Abstract
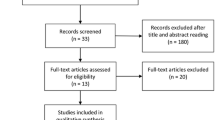
Introduction: Sleep-disordered breathing (SDB) is detected in 70% of stroke patients and impedes functional rehabilitation; it also increases the length of hospital stay and the risk of stroke recurrence and fatal outcome. Objective: To study the dynamics of SDB in its correlation with neurological disorders in stroke patients and to develop the approaches to optimization of early rehabilitation. Materials and methods: Seventy eight patients with acute ischemic stroke were examined. SDB was verified by cardiorespiratory monitoring; neurological deficit was assessed with the NIHSS and mRS scales. Examination was performed upon admission (days 2–5 post stroke) and repeated 3 weeks after. The effect of SDB correction on neurological recovery was studied for positional therapy (elevated head of bed by 30°) in combination with oxygen therapy (insufflation of O2 with maintenance of saturation level not less than 95% under digital sensor control). Results: Upon admission, SDB was revealed in 88% of patients; moderate and severe disorders being predominant (the apnea/hypopnea index (AHI) ≥ 15 h–1), most frequently presenting as obstructive apnea. In patients with AHI < 15 h–1, the positive dynamics of neurological disorders (p < 0.04) was observed along with stable SDB parameters. Neurological improvement (р < 0.05) was present in patients with AHI ≥ 15 h–1, which was associated with lesser severity of SDB. A direct correlation between the severity of neurological disorders and AHI after 3 weeks from the onset was revealed: RNIHSS/AHI = 0.45 (р = 0.003) and RmRS/AHI = 0.44 (р = 0.004). Patients with AHI ≥ 15 h–1 were divided into 2 groups: group A (no interventions) and group B (with application of positional and oxygen therapy in the night sleep during 7 days). A positive effect of therapy on restoration of neurological functions, along with a decrease in AHI, was revealed. Conclusions: SDB is a frequent and persistent disorder in patients with ischemic stroke. Early detection and correction of SDB should be regarded as an important component of post-stroke rehabilitation.
Similar content being viewed by others
REFERENCES
Insul’t: diagnostika, lechenie, profilaktika (Stroke: Diagnostics, Treatment, and Prevention), Suslina, Z.A. and Piradov, M.A., Eds., Moscow: MEDpress-inform, 2008.
Gudkova, V.V., Stakhovskaya, L.V., Kirilchenko, T.D., et al., Early rehabilitation after a stroke, Consilium Med., 2005, vol. 7, no. 8, pp. 692–696.
Kistenev, B.A., Fonyakin, A.V., Geraskina, L.A., and Petrova, E.A., Transient sick sinus syndrome as a manifestation of cerebrocardial syndrome in the acute period of stroke, Nevrol. Zh., 2003, no. 2, pp. 16–20.
Saposnik, G., Kapral, M.K., Liu, Y., et al., IScore: a risk score to predict death early after hospitalization for an acute ischemic stroke, Circulation, 2011, vol. 123, pp. 739–749. PMID 21300951. doi 10.1161/CIRCULA-TIONAHA.110.983353
Wessendorf, T.E., Wang, Y.M., Thilmann, A.F., et al., Treatment of obstructive sleep apnoea with nasal continuous positive airway pressure in stroke, Eur. Respir. J., 2001, vol. 18, pp. 623–629. PMID 11716165
Hermann, D.M. and Bassetti, C.L., Sleep-related breathing and sleep-wake disturbances in ischemic stroke, Neurology, 2009, vol. 73, pp. 1313–1322. PMID 19841384. doi 10.1212/WNL.0b013e3181bd137c
Kaneko, Y., Hajek, V.E., Zivanovic, V., et al., Relationship of sleep apnea to functional capacity and length of hospitalization following stroke, Sleep, 2003, vol. 26, no. 3, pp. 293–297. PMID 12749548
Rola, R., Jarosz, H., Wierzbicka, A., et al., Sleep disordered breathing and recurrence of cerebrovascular events, case-fatality, and functional outcome in patients with ischemic stroke or transient ischemic attack, J. Physiol. Pharmacol., 2008, vol. 59, no. 6, pp. 615–621. PMID 19218688
Sahlin, C., Sandberg, O., Gustafson, Y., et al., Obstructive sleep apnea is a risk factor for death in patients with stroke: a 10-year follow-up, Arch. Int. Med., 2008, vol. 168, pp. 297–301. PMID 18268171. doi 10.1001/archinternmed.2007.70
Shi, Y.-F. and Wang, Y.-P., Sleep-disordered breathing: impact on functional outcome of ischemic stroke patients, Sleep Med., 2009, vol. 10, pp. 717–719. PMID 19168390. doi 10.1016/j.sleep.2008.08.006
Martínez-García, M.A., Soler-Cataluña, J.J., Ejarque-Martínez, L., et al., Continuous positive airway pressure treatment reduces mortality in patients with ischemic stroke and obstructive sleep apnea: a 5-year follow-up study, Am. J. Respir. Crit. Care Med., 2009, vol. 180, no. 1, pp. 36–41. PMID 19406983. doi 10.1164/rccm.200808-1341OC
Parra, O., Sánchez-Armengol, A., Bonnin, M., et al., Early treatment of obstructive apnoea and stroke outcome: a randomized controlled trial, Eur. Respir. J., 2011, vol. 37, pp. 1128–1136. PMID 20847081. doi 10.1183/09031936.00034410
Bravata, D.M., Concato, J., Fried, T., et al., Continuous positive airway pressure: evaluation of a novel therapy for patients with acute ischemic stroke, Sleep, 2011, vol. 34, no. 9, pp. 1271–1277. PMID 21886365. doi 10.5665/SLEEP.1254
Kernan, W.N., Ovbiagele, B., Black, H.R., et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association, Stroke, 2014, vol. 45, pp. 2160–2236. doi 10.1161/STR. 0000000000000024
Hsu, C.Y., Vennelle, M., Li H.Y., et al., Sleep-disordered breathing after stroke: a randomised controlled trial of continuous positive airway pressure, J. Neurol. Neurosurg. Psychiatry, 2006, vol. 77, no. 10, pp. 1143–1149. PMID 2077531. doi 10.1136/jnnp.2005.08668
Ryan, C.M., Bayley, M., Green, R., et al., Influence of continuous positive airway pressure on outcomes of rehabilitation in stroke patients with obstructive sleep apnea, Stroke, 2011, vol. 42, no. 4, pp. 1062–1067. PMID 21372306. doi 10.1161/STROKEAHA. 110.597468
Svatikova, A., Chervin, R.D., Wing, J.J., et al., Positional therapy in ischemic stroke patients with obstructive sleep apnea, Sleep Med., 2011, vol. 12, pp. 262–266. PMID 21306949. doi 10.1016/j.sleep.2010.12.008
Mareev, V.Yu., Ageev, F.T., Arutyunov, G.P., Koroteev, A.V., et al., National recommendations of VNOK and SSHF on the diagnostics and treatment of chronic heart failure (third review): Approved by OSSN Conference, December 15, 2009, Zh. Serdechnaya Nedostatochn., 2010, vol. 11, no. 1 (57), pp. 3–62.
Warlow, C.P., Dennis, M.S., van Gijn, J., et al., Stroke: A Practical Guide to Management, Oxford: Blackwell, 1996.
Vereshchagin, N.V., Bragina, L.K., Vavilov, S.B., and Levina, G.Ya., Komp’yuternaya tomografiya mozga (Computer Tomography of the Brain), Moscow: Meditsina, 1986.
Tsara, V., Amfilochiou, A., Papagrigorakis, M.J., et al., Guidelines for diagnosis and treatment of sleep-related breathing disorders in adults and children. Definition and classification of sleep related breathing disorders in adults: different types and indications for sleep studies (Part 1), Hippokratia, 2009, vol. 13, no. 3, pp. 187–191. PMID 19918312
Young, T., Peppard, P.E., and Gottlieb, D.J., Epidemiology of obstructive sleep apnea: a population health perspective, Am. J. Respir. Crit. Care Med., 2002, vol. 165, pp. 1217–1239. doi 10.1164/rccm.2109080
Young, T., Palta, M., Dempsey, J., et al., Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study, Wis. Med. J., 2009, vol. 108, no. 5, pp. 246–249. PMID 19743755. PMCID PMC2858234.
Peppard, P.E., Young, T., Barnet, J.H., et al., Increased prevalence of sleep-disordered breathing in adults, Am. J. Epidemiol., 2013, vol. 177, no. 9, p. 1006. doi 10.1161/STROKEAHA.111.000112
Kapur, V.K., Obstructive sleep apnea: diagnosis, epidemiology, and economics, Respir. Care, 2010, vol. 55, pp. 1155–1167. PMID 20799998
Young, T., Peppard, P.E., and Taheri, S., Excess weight and sleep-disordered breathing, J. Appl. Physiol., 2005, vol. 99, no. 4, pp. 1592–1599. doi 10.1152/japplphysiol.00587.2005
Garvey, J.F., Pengo, M.F., Drakatos, P., and Kent, B.D., Epidemiological aspects of obstructive sleep apnea, J. Thorac. Dis., 2015, vol. 7, no. 5, pp. 920–929. doi 10.3978/j.issn.2072-1439.2015.04.52
Lutokhin, G.M., Geraskina, L.A., and Fonyakin, A.V., Sleep disordered breathing in ischemic stroke, Zh. Nevropatol. Psikhiatr. im. S.S. Korsakova, 2016, no. 12-2, pp. 14–20. doi 10.17116/jnevro201611612214-20
Eckert, D.J., Jordan, A.S., Merchia, P., and Malhotra, A., Central sleep apnea: pathophysiology and treatment, Chest J., 2007, vol. 131, no. 2, pp. 595–607. doi 10.1378/chest.06.2287
Plum, F. and Posner, B.J., The Diagnosis of Stupor and Coma, Philadelphia: F.A. Davis, 1966.
Bassetti, C., Aldrich, M., Chervin, R., and Quint, D., Sleep apnea in acute phase of TIA and stroke, Neurology, 1996, vol. 47, pp. 1167–1173. PMID 8909424
Parra, O., Arboix, A., Bechich, S., et al., Time course of sleep-related breathing disorders in first-ever stroke or transient ischemic attack, Am. J. Respir. Crit. Care Med., 2000, vol. 161, pp. 375–380. PMID 10673174. doi 10.1164/ajrccm.161.2.9903139
Bassetti, C.L., Milanova, M., and Gugger, M., Sleep-disordered breathing and acute ischemic stroke: diagnosis, risk factors, treatment, evolution, and long-term clinical outcome, Stroke, 2006, vol. 37, no. 4, pp. 967–972. PMID 16543515. doi 10.1161/01.STR. 0000208215.49243.c3
Harbison, J., Ford, G.A., James, O.F., and Gibson, G.J., Sleep-disordered breathing following acute stroke, Q. J. Med., 2002, vol. 95, pp. 741–747. PMID 12391386
Shepard, J.W., Hypertension, cardiac arrhythmias, myocardial infarction, and stroke in relation to obstructive sleep apnea, Clin. Chest, 1992, vol. 13, pp. 437–458. PMID 1521412
Garvey, J.F., Taylor, C.T., and McNicholas, W.T., Cardiovascular disease in obstructive sleep apnea syndrome: the role of intermittent hypoxia and inflammation, Eur. Respir. J., 2009, vol. 33, pp. 1195–1205. doi 10.1183/09031936.00111208
Sandberg, O., Franklin, K.A., Bucht, G., et al., Nasal continuous positive airway pressure in stroke patients with sleep apnea: a randomized treatment study, Eur. Respir. J., 2001, vol. 18, no. 4, pp. 630–634. PMID 11716166
Palombini, L. and Guilleminault, C., Stroke and treatment with nasal CPAP, Eur. J. Neurol., 2006, vol. 13, pp. 198–200. PMID 16490054. doi 10.1111/j.1468-1331.2006.01169.x
Mehta, V., Vasu, T.S., Phillips, B., and Chung, F., Obstructive sleep apnea and oxygen therapy: a systematic review of the literature and meta-analysis, J. Clin. Sleep Med., 2013, vol. 9, no. 3, pp. 271–279. PMID 23493498. PMCID PMC3578679. doi 10.5664/jcsm.2500
Epstein, L.J., Kristo, D., Strollo, P.J., et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults, J. Clin. Sleep Med., 2009, vol. 5, no. 3, pp. 263–276. PMID 19960649. PMCID PMC2699173.
Pevernagie, D.A., Stanson, A.W., Sheedy, P.F., et al., Effects of body position on the upper airway of patients with obstructive sleep apnea, Am. J. Respir. Crit. Care Med., 1995, vol. 152, pp. 179–185. PMID 7599821. doi 10.1164/ajrccm.152.1.7599821
Ravesloot, M.J.L., van Maanen, J.P., Dun, L., and de Vries, N., The undervalued potential of positional therapy in position-dependent snoring and obstructive sleep apnea—a review of the literature, Sleep Breath, 2013, vol. 17, pp. 39–49. doi 10.1007/s11325-012-0683-5
Brunser, A.M., Muñoz Venturelli, P., Lavados, P.M., et al., Head position and cerebral blood flow in acute ischemic stroke patients: Protocol for the pilot phase, cluster randomized, Head Position in Acute Ischemic Stroke Trial (HeadPoST pilot), Int. J. Stroke, 2016, vol. 11, no. 2, pp. 253–259. PMID 26783317. doi 10.1177/1747493015620808
2017 International Stroke Conference. http://news. heart.org/international-stroke-conference-2017/.
Author information
Authors and Affiliations
Corresponding author
Additional information
The article is published in the original.
Rights and permissions
About this article
Cite this article
Lutokhin, G.M., Geraskina, L.A., Fonyakin, A.V. et al. Optimization of Early Rehabilitation of Patients with Ischemic Stroke and Sleep-Disordered Breathing. Hum Physiol 44, 875–882 (2018). https://doi.org/10.1134/S0362119718080066
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0362119718080066