Abstract
Purpose
To assess the effect of a 12 week resistance or aerobic training intervention on markers of cardio-metabolic function and sleep among male rotational shift workers.
Method
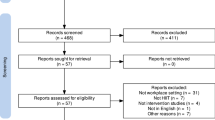
Thirty-eight sedentary, apparently healthy, male rotational shift workers were recruited and randomly allocated to a non-exercise control (CON) group, 3 sessions/week of moderate intensity continuous (MICT), or resistance training (RT) for 12 weeks in a semi-supervised setting. Pre- and post-testing assessed markers of cardio-metabolic function including peak oxygen uptake (VO2peak), glucose metabolism, insulin sensitivity, body composition, inflammatory markers, and 14 day actigraphy sleep assessment.
Results
Mean session attendance across the intervention was 25 (± 7) of a possible 36 sessions. A significant group by time interaction was observed for MICT, with lower c-reactive protein (CRP) values observed post-training (P = 0.049). A significant effect for time was observed for both MICT (n = 9; P = 0.04) and RT (n = 10; P = 0.021), increasing total sleep time (TST) following a night shift post-intervention. Data redistribution regarding exercise adherence: < 24 (N-ADHERE) or ≥ 24 (ADHERE) resulted in significant pre-to-post reduction in body fat (P = 0.024) and fat mass percentage (P = 0.014) among ADHERE. No differences were observed for any intervention group on insulin sensitivity, glucose metabolism or oxygen uptake.
Conclusion
The results of the current study support exercise as a valid intervention to improve the cardio-metabolic health of rotational shift workers. Average sessional attendance suggests shift workers face barriers to exercise that may need to be addressed to improve health outcomes.
Similar content being viewed by others
Introduction
Shift work meets the growing demands of modern society by utilising rotational work periods to extend total labour opportunity [14, 30, 33]. However, the rotational divisions systematically misalign biological rhythms with biological regulators in the external environment [26, 30]. Given the rhythmic and integrated nature of cardiovascular and metabolic regulation, such disruptions may have deleterious effects on function [21, 38]. For example, misaligned circadian and sleep-wake cycles adversely affect insulin sensitivity [23], sleep quality [22] and inflammatory status [23, 31]. While chronic exposure to circadian disruption and poor sleep quality in the form of long-term shift work employment is associated with poor body composition [25] and an increased relative risk of developing cardio-metabolic disorders [14, 30]. With 20% of the global working population involved in shift work [33], intervention strategies targeting improved cardio-metabolic function are vital for employee health.
Exercise is an established intervention method demonstrated to exert wide-ranging improvements in cardio-metabolic function [1, 12, 24]. Exercise is associated with improved sleep quality [14, 21], while, previous research has reported improved cardiopulmonary fitness, inflammatory status and body composition following aerobic exercise [28, 36], and enhanced skeletal muscle mass [28], and glycaemic control [36] following resistance training (RT). The stimulus specific nature of exercise induced adaptations [5] highlight the need for detailed exercise prescription among shift workers to maximise health improvements. However, a lack of shift work specific research [14] means the potential cardio-metabolic effects are yet to be investigated in the context of rotating sleep restriction and circadian disruption. Therefore, exercise may be a viable intervention to improve the cardio-metabolic health of shift workers, however additional research is required to substantiate the hypothesis and identify the most effective mode(s) [14].
In addition to limited research supporting exercise interventions, shift workers report lower levels of physical activity (PA) engagement due to labour specific barriers to exercise [26]. Sleep and social obligations are often prioritised within shift breaks, restricting available time to achieve the PA recommendations [4]. Further, rotational shifts are reported to reduce the motivation to exercise through feelings of residual fatigue [17] and provide exercise opportunities in opposition to team sport or gym facility scheduling [7, 26]. Consequently, developing ecologically valid interventions are important considerations for research conducted among rotational shift workers.
The current study aims to assess the adherence to a semi-supervised exercise training intervention among rotational shift workers. Further, an investigation of the potential effect of aerobic and resistance exercise modalities on cardio-metabolic function, inflammatory markers and sleep will be assessed. It is hypothesised that both training modalities will improve markers of cardio-metabolic function. Further, MICT is hypothesised to be more effective at improving objectively measured sleep, maximal oxygen uptake, body composition and inflammatory status of shift workers.
