Abstract
Background
Vitamin D has been shown to exert manifold immunomodulatory effects. Type 1 diabetes mellitus (T1DM) is regarded to be immune-mediated and vitamin D prevents the development of diabetes in the NOD mouse. We studied the association between T1DM and the initiation codon polymorphism in exon 2 of the vitamin D receptor gene in a Japanese population. We also investigated associations between the vitamin D receptor polymorphism and GAD65-antibody (Ab) positivity. We carried out polymerase chain reaction-restriction fragment length polymorphism analysis in 110 Japanese T1DM patients and 250 control subjects. GAD65 antibodies were assessed in 78 patients with T1DM.
Results
We found a significantly higher prevalence of the F allele / the FF genotype in the patients compared to the controls (P = 0.0069 and P = 0.014, respectively). Genotype and allele frequencies differed significantly between GAD65-Ab-positive patients and controls (P = 0.017 and P = 0.012, respectively), but neither between GAD65-Ab-negative patients and controls (P = 0.68 and P = 0.66, respectively) nor between GAD65-Ab-positive and -negative patients (P = 0.19 and P = 0.16, respectively).
Conclusions
Our findings suggest that the vitamin D receptor initiation codon polymorphism influences genetic susceptibility to T1DM among the Japanese. This polymorphism is also associated with GAD65-Ab-positive T1DM, although the absence of a significant difference between GAD65-Ab-negative patients and controls might be simply due to the small sample size of patients tested for GAD65 antibodies.
Similar content being viewed by others
Background
Type 1 diabetes mellitus (T1DM) is a multifactorial disease with a strong genetic component [1]. The main genetic contribution to T1DM susceptibility lies in the major histocompatibility complex (MHC) on the short arm of chromosome 6; several non-MHC chromosomal regions are also involved [2]. Several approaches have been used to identify T1DM susceptibility regions, including case-control studies of candidate genes [human leukocyte antigen (HLA), insulin gene regulatory region, interleukin-1 receptor type 1 (ILIR1)] [3,4,5,6], combined linkage and association-based studies of candidate genes [cytotoxic T lymphocyte associated-4 (CTLA-4)] [7], and systematic total genome searches in addition to analyses of individual chromosomal regions [8,9,10,11,12,13,14,15,16].
There are clear differences in immunogenetic predisposition to T1DM between countries, and disease incidence seems to vary along with these differences in predisposition [1]. The incidence of T1DM in Southern India (10.4/100000 cases per year) is similar to that in Asian children in the UK and Caucasian children of European extraction [17,18]. While an MHC component is apparent [19,20] in T1DM susceptibility in Southern India, no association with either the insulin gene [20] or ILIR1 [6] has been found there in case-control studies. This suggests possible differences in the non-MHC T1DM component between Southern Indians and Caucasians of European extraction. In the latter population, an association with the insulin gene has been universally reported [4,5,21], and an IL1R1 association with T1DM has been reported in some Northern Europeans [6,22].
VDR gene polymorphisms influence susceptibility to osteoporosis [23,24,25], primary hyperparathyroidism [26,27], and autoimmune diseases such as Graves' disease [28,29], Hashimoto's thyroiditis [30], and multiple sclerosis [31]. Allelic variation in VDR also influences susceptibility to T1DM in Indian Asians [17], Germans [32], and Taiwanese [33]. There are six known polymorphisms in the VDR locus: an exon 2 initiation codon polymorphism, which is detected with FokI restriction enzyme [34,35,36,37], the BsmI, Tru9I, and ApaI restriction fragment length polymorphisms (RFLPs) located between exons 8 and 9 [23,38], the TaqI RFLP located in exon 9 [23], and a poly A polymorphism downstream of the 3' untranslated region [39,40]. There is apparently no significant linkage disequilibrium between the FokI polymorphism and the BsmI, ApaI, and TaqI polymorphisms [34,35,36,37]. In this study, we analyzed the exon 2 initiation codon (VDR-FokI) gene polymorphism in Japanese patients with T1DM. We also investigated associations between this VDR polymorphism and GAD65 antibody (Ab) status, an immune marker.
Subjects and Methods
Subjects
The study population comprised 110 unrelated Japanese T1DM patients (50 men and 60 women) from the Tokyo metropolitan area. T1DM was diagnosed on the basis of sudden-onset of severe symptoms or rapid progress to overt diabetes and dependence on exogenous insulin due to absolute insulin deficiency, according to the 1997 Committee of the American Diabetes Association (Expert Committee on the Diagnosis and Classification of Diabetes Mellitus, 1997) criteria. All subjects were insulin-dependent at the time of the study, although their β-cell reserve, estimated by measurement of fasting serum C-peptide, was variable. Slowly progressive T1DM was not included in this study. Mean age at onset of T1DM was 26.0 ± 3.7 years (mean ± SEM). GAD65 antibodies were assessed in 78 patients. Two hundred and fifty unrelated Japanese subjects (100 men and 150 women) without clinical evidence or family history of diabetes mellitus or autoimmune disease were selected as controls. The controls used in the present study are identical with the previously published controls [28,29,30]. This study was carried out in accordance with the principles of the Declaration of Helsinki. Informed consent was obtained from patients and controls.
Genotype analysis
Genomic DNA was isolated from whole blood with the Genomix kit (Talent, Trieste, Italy). Primers VDR2a (5'-AGCTGGCCCTGGCACTGACTCTTGCTCT-3') and VDR2b (5'-ATGGAAACACCTTGCTTCTTCTCCCTC-3') and 100 ng of genomic DNA were combined in a polymerase chain reaction (PCR) mixture to amplify a 265-bp fragment containing the polymorphism in the initiation codon of VDR [34]. PCR products were digested with FokI at 37°C for 3 h and then subjected to electrophoresis in 2% agarose gel containing ethidium bromide. Cleavage of homozygous DNA carrying the FokI polymorphism (FF) generates 69-bp and 196-bp fragments. Restriction endonuclease cleavage analysis of DNA heterozygous for the FokI polymorphism (Ff) results in uncleaved (265-bp) DNA as well as the 69-bp and 196-bp products. Homozygous DNA that does not carry the FokI polymorphism (ff) is not cleaved by FokI and appears as a single 265-bp fragment on agarose gels.
Measurement of GAD65 antibody
GAD65 Ab was detected with a radioligand binding assay described previously [41]. Intra- and inter-assay coefficients of variation were less than 5%. At the First International GAD Autoantibody Workshop, our GAD65 Ab assay yielded 100% sensitivity (% positive samples confirmed to be positive) and 100% specificity (% known negative samples confirmed to be negative).
Statistical analysis
Genotypes and alleles in patients and controls were compared with the Χ2-tests for 2 × 2 and 2 × 3 tables and by Fisher's exact test. Relative risk was calculated by Woolf's method [42]. P < 0.05 was considered significant. We corrrected for multiple testing using the Bonferoni correction.
Results
Genotype and allele frequencies of the VDR-FokI gene polymorphism in patients and controls
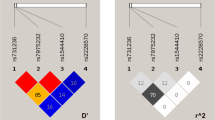
PCR-RFLP was used to examine VDR-FokI genotype distributions in T1DM patients and controls (Table 1). The distribution of VDR genotypes was similar between the male and female control subjects (data not shown). The genotype distribution in our control subjects was similar to that in a previously reported group of Japanese women who resided in Kagawa prefecture [25].
The distribution of genotype frequencies differed significantly between T1DM patients and controls (Χ2 = 8.48, 2 degrees of freedom, P = 0.014), with the VDR FF genotype occurring more frequently in the T1DM patients. The distribution of allele frequencies differed significantly between T1DM patients and controls (Χ2 = 7.29, 1 degree of freedom, P = 0.0069). The relative risk conferred by at least one F allele (FF or Ff) was 2.4.
Genotype distributions among patients and controls did not differ according to age, height, or weight (data not shown). No significant linkage disequilibrium was detected between this polymorphism and the BsmI polymorphism in intron 8 and exon 9 in the T1DM patients (data not shown).
VDR-FokI gene polymorphism in GAD65-antibody-positive and -negative subjects
We investigated association between VDR-FokI gene polymorphism and GAD65-Ab positivity in 78 patients (Table 2). The distribution of genotype frequencies differed significantly between GAD65-Ab-positive patients and controls (Χ2 = 8.14, 2 degrees of freedom, P = 0.017). The distribution of allele frequencies also differed significantly between GAD65-Ab-positive T1DM patients and controls (Χ2 = 6.32, 1 degree of freedom, P = 0.012). The relative risk conferred by at least one F allele (FF or Ff) was 2.0. The distribution of genotype and allele frequencies did not differ significantly between GAD65-Ab-negative T1DM patients and controls (Χ2 = 0.78, 2 degrees of freedom, P = 0.68 and Χ2 = 0.19, 1 degree of freedom, P = 0.66). The genotype and allele distributions in the GAD65-Ab-positive and -negative patients did not differ significantly (Χ2 = 3.36, 2 degrees of freedom, P = 0.19 and Χ2 = 1.98, 1 degree of freedom, P = 0.16, respectively).
Discussion
We found an association between the VDR-FokI polymorphism and T1DM in our study population. Selective β-cell destruction, which is observed in T1DM, is thought to be caused by a T-cell-mediated autoimmune process [43]. Genetic susceptibility to T1DM is well established, and certain HLA pheno- and genotypes are associated with T1DM; for example, HLA-DR 3 and -DR 4 in Caucasian populations [43], and HLA-DR 4 and -DR 9 in Japanese populations [44]. Recent genome-wide searches and several candidate gene studies have revealed new regions possibly associated with T1DM [8,9,10,11,12,13,14,15,16,45,46].
Vitamin D hormone has important immunomodulatory properties and influences insulin secretion [47]. This hormone inhibits T-cell activation both in vitro and in vivo and the secretion of IL-1, IL-2, IL-6, IL-12, TNF, and interferon (IFN)-γ [48,49,50,51]. These cytokines play important roles in the development of T cells, which are believed to be involved in the pathogenesis of several chronic inflammatory autoimmune diseases [52]. In recent studies, 1,25-dihydroxyvitamin D3 was shown to inhibit IL-12 production by macrophages and dendritic cells by suppressing transcriptional activation of the p35 and p45 genes, which code for subunits of IL-12. Transcriptional repression of the p40 gene is dependent on expression of VDR [53]. In murine models, vitamin D administration prevents development of T1DM as well as the associated autoimmune insulitis [54]. In Bangladeshi subjects, vitamin D levels were found to be reduced in those subjects most at risk for type 2 diabetes [55].
The VDR locus has been studied extensively for association with susceptibility to osteoporosis [23,24,25], primary hyperparathyroidism [26,27], and autoimmune diseases such as Graves' disease [28,29], Hashimoto's thyroiditis [30], and multiple sclerosis [31]. The BsmI B allele of VDR has been associated with reduced bone mineral density in some studies [23,56], but not in others [57,58], and at least one study showed the b allele of VDR to be associated with particular subtypes of osteoporosis [59]. The bb genotype has been associated with primary hyperparathyroidism in Swedish patients [26,27] and multiple sclerosis in Japanese patients [31]. The FokI FF genotype for VDR has been associated with both Graves' disease [28] and Hashimoto's thyroiditis [30] in Japanese patients.
The role of the VDR gene in T1DM has also been examined [17,32]. Evidence for preferential transmission of the VDR b allele to affected offspring has been found in Indian Asians [17]. Pani et al. [32] detected significant haplotype-wise extended transmission disequilibrium for the BsmI/ApaI/TaqI, BsmI/TaqI, and ApaI/TaqI haplotypes in Germans; analysis of the FokI site did not provide additional information on susceptibility. Recently, Chang et al. confirmed the association of these markers with T1DM in the Taiwanese population [33]. Allelic frequencies for this and other VDR RFLPs (ApaI, TaqI) differ between Caucasian and Japanese subjects [24,60]. RFLP analysis of VDR revealed that the BBAAtt genotype is relatively common (16.7%) in Caucasian populations and rare in Japanese populations (1.4%) [24]. Therefore, we investigated VDR-FokI polymorphism in this study. Our investigation of VDR-FokI genotype frequencies in Japanese subjects revealed that the FF genotype is significantly more common in T1DM patients (47%) than in control subjects (33%), suggesting that patients with this genotype may be predisposed to T1DM [28].
In contrast to our findings for T1DM, an increased frequency of the F allele, because it encodes a VDR isoform with higher transcriptional activity, has a beneficial effects in the prevention of osteoporosis, and should lead to higher immunomodulatory activity of the vitamin D hormone [61]. Recently, Colin et al. [62] demonstrated in peripheral blood mononuclear cells with a natural VDR genotype a direct functional consequence of the VDR-FokI polymorphism for the action of 1,25-dihydroxyvitamin D3. They found that the FF genotype had a significant lower ED50 than the Ff genotype corresponding to an allele dose effect of 0.32 nM per f allele copy (P = 0.0036), while for BsmI genotypes no differences in ED50 were observed [62]. The apparent discrepancy could be due to the effect of the genetic susceptibility to T1DM and ethnic differences related to VDR-FokI allelic prevalences as well as to environmental and geographic variations in calcium intake, exposure to sunshine, or other factors.
In the present study, the FF genotype (or presence of the F allele) of the VDR-FokI polymorphism was also associated with GAD65-Ab-positive T1DM in the Japanese population, although the absence of a significant difference between GAD65-Ab-negative patients and controls might be simply due to the small sample size of patients tested for GAD65 antibodies. McDermott et al. [17] found no relation between the VDR-BsmI, -TaqI, or -ApaI polymorphism and GAD65 Ab status in Indian Asians. Thus, since there is apparently no linkage disequilibrium between FokI polymorphism and BsmI, ApaI, and TaqI polymorphisms [34,35,36,37], the VDR-FokI polymorphism seems to contribute to immunological heterogeneity of T1DM, although the mechanism remains unclear. Although no in vitro or animal studies have shown that VDR function is directly associated with antibody production in autoimmune disease or that this polymorphism might alter immune function, GAD65-Ab-negative diabetes patients could be subject to a different disease process or a different path of clinical development with regards to a possible VDR contribution. Both possibilities warrant further study.
Conclusions
In conclusion, our data indicates an association between the VDR gene and T1DM among the Japanese. We suggest that the FF genotype may predispose Japanese individuals to T1DM and that this genotype appears to be a marker for T1DM. The role of the VDR gene polymorphism should be studied further in other populations, and other polymorphisms, such as the BsmI, ApaI, Tru9I and TaqI polymorphisms, should be analyzed for association with T1DM susceptibility. In addition, the VDR-FokI polymorphism showed a possible association with GAD65-Ab-positive T1DM. The VDR plays a role in lymphocyte response to microorganisms (tuberculin reactive status in pulmonary tuberculosis, leprosy etc.). Thus, it is conceivable that it may also be involved in immune response to self antigens e.g. GAD65 antibodies.
References
Atkinson MA, MacLaren NK: Mechanisms of disease: the pathogenesis of insulin-dependent diabetes mellitus. N Engl J Med. 1994, 331: 1428-1436. 10.1056/NEJM199411243312107.
Cordell HJ, Todd JA: Multifactorial inheritance in type 1 diabetes. Trends Genet. 1995, 11: 499-503. 10.1016/S0168-9525(00)89160-X.
Nerup J, Platz P, Ortved-Anderson O, Christy M, Lynsgoe J, Poulsen JE: HLA antigens and diabetes mellitus. Lancet. 1974, 2: 864-866.
Bell GI, Horita S, Karam JH: A polymorphic marker near the human insulin gene is associated with insulin dependent diabetes mellitus. Diabetes. 1984, 33: 176-183.
Hitman GA, Tarn AC, Winter RM, et al: Type 1 (insulin-dependent) diabetes and a highly variable locus close to the insulin gene on chromosome 11. Diabetologia. 1985, 28: 218-222.
Metcalfe KA, Hitman GA, Pociot F, et al: An association between type 1 diabetes and the interleukin-1 receptor type 1 gene. Hum Immunol. 1996, 51: 41-48. 10.1016/S0198-8859(96)00206-6.
Nistico L, Buzzetti R, Pritchard LE, et al: The CTLA-4 gene region of chromosome 2q33 is linked to, and associated with, type 1 diabetes. Hum Mol Genet. 1996, 5: 1075-1080. 10.1093/hmg/5.7.1075.
Davies JL, Kawaguchi Y, Bennett ST, et al: A genome-wide search for human type 1 diabetes susceptibility genes. Nature. 1994, 371: 130-136. 10.1038/371130a0.
Field LL, Tobias R, Magnus T: A locus on chromosome 15q26 (IDDM3) produces susceptibility to insulin dependent diabetes mellitus. Nat Genet. 1994, 8: 189-194.
Hanis CL, Boerwinkle E, Chakraborty R, et al: A genome-wide search for human non-insulin dependent (type 2) diabetes genes reveals a major susceptibility locus on chromosome 2. Nat Genet. 1996, 13: 161-167.
Luo DF, Buzzetti R, Rotter JI, et al: Confirmation of three susceptibility genes to insulin-dependent diabetes mellitus: IDDM4, IDDM5 and IDDM8. Hum Mol Genet. 1996, 5: 693-698. 10.1093/hmg/5.5.693.
Luo DF, Bui MM, Muir A, Maclaren NK, Thomsen G, She J-X: Affected sibpair mapping of a novel susceptibility gene to insulin-dependent diabetes mellitus (IDDM8) on chromosome 6q25-q27. Am J Hum Genet. 1995, 51: 911-919.
Owerbach D, Gabbay KM: The HOXD8 locus (2q31) is linked to type 1 diabetes. Diabetes. 1995, 44: 132-136.
Morahan G, Huang D, Tait BD, Colman PG, Harrison LC: Markers on distal chromosome 2q linked to insulin-dependent diabetes mellitus. Science. 1996, 272: 1811-1813.
Hashimoto L, Habita C, Beressi JP, et al: Genetic mapping of a susceptibility locus for insulin-dependent diabetes mellitus on chromosome 11q. Nature. 1994, 371: 161-164. 10.1038/371161a0.
Copeman JB, Cucca F, Hearne CM, et al: Linkage disequilibrium mapping of a type 1 diabetes susceptibility gene (IDDM7) to chromosome 2q31-q33. Nat Genet. 1995, 9: 80-85.
McDermott MF, Ramachandran A, Ogunkolade BW, et al: Allelic variation in the vitamin D receptor influences susceptibility to IDDM in Indian Asians. Diabetologia. 1997, 40: 971-975. 10.1007/s001250050776.
Gujral JS, McNally PG, Botha JL, Burden AC: Childhood-onset diabetes in the white and South Asian population in Leicestershire, UK. Diabet Med. 1994, 11: 570-572.
Serjeantson SW, Ranford PR, Kirk RL, et al: HLA-DR and -DQ genotyping in insulin-dependent diabetes patients in South India. Dis Markers. 1987, 5: 101-108.
Kambo PK, Hitman GA, Mohan V, et al: The genetic predisposition to fibrocalculous pancreatic diabetes. Diabetologia. 1989, 32: 45-51.
Julier C, Hyer RN, Davies J, et al: Insulin-IGF2 region on chromosome 11p encodes a gene implicated in HLA-DR4-dependent diabetes susceptibility. Nature. 1991, 354: 155-159. 10.1038/354155a0.
Bergholdt R, Karlsen AE, Johannesen J, et al: Chracterization of polymorphisms of an interleukin-1 receptor type 1 gene (IL1R1) promoter region (P2) and their relation to insulin-dependent diabetes mellitus (IDDM). Cytokine. 1995, 7: 727-733. 10.1006/cyto.1995.0086.
Morrison NA, Qi JC, Tokita A, et al: Prediction of bone density from vitamin D receptor alleles. Nature. 1994, 367: 284-287. 10.1038/367284a0.
Tokita A, Matsumoto H, Morrison NA, et al: Vitamin D receptor alleles, bone mineral density and turnover in premenopausal Japanese women. J Bone Miner Res. 1996, 11: 1003-1009.
Arai H, Miyamoto K, Taketani Y, et al: A vitamin D receptor gene polymorphism in the translation initiation codon: effect on protein activity and relation to bone mineral density in Japanese women. J Bone Miner Res. 1997, 12: 915-921.
Carling T, Kindmark A, Hellman P, et al: Vitamin D receptor genotypes in primary hyperparathyroidism. Nat Med. 1995, 1: 1309-1311.
Carling T, Åkerström G, Rastad J, Westin G: Vitamin D receptor (VDR) and parathyroid hormone mRNA levels correspond to polymorphic VDR alleles in human parathyroid tumors. J Clin Endocrinol Metab. 1998, 83: 2255-2259.
Ban Y, Ban Y, Taniyama M, Katagiri T: Vitamin D receptor initiation codon polymorphism in Japanese patients with Graves' disease. Thyroid. 2000, 10: 375-380.
Ban Y, Taniyama M, Ban Y: Vitamin D Receptor Gene Polymorphism is Associated with Graves' Disease in the Japanese Population. J Clin Endocrinol Metab. 2000, 85: 4639-4643.
Ban Y, Taniyama M, Ban Y: Vitamin D Receptor Gene Polymorphisms in Hashimoto's thyroiditis. Thyroid. 2001, 11: 607-608. 10.1089/10507250175030296710.1089/105072501750302967.
Fukazawa T, Yabe I, Kikuchi S, et al: Association of vitamin D receptor gene polymorphism with multiple sclerosis in Japanese. J Neurol Sci. 1999, 166: 47-52. 10.1016/S0022-510X(99)00112-4.
Pani MA, Knapp M, Donner H, et al: Vitamin D receptor allele combinations influence genetic susceptibility to type 1 diabetes in Germans. Diabetes. 2000, 49: 504-507.
Chang T-J, Lei H-H, Yeh J-I, et al: Vitamin D receptor gene polymorphisms influence susceptibility to type 1 diabetes mellitus in the Taiwanese population. Clin Endocrinol (Oxf). 2000, 52: 575-580. 10.1046/j.1365-2265.2000.00985.x.
Gross C, Eccleshall T, Malloy P, Villa M, Marcus R, Feldman D: The presence of a polymorphism at the translation initiation site of the vitamin D receptor is associated with low bone mineral density in postmenopausal Mexican-American women. J Bone Miner Res. 1996, 11: 1850-1855.
Eccleshall T, Garnero P, Gross C, Delmas P, Feldman D: Lack of correlation between start codon polymorphism of the vitamin D receptor gene and bone mineral density in premenopausal French women: The OFELY study. J Bone Miner Res. 1998, 13: 31-35.
Harris S, Eccleshall T, Gross C, Dawson-Hughes B, Feldman D: The vitamin D receptor start codon polymorphism (FokI) and bone mineral density in premenopausal American black and white women. J Bone Miner Res. 1997, 12: 1043-1048.
Ferrari S, Rixxoli R, Manen D, Slosman D, Bonjour JP: Vitamin D receptor gene start codon polymorphisms (FokI) and bone mineral density: interaction with age, dietary calcium, and 3'-end region polymorphism. J Bone Miner Res. 1998, 13: 925-930.
Ye W-Z, Reis AF, Velho G: Identification of a novel Tru9I polymorphism in the human vitamin D receptor gene. J Hum Genet. 2000, 45: 56-57. 10.1007/s100380050011.
Ingles SA, Haile RW, Henderson BE, et al: Strength of linkage disequilibrium between two vitamin D receptor markers in five ethnic groups: implications for association studies. Cancer Epidemiol Biomarkers Prev. 1997, 6: 93-98.
Ingles SA, Ross RK, Yu MC, et al: Association of prostate cancer risk with genetic polymorphisms in vitamin D receptor and androgen receptor. J Natl Cancer Inst. 1997, 89: 166-170. 10.1093/jnci/89.2.166.
Kasuga A, Maruyama T, Ozawa Y, et al: Antibody to the Mr 65,000 isoform of glutamic acid decarboxylase are detected in non-insulin-dependent diabetes mellitus in Japanese. J Autoimmun. 1996, 9: 105-111. 10.1006/jaut.1996.0013.
Woolf B: On estimating the relation between blood group and disease. Ann Hum Genet. 1955, 19: 251-253.
Bach J-F: Insulin-dependent diabetes mellitus as an autoimmune disease. Endocr Rev. 1994, 15: 516-542.
Matsuda A, Kuzuya T, Iwamoto Y, et al: HLA DR antigens in adult-onset and juvenile-onset Japanese insulin-dependent diabetic patients. Diabetes Res Clin Pract. 1988, 5: 107-112.
Mein CA, Esposito L, Dunn MG, et al: A search for type 1 diabetes susceptibility genes in families from the United Kingdom. Nat Genet. 1998, 19: 297-300. 10.1038/991.
Concannon P, Gogolin-Ewens KJ, Hinds DA, et al: A second generation screen of the human genome for susceptibility to insulin-dependent diabetes mellitus. Nat Genet. 1998, 19: 292-296. 10.1038/985.
Frankel BJ, Heldt AM, Grodsksy GM: Vitamin D deficiency inhibits pancreatic secretion of insulin. Science. 1980, 209: 823-825.
Muller K, Bendtzen K: Inhibition of human T lymphocyte proliferation and cytokine production by 1,25-dihydroxyvitamin D3. Differential effects on CD45RA+ and CD45RO+ cells. Autoimmunity. 1992, 14: 37-43.
Bhalla AK, Amento EP, Serog B, Glimcher LH: 1,25-Dihydroxyvitamin D inhibits antigen-induced T cell activation. J Immunol. 1984, 133: 1748-1754.
Rigby WFC, Denome S, Fanger MW: Regulation of lymphokine production and human T lymphocyte activation by 1,25-dihydroxyvitamin D3. J Clin Invest. 1987, 79: 1659-1664.
Lemire JM: Immunomodulatory actions of 1,25-dihydroxyvitamin D3. J Steroid Biochem Mol Biol. 1995, 53: 599-602. 10.1016/0960-0760(95)00106-A.
Trembleau S, Germann T, Gately MK, Adorini L: The role of IL-12 in the induction of organ-specific autoimmune diseases. Immunol Today. 1995, 16: 383-386. 10.1016/0167-5699(95)80006-9.
D'Ambrosio D, Cippitelli M, Cocciolo MG, et al: Inhibition of IL-12 production by 1,25-dihydroxyvitamin D3. Involvement of NF-κB downregulation in transcriptional repression of the p40 gene. J Clin Invest. 1998, 101: 252-262.
Mathieu C, Laureys J, Sobis H, Vandeputte M, Waer M, Bouillon R: 1,25-dihydroxyvitamin D3 prevents insulitis in NOD mice. Diabetes. 1992, 41: 1491-1495.
Boucher BJ, Mannan N, Noonan K, Hales CN, Evans SJW: Glucose intolerance and impairment of insulin secretion in relation to vitamin D deficiency in East London Asians. Diabetologia. 1995, 38: 1239-1245. 10.1007/s001250050418.
Fleet JC, Harris SS, Wood RJ, Dawson-Hughes B: The BsmI vitamin D receptor restriction fragment length polymorphism (BB) predicts low bone density in premenopausal black and white women. J Bone Miner Res. 1995, 10: 985-990.
Riggs BL, Nguyen TV, Melton LJ, et al: The contribution of vitamin D receptor gene alleles to the determination of bone mineral density in normal and osteoporotic women. J Bone Miner Res. 1995, 10: 991-996.
Hustmyer FG, Peacock M, Hui S, Johnston CC, Christian J: Bone mineral density in relation to polymorphism at the vitamin D receptor gene locus. J Clin Invest. 1994, 94: 2130-2134.
Uitterlinden AG, Pols HA, Burger H, et al: A large scale population-based study of the association of vitamin D receptor gene polymorphisms with bone mineral density. J Bone Miner Res. 1996, 11: 1241-1248.
Yamagata Z, Miyamura T, Iijima S, et al: Vitamin D receptor gene polymorphism and bone mineral density in healthy Japanese women. Lancet. 1994, 344: 1027-10.1016/S0140-6736(94)91690-X.
Haussler MR, Whitfield GK, Haussler CA, et al: The nuclear vitamin D receptor: biological and molecular regulatory properties revealed. J Bone Miner Res. 1998, 13: 325-349.
Colin EM, Weel AEAM, Uitterlinden AG, et al: Consequences of vitamin D receptor gene polymorphisms for growth inhibition of cultured human peripheral blood mononuclear cells by 1,25-dihydroxyvitamin D3. Clin Endocrinol (Oxf). 2000, 52: 211-216. 10.1046/j.1365-2265.2000.00909.x.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/content/backmatter/1471-2350-2-7-b1.pdf
Acknowledgments
This work was supported, in part, by the High-Technology Research Center Project from the Ministry of Education, Science, Sports and Culture of Japan.
Competing interests
Have you in the past five years received reimbursements, fees, funding, or salary from an organisation that may in any way gain or lose financially from the publication of this paper? No.
Do you hold any stocks or shares in an organisation that may in any way gain or lose financially from the publication of this paper? No.
Do you have any other financial competing interests? No.
Are there any non-financial competing interests you would like to declare in relation to this paper? No.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ban, Y., Taniyama, M., Yanagawa, T. et al. Vitamin D receptor initiation codon polymorphism influences genetic susceptibility to type 1 diabetes mellitus in the Japanese population. BMC Med Genet 2, 7 (2001). https://doi.org/10.1186/1471-2350-2-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2350-2-7