Abstract
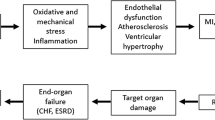
Carvedilol is a novel, multiple-action cardiovascular drug that is currently approved in many countries for the treatment of hypertension. The reduction in blood pressure produced by carvedilol results primarily from β-adrenoceptor blockade and vasodilation, the latter resulting from α_1-adrenoceptor blockade. These actions, as well as several of the other activities of carvedilol, are associated with cardioprotection in animal models that occurs to a degree that is greater than that observed with other drugs. The multiple actions of carvedilol may also provide the underlying rationale for the use of the drug in the treatment of coronary artery disease and congestive heart failure. By virtue of being both a beta-blocker and a vasodilator, carvedilol significantly decreases myocardial work by reducing all three components of myocardial oxygen demand, namely, heart rate, contractility, and wall tension. The vasodilatory effects of carvedilol reduce afterload, and the resulting decrease in impedance to left ventricular ejection offsets the negative inotropic effect that would normally result from beta-blockade. As a consequence, stroke volume and cardiac output are maintained or even increased in animals and in patients with congestive heart failure who are treated with carvedilol. Carvedilol and several of its metabolites are potent antioxidants, and this activity may account, in part, for the cardioprotective effects of the drug observed in animal models of acute myocardial ischemia and, in theory, could also serve to protect the myocardium of patients with hypertension, coronary artery disease, and congestive heart failure, in which oxidative stress is now recognized to occur. The antioxidant effects of carvedilol may both inhibit the direct cytotoxic actions of reactive oxygen radicals and prevent oxygen-radical induced activation of transcription factors and genes associated with inflammatory and remodeling processes. Accordingly, carvedilol inhibits the gene expression of the intracellular adhesion molecule-1 (ICAM-1), an adhesion molecule for polymorphonuclear leukocytes, which typically infiltrate the myocardium under conditions of ischemia and may exacerbate ischemic injury. The antioxidant activity of carvedilol has been shown to inhibit the oxidation of low density lipoprotein (LDL) in vitro, thereby preventing the formation of this cytotoxic and atherogenic form of LDL. It follows, therefore, that in animal models of hyperlipidemia, carvedilol attenuates aortic lipid accumulation and decreases the aortic content of monocytes and foam cells, and at the same time it has been shown to preserve endothelial integrity and function. These actions of carvedilol are not shared by other beta-blockers or by other drugs currently used in the management of hypertension, coronary artery disease, or congestive heart failure. The multiple actions of carvedilol may provide the underlying pharmacologic rationale for the use of this drug in the treatment of patients with coronary artery disease or congestive heart failure, and these actions may account, at least in part, for the reduction in mortality produced by carvedilol in clinical trials involving patients with congestive heart failure. Likewise, these actions of carvedilol may also provide protection, beyond that afforded from reduction in blood pressure, against secondary organ damage in hypertensive patients treated with the drug.
Similar content being viewed by others
References
Ruffolo RR Jr, Gellai M, Hieble JP, Willette RN, Nichols AJ. The pharmacology of carvedilol. Eur J Clin Pharmacol 1990;38:S82-S88.
Nichols AJ, Gellai M, Ruffolo RR Jr. Studies on the mechanism of arterial vasodilation produced by the novel antihypertensive agent, Carvedilol, Fund Clin Pharmacol 1991;5:25–38.
Feuerstein GZ, Ruffolo RR Jr. Carvedilol, a novel multiple action antihypertensive agent with antioxidant activity and the potential for myocardial and vascular protection. Eur Heart J 1995;16:38–42.
Gellai M, DeWolf R, Ruffolo RR Jr. Effect of carvedilol on renal hemodynamics and renal excretory function in spontaneously hypertensive rats. Pharmacology 1990;41:200–206.
Lysko PG, Lysko KA, Yue T-L, Webb CL, Gu J-L, Feuerstein GZ. Neuroprotective effects of carvedilol, a new antihypertensive agent, in cultured rat cerebellar neurons and in gerbil global brain ischemia. Stroke 1992;23:1630–1636.
Ohlstein EH, Douglas SA, Sung CP, Yue T-L, Louden C, Arleth A, Poste G, Ruffolo RR, Feuerstein GZ. Carvedilol, a cardiovascular drug, prevents vascular smooth muscle cell proliferation, migration, and neointimal formation following vascular injury. Proc Natl Acad Sci USA 1993;90:6189–6193.
Feuerstein GZ, Hamburger SA, Smith EF, Bril A, Ruffolo RR. Myocardial protection with carvedilol. J Cardiovas Pharmacol 1992;19(Suppl 1):S138-S141.
Inamura T, Sato J, Nishimura H, et al. The effect of carvedilol on atherosclerosis. Atherosclerosis 1995;115(Suppl):S126.
Feuerstein G, Nunnari J, Fisher M, Ruffolo RR Jr. Carvedilol inhibits aortic lipid deposition in the hypercholesterolemic rat model. Pharmacology 1997, in press.
Nichols AJ, Sulpizio AC, Ashton DJ, Hieble JP, Ruffolo RR Jr. In vitro pharmacologic profile of the novel beta-adrenoceptor antagonist and vasodilator, carvedilol. Pharmacology 1989;39:327–336.
Nichols AJ, Sulpizio AC, Ashton DJ, Hieble JP, Ruffolo RR Jr. The interaction of the enantiomers of carvedilol with α1-β1-adrenoceptors. Chirality 1989;1:265–270.
Hieble JP, Naselsky DP, Arch JRS, Chapman H, Smith SA, Ruffolo RR Jr. Affinity of carvedilol for recombinant human adrenoceptors. Pharmacol Commun 1995, in press.
Ruffolo RR, Boyle DA, Brooks DP, Feuerstein GZ, Venuti RP, Lukas MA, Poste G. Carvedilol: A novel cardiovascular drug with multiple actions. Cardiovasc Drug Rev 1992;10:127–157.
DuPont AG, Vander Niepan P, Tallymamsy Y, et al. Effect of carvedilol on ambulatory blood pressure renal hemodynamics and cardiac function in essential hypertension. J Cardiovasc Pharmacol 1987(Suppl 11):S130-S136.
Weber, K., Bohmeke T, van der Does R, Taylor SH. Comparison of the hemodynamic effects of metoprolol and carvedilol in hypertensive patients. Cardiovasc Drugs Ther 1996;10:113–117.
Olsen SL, Gilbert EM, Renlund DG, Mealey PC, Taylor DO, Volkman AK, Bristow MR. Carvedilol improves symptoms and left ventricular function in patients with congestive heart failure due to ischemic or idiopathic dilated cardiomyopathy. J Am Coll Cardiol 1993;21:114A.
Olsen SL, Gilbert EM, Renhend DG, Bristow MR. Carvedilol improves left ventricular function and symptoms in chronic heart failure; a double blind randomized study. J Am Coll Cardiol 1995;25:1225–1231.
Brooks DP, Short BG, Cyronak MJ, Contino LC, DiCristo M, Wang YX, Ruffolo RR Jr. Comparison between carvedilol and captopril in rats with partial ablation-induced chronic renal failure. Br J Pharmacol 1993;109:581–586.
Albrightson, CR, Zabko-Potapovich B, Brooks DP. Effect of carvedilol on mitogen-stimulated mesangial cell proliferation. Pharmacol Communi 1992;1:267–272.
Cruckshank JM, Prichard BNC. Beta-Blockers in Clinical Practice. London: Churchill Livingstone, 1994.
Kendall MJ. Beta Blockade and Cardioprotection. London: Science Press, 1991.
Hansson L. Beta Blockers. London: 1994 Science Press.
Feuerstein GZ, Ruffolo RR Jr. Comparison of the ability of two vasodilating β-blockers, carvedilol and celiprolol, to reduce infarct size in a pig model of acute myocardial infarction. Pharmacol Communi 1994;5:57–63.
Hamburger SA, Barone FC, Feuerstein GZ, Ruffolo RR Jr. Carvedilol (Kredex) reduces infarct size in a canine model of acute myocardial infarction. Pharmacology 1991;43:113–120.