Methods
Participants
Inclusion criteria required participants to be male, aged 18 years or older, employed in rotational shift work, sedentary (< 60 min planned PA per week), non-smoker with no known cardio-metabolic, sleep or inflammatory disorders. Thirty-eight male rotational shift workers, currently employed in clockwise rotating 8–12 h morning, afternoon, and night shifts, volunteered for this study (baseline data in Table 1). This study was approved by the Institutions Human Ethics Committee, with informed written and verbal consent attained from all participants.
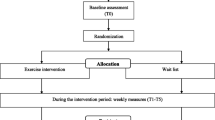
Study Overview
Following recruitment, participants attended a familiarisation session in which procedures and protocols were verbally outlined. Participants then completed baseline testing procedures including anthropometry assessments, maximal graded exercise test (GXT) and objective sleep assessment (actigraphy). Following a 14 day actigraphy and sleep diary assessment, participants returned for a laboratory testing session that included baseline fasted venous blood sampling for assessment of inflammatory markers, an oral glucose tolerance test (OGTT), dual x-ray absorptiometry (DEXA) scan for body composition. Participants were then randomly assigned one of three groups, a non-exercising control (CON; n = 13), moderate-intensity continuous training (MICT; n = 13) or resistance training (RT; n = 12). Upon completion of the 12-week intervention all participants returned for standardised post-intervention testing comprised of the same pre-test procedures.
Exercise Pre-screening and Anthropometry
Participants’ baseline health characteristics were assessed during the familiarisation session via the Adult Pre-exercise Screening Tool (APSS). Anthropometric measures were obtained pre and post training including body mass, recorded wearing minimal clothing, using calibrated electronic scales (A and D HW-PW200, Thebarton, SA, Australia) and height, recorded using a stadiometer in an upright position with head in the Frankfort plane. Waist to hip ratio (WHR) was calculated using waist circumference, measured at the mid-point between the costal arch and the iliac crest; and hip circumference, measured in line with the greater trochanter (steel tape; EC P3 metric graduation, Sydney, NSW, Australia).
Graded Exercise Test (GXT)
All participants completed a ramped maximal graded exercise test (GXT) (Wattbike Trainer, Smeaton Grange, NSW, Australia) conducted with 1 min stages. Fixed resistance was applied to the cycle ergometer with participants required to increase cadence throughout the ramp protocol. An initial power output of 50 W was followed by incremental increase in power output of 25 W/min until volitional exhaustion was achieved. Maximal effort was assessed via an inability to maintain target power output (produced by increasing cycle cadence), combined with RER ≥ 1.1 or HR ± 10 beats of age predicted maximum (220 − Age). Expired gases and flow volumes were collected during the GXT and analysed by a calibrated metabolic cart (TrueOne 2400, ParvoMedics, Salt Lake City, Utah) every 15 s. Peak oxygen uptake (VO2peak) was identified as the mean of the highest two consecutive oxygen consumption values in the final stage of the test.
Actigraphy and Sleep Diaries
Participants were issued a wrist-worn actigraphy watch (Actiware 2, Philips Respironics, Andover, MA, USA) and sleep diary to record subjective bedtime, time of sleep initiation, awake time and the number of awakenings over a 14 day period. Actigraphy was recorded in 30 s epochs and analysed using Actiware v5.70 software (Philips Respironics) in combination with participant sleep diaries recorded during the collection period. Variables obtained from actigraphy software include bedtime, wake time, time in bed (TIB; period between bedtime and get up time), total sleep time (TST; time asleep during TIB), sleep latency (period between bedtime and sleep onset), sleep efficiency (percentage of time in bed spent sleeping), total time awake after sleep onset (WASO), and number of awakenings during total sleep period which were averaged across the collection period. Further calculations were conducted post assessment to obtain the number of awakenings per hour and the percentage of time spent awake after sleep onset. If technical difficulties impacted date collection or the actigraphy device were removed for an extended period within an hour of documented bed or rising time, data of the subsequent sleep period was manually excluded.
Laboratory Testing Session
Following the 14 day actigraphy collection period, participants arrived at the laboratories between 0600 and 0900 h. Participants were instructed to avoid strenuous PA for 24–48 h and caffeine and food for ~ 12 h (fasted) prior to testing. As night shift is associated with acute sleep deprivation and circadian misalignment, testing occurred following either a day off or previous day shift to ensure adequate time for recovery and consistency between all participants. Participants underwent intravenous blood sampling, an OGTT and DEXA scan.
Venous Blood Collection and Analysis
Venous blood was collected to determine baseline inflammatory markers pre- and post-intervention via a 22G catheter (22G BD Medical, North Ryde, NSW, Sydney) inserted into the medial antecubital vein. Samples were collected using ethylenediaminetