobiliary Pancreat Surg. 2004, 11: 4-10. 10.1007/s00534-002-0775-x.
Sahani DV, Shah ZK, Catalano OA, Boland GW, Brugge WR: Radiology of pancreatic adenocarcinoma: current status of imaging. J Gastroenterol Hepatol. 2008, 23: 23-33. 10.1111/j.1440-1746.2007.04868.x.
Diehl SJ, Lehmann KJ, Sadick M, Lachmann R, Georgi M: Pancreatic cancer: value of dual-phase helical CT in assessing resectability. Radiology. 1998, 206: 373-378.
Legmann P, Vignaux O, Dousset B, Baraza AJ, Palazzo L, Dumontier I, Coste J, Louvel A, Roseau G, Couturier D, Bonnin A: Pancreatic tumors: comparison of dual-phase helical CT and endoscopic sonography. AJR Am J Roentgenol. 1998, 170: 1315-1322.
Lu DS, Reber HA, Krasny RM, Kadell BM, Sayre J: Local staging of pancreatic cancer: criteria for unresectability of major vessels as revealed by pancreatic-phase, thin-section helical CT. AJR Am J Roentgenol. 1997, 168: 1439-1443.
Steinberg WM, Barkin J, Bradley EL, Di Magno E, Layer P: Workup of a patient with a mass in the head of the pancreas. Pancreas. 1998, 17: 24-30. 10.1097/00006676-199807000-00002.
Conlon KC, Dougherty E, Klimstra DS, Coit DG, Turnbull AD, Brennan MF: The value of minimal access surgery in the staging of patients with potentially resectable peripancreatic malignancy. Ann Surg. 1996, 223: 134-140. 10.1097/00000658-199602000-00004.
Rose DM, Delbeke D, Beauchamp RD, Chapman WC, Sandler MP, Sharp KW, Richards WO, Wright JK, Frexes ME, Pinson CW, Leach SD: 18Fluorodeoxyglucose-positron emission tomography in the management of patients with suspected pancreatic cancer. Ann Surg. 1999, 229: 729-738. 10.1097/00000658-199905000-00016.
Sendler A, Avril N, Helmberger H, Stollfuss J, Weber W, Bengel F, Schwaiger M, Roder JD, Siewert JR: Preoperative evaluation of pancreatic masses with positron emission tomography using 18F-fluorodeoxyglucose: diagnostic limitations. World J Surg. 2000, 24: 1121-1129. 10.1007/s002680010182.
Delbeke D, Rose DM, Chapman WC, Pinson CW, Wright JK, Beauchamp RD, Shyr Y, Leach SD: Optimal interpretation of FDG PET in the diagnosis, staging and management of pancreatic carcinoma. J Nucl Med. 1999, 40: 1784-1791.
Nakamoto Y, Higashi T, Sakahara H, Tamaki N, Kogire M, Imamura M, Konishi J: Contribution of PET in the detection of liver metastases from pancreatic tumours. Clin Radiol. 1999, 54: 248-252. 10.1016/S0009-9260(99)91160-1.
Koprowski H, Steplewski Z, Mitchell K, Herlyn M, Herlyn D, Fuhrer P: Colorectal carcinoma antigens detected by hybridoma antibodies. Somatic Cell Genet. 1979, 5: 957-971. 10.1007/BF01542654.
Wu X, Lu XH, Xu T, Qian JM, Zhao P, Guo XZ, Yang XO, Jiang WJ: [The diagnostic value of serum carcinoma markers, fecal K-ras and p53 gene mutation in pancreatic cancers] [in Chinese]. Zhonghua Nei Ke Za Zhi. 2005, 44: 741-744.
Okusaka T, Okada S, Sato T, Wakasugi H, Saisho H, Furuse J, Ishikawa O, Matsuno S, Yokoyama S: Tumor markers in evaluating the response to radiotherapy in unresectable pancreatic cancer. Hepatogastroenterology. 1998, 45: 867-872.
Liao Q, Zhao YP, Yang YC, Li LJ, Long X, Han SM: Combined detection of serum tumor markers for differential diagnosis of solid lesions located at the pancreatic head. Hepatobiliary Pancreat Dis Int. 2007, 6: 641-645.
Kiliç M, Göçmen E, Tez M, Ertan T, Keskek M, Koç M: Value of preoperative serum CA 19–9 levels in predicting resectability for pancreatic cancer. Can J Surg. 2006, 49: 241-244.
Han SS, Jang JY, Kim SW, Kim WH, Lee KU, Park YH: Analysis of long-term survivors after surgical resection for pancreatic cancer. Pancreas. 2006, 32: 271-275. 10.1097/01.mpa.0000202953.87740.93.
Moon HJ, An JY, Heo JS, Choi SH, Joh JW, Kim YI: Predicting survival after surgical resection for pancreatic ductal adenocarcinoma. Pancreas. 2006, 32: 37-43. 10.1097/01.mpa.0000194609.24606.4b.
Shimada K, Sakamoto Y, Sano T, Kosuge T: Prognostic factors after distal pancreatectomy with extended lymphadenectomy for invasive pancreatic adenocarcinoma of the body and tail. Surgery. 2006, 139: 288-295. 10.1016/j.surg.2005.08.004.
Schmidt CM, Powell ES, Yiannoutsos CT, Howard TJ, Wiebke EA, Wiesenauer CA, Baumgardner JA, Cummings OW, Jacobson LE, Broadie TA, Canal DF, Goulet RJ, Curie EA, Cardenes H, Watkins JM, Loehrer PJ, Lillemoe KD, Madura JA: Pancreaticoduodenectomy: a 20-year experience in 516 patients. Arch Surg. 2004, 139: 718-727. 10.1001/archsurg.139.7.718.
Ni XG, Bai XF, Mao YL, Shao YF, Wu JX, Shan Y, Wang CF, Wang J, Tian YT, Liu Q, Xu DK, Zhao P: The clinical value of serum CEA, CA19-9, and CA242 in the diagnosis and prognosis of pancreatic cancer. Eur J Surg Oncol. 2005, 31: 164-169. 10.1016/j.ejso.2004.09.007.
Ferrone CR, Finkelstein DM, Thayer SP, Muzikansky A, Fernandez-del Castillo C, Warshaw AL: Perioperative CA19-9 levels can predict stage and survival in patients with resectable pancreatic adenocarcinoma. J Clin Oncol. 2006, 24: 2897-2902. 10.1200/JCO.2005.05.3934.
Berger AC, Meszoely IM, Ross EA, Watson JC, Hoffman JP: Undetectable preoperative levels of serum CA 19–9 correlate with improved survival for patients with resectable pancreatic adenocarcinoma. Ann Surg Oncol. 2004, 11: 644-649. 10.1245/ASO.2004.11.025.
Sirott MN, Bajorin DF, Wong GY, Tao Y, Chapman PB, Templeton MA, Houghton AN: Prognostic factors in patients with metastatic malignant melanoma: a multivariate analysis. Cancer. 1993, 72: 3091-3098. 10.1002/1097-0142(19931115)72:10<3091::AID-CNCR2820721034>3.0.CO;2-V.
McMillan DC, Watson WS, O’Gorman P, Preston T, Scott HR, McArdle CS: Albumin concentrations are primarily determined by the body cell mass and the systemic inflammatory response in cancer patients with weight loss. Nutr Cancer. 2001, 39: 210-213. 10.1207/S15327914nc392_8.
Ruiz-Tovar J, Martín-Pérez E, Fernández-Contreras ME, Reguero-Callejas ME, Gamallo-Amat C: Impact of preoperative levels of hemoglobin and albumin on the survival of pancreatic carcinoma [English and Spanish]. Rev Esp Enferm Dig. 2010, 102: 631-636.
von Meyenfeldt M: Cancer-associated malnutrition: an introduction. Eur J Oncol Nurs. 2005, 9 (Suppl 2): S35-S38.
Barber MD, Ross JA, Fearon KC: Changes in nutritional, functional, and inflammatory markers in advanced pancreatic cancer. Nutr Cancer. 1999, 35: 106-110. 10.1207/S15327914NC352_2.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
K-CC wrote the manuscript, S-HU carried out the pathological examination, J-TH helped write the manuscript, T-SY helped write the manuscript,Y-YJ participated in data collection, T-LH helped write the manuscript, M-FC helped review this manuscript. C-NY finalized the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Chiang, KC., Yeh, CN., Ueng, SH. et al. Clinicodemographic aspect of resectable pancreatic cancer and prognostic factors for resectable cancer. World J Surg Onc 10, 77 (2012). https://doi.org/10.1186/1477-7819-10-77
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7819-10-77