Bril A, Slivjak M, DiMartino J, et al. Cardioprotective effects of carvedilol, a novel β-adrenoceptor antagonist with vasodilating properties, in anaethetised minipigs: Comparison with propranolol. Cardiovasc Res 1992;26:518–525.
Mueller H. Propranolol in acute myocardial infarction in man: Effects of hemodynamics and myocardial oxygenation. Acta Med Scand 1976: 587(Suppl):177–183.
Maroko PR, Kjekshur JK, Sobel BE, et al. Factors influencing infarct size following experimental coronary artery occlusion. Circulation 1971;43:67–82.
Cohn JN. Overview of pathophysiology of clinical heart failure. In: Hosenpund JD, Greenberg BA, eds. Congestive Heart Failure. Springer Verlag, 1994:11–16.
Cohn JN, Rector JS. Prognosis of congestive heart failure and predictors of mortality. Am J Cardiol 1988;62:25A-30A.
Colucci WS. The sympathetic nervous system in congestive heart failure. In: Congestive Heart Failure. Hosenpund JD, Greenberg BH, eds. Springer Verlag, 1994:126–135.
Levine TB, Francis GS, Goldsmith SR, Simon AB, Cohn JN. Activity of the sympathetic nervous system and renin angiotensin system assessed by plasma hormone levels and their relation to hemodynamic abnormalities in congestive heart failure. Am J Cardiol 1982;49:1659–1666.
Mueller HS, Ayres SM. Propranolol decreases sympathetic nervous system activity reflected by plasma catecholamines during evolution of myocardial infarction in man. J Clin Invest 1980;65:338–346.
Opie LH, Thomas M. Propanolol and experimental myocardial infarction: Substrate effects. Postgrad Med 1976;52(Suppl):124–132.
Murray DP, Murray RG, Rafigi E, et al. Beta-adrenergic blockade in acute myocardial infarction: A hemodynamic radionuclide study. Eur Heart J 1987;8:845–854.
Bril A, Tomasi V. Laville MP. Antiarrhythmic effects of carvedilol in rat isolated heart subjected to regional ischemic and reperfusion. Pharmacol Commun 1995, in press.
Brunvald H, Kvitting P, Rynning SE, Berge RK, Grong K. Carvedilol protects against lethal reperfusion injury through antiadrenergic mechanisms. J Cardiovasc Pharmacol 1996;28:409–417.
Fitzgerald JD. By what means might beta-blockers prolong life after acute myocardial infarction? Eur Heart J 1987;8:945–951.
Engler RL, Dahlgren MD, Morris D, et al., Role of leukocytes in the response to acute myocardial ischemia and reflow in dogs. Am J Physiol 1986;251:H314-H323.
Go LO, Murray CE, Richard VJ, et al., Myocardial neutrophil accumulation during reperfusion after reversible or irreversible ischemic injury. Am J Physiol 1988;255:H1188-H1198.
Smith EF, Griswold DE, Egan JW, Hillegass LM, DiMartino MJ. Reduction of myocardial damage and polymorphonuclear leukocyte accumulation following coronary artery occlusion and reperfusion by the thromboxane receptor antagonist, BM 13.505. J Cardiovasc Pharmacol 1989;13:715–722.
Ma X-L, Yue T-L, Lopez BL, et al. Carvedilol, a new β-adrenoreceptor blocker and free radical scavenger, attenuates myocardial ischemia-reperfusion injury in hypercholestrolemic rabbits. J Pharmacol Exp Ther 1995, submitted.
Yue T-L, McKenna PJ, Lysko PG, Gu JL, Lysko KA, Ruffolo RR, Feuerstein GZ. SB 211475, a metabolite of carvedilol, a novel antihypertensive agent, is a potent antioxidant. Euro Jo Pharmacol 1994;251:237–243.
Yue T-L, McKenna PJ, Ruffolo RR Jr, Feuerstein GZ. Carvedilol, a new β-adrenoceptor antagonist and vasodilator antihypertensive drug, inhibits superoxide release from human neutrophils. Eur J Pharmacol 1992;214:277–280.
Yue T-L, Wang X, Gu J-L, Ruffolo RR, Jr, Feuerstein GZ. Carvedilol, a novel vasodilating beta-adrenoceptor antagonist, prevents low-density lipoprotein (LDL)-enhanced leukocyte adhesion to endothelial cells by inhibition of LDL oxidation J Cardiovasc Pharmacol 1995, in press.
Feuerstein GZ, Poste G, Ruffolo RR, Jr, Carvedilol update III: Rationale for use in congestive heart failure. Drugs of Today 1995; 31:307–326.
Yue T-L, Wang X, Gu J-L, Ruffolo RR, Jr, Feuerstein GZ. Carvedilol, a new vasocilating beta-adrenoceptor blocer, inhibits oxidation of low density lipoproteins by vascular smooth muscle cells and prevents leukocyte adhesion to smooth muscle cells. J Pharmacol Exp Ther 1995, in press.
Yue T-L, Cheng HY, Lysko PG, et al. Carvedilol, a new vasodilator and beta adrenoceptor antagonist, is an antioxidant and free radical scavenger. J Pharmacol Exp Ther 1992;263:92–98.
Yue T-L, McKenna PJ, Lysko PG, Ruffolo RR Jr, Feuerstein GZ. Carvedilol, a new antihypertensive, prevents oxidation of human low density lipoprotein by macrophages and copper. Atherosclerosis 1992;97:209–216.
Yue T-L, Liu T, Feuerstein GZ. Carvedilol, a new vasodilator and β-adrenoceptor antagonist, inhibits oxygen-radical-mediated lipid peroxidation in swine ventricular membranes. Pharmacol Communi 1992;1:27–35.
Yue, TL, Lysko PG, Barone FC, Gu JL, Ruffolo RR, Feuerstein G. Carvedilol, a new antihypertensive drug with unique antioxidant activity: Potential role in cerebroprotection. NY Acad Sci 1994;738:230–242.
Cohen MV. Free radicals in ischemic and reperfusion myocardial injury: Is this the time for clinical trials? Ann Intern Med 1989;11:918–931.
Yue T-L, McKenna PJ, Gu JL, Cheng HY, Ruffolo RR, Jr, Feuerstein GZ. Carvedilol, a new antihypertensive agent, prevents lipid perodixation and oxidative injury to endothelial cells. Hypertension 1993;22:922–928.
Yue TL, McKenna J, Gu JL, Cheng HY, Ruffolo RR, Feuerstein GZ. Carvedilol, a new vasodilating β-adrenoceptor blocker antihypertensive drug, protects endothelial cells from damage initiated by xanthine-xanthine oxidase and neutrophils. Cardiovasc Res 1994;28:400–406.
Feuerstein R, Yue T-L. A potent antioxidant, SB 209995, inhibits oxygen-radical-mediated lipid peroxidation and cytotoxicity. Pharmacology 1994;48:385–391.
Christopher TA, Yue T-L, Feuerstein GZ, Ruffolo RR, Jr, Lopez BL, Ma X-L. Carvedilol, a new β-adrenoceptor blocker, vasodilator and free radical scavenger, exerts an anti-shock and endothelial protective effect in rat splanchnic ischemia and reperfusion. J Pharmacol Exp Ther 1995;273:64–71.
Sung C-P, Arleth AJ, Ohlstein EH. Carvedilol inhibits vascular smooth muscle cell proliferation. J Cardiovasc Pharmacol 1993;21:221–227.
Jackson CL, Raines EW, Ross R, Reidy MA. Role of endogenous platelet-derived growth factor in arterial smooth muscle cell migration after balloon catheter injury. Arterioscler Thromb 1993;13:1218–1226.
Schwartz RS, Holmes DR, Topol EJ. The restenosis paradigm revisited: An alternative proposal for cellular mechanisms. J Amer Coll Cardiol 1992;20:1284–1293.
Taylor SH, Silke B. Haemodynamic effects of beta-blockade in ischaemic heart failure. Lancet 1981;2:835–837.
Waagstein F, Hjalmarson A, Varnauskas E, Wallentin I. Effect of chronic beta-adrenergic receptor blockade in congestive cardiomyopathy. Br Heart J 1975;37:1022–1036.
Packer M, Bristwo MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM, Shusterman NH. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. N Engl J Med 1996;334:1349–1355.
Olsen SL, Gilbert EM, Renlund DG, et al. Carvedilol improves left ventricular function in idiopathic dilated cardiomyopathy Circulation 1991;84:11–564.
Olsen SL, Yanowitz FG, Gilbert EM, Mealey PC, Volkman AK, Renlund DG, Bristow MR. β-blocker related improvement in submaximal exercise tolerance in heart failure from idiopathic dilated cardiomyopathy (IDC). J Am Coll Cardiol 1992;19:146A.
Krum H, Gu A, Willshire-Clement M, Miller M, Medina M, Yushola M, Packer M. Changes in plasma levels of endothelin reflect the long term clinical and hemodynamic effects of beta-blockade in patients with chronic heart failure. J Am Coll Cardiol 1994;172A.
Clavell AL, Wright RS, Thomas MR, Brandt RR, Opgenorth TJ, Burnett JC, Elevated endogenous endothelin mediates systemic vasoconstriction in experimental chronic congestive failure. J Am Coll Cardiol 1994;172A.
Ikram H, Fitzpatrick D, Grozier ZG. Therapeutic controversies with use of beta-adrenoceptor blockade in heart failure. Am J Cardiol 1993;71:546–606.
Cohn, JN, Johnson G. Heart failure with normal ejection fraction. The V-HeFT study. Veterans Administration Cooperative Study Group Circulation 1990;81(Suppl III):48–53.
McMurray J, Chopra M, Abdullah I, Smith E, Dargie JH. Evidence of oxidative stress in chronic heart failure in humans. Eur Heart J 1993;14:1493–1498.
Schreck R, Reiber P, Baeccerle PA. Reactive oxygen intermediates as apparently widely used second messengers in the activation of NF-kB transcription factor and HIV-1. EMBO J 1991;10:2247–2258.
Schreck R, Meier B, Mannel D, Droge W, Baeuerle PA. Dithiocarbamates as potent inhibitors of nuclear factor KB activation in intact cells. J Exp Med 1992;175:1181–1194.
Schreck R, Baeuerle PA. A role for oxygen radicals as second messengers. Trends Cell Biol 1991;1:39–44.
Schindler U, Baichwal VR. Three NF-kB binding sites in the human Eselectin gene required for maximal tumor necrosis factor alpha induced expression. Mol Cell Biol 1994;14:5820–5831.
Hockenbery DM, Oltvai ZN, Yin YM, Milliman CL, Kobmeyer SJ. Bcl-2 functions in an antioxidant pathwa to prevent apoptosis. Cell 1993;75:241–151.
Gottlieb RA, Burleson KO, Kloner RA, Babior BM, Engler RL. Reperfusion injury induces apoptosis in rabbit cardiomyocytes. J Clin Invest 1994;94:1621–1628.
Entman ML, Michael L, Rosson RD, Dreyer WJ, Anderson DC, Taylor AA, Smith WC. Inflammation in the course of early myocardial ischemia. FASEB J 1991;5:2529–2537.
Levine B, Kalman J, Mayer L, Fillit HR, Packer M. Elevated circulating levels of tumor necrosis factor in severe chronic heart failure. N Eng J Med 1990;323:236–241.
Hosepund JD, Greenberg BH. Congestive Heart Failure: Pathophysiology, Diagnosis and Comprehensive Approach to Management. Springer Verlag, 1994.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ruffolo, R.R., Feuerstein, G.Z. Pharmacology of Carvedilol: Rationale for Use in Hypertension, Coronary Artery Disease, and Congestive Heart Failure. Cardiovasc Drugs Ther 11 (Suppl 1), 247–256 (1997). https://doi.org/10.1023/A:1007735729121
Issue Date:
DOI: https://doi.org/10.1023/A:1007735729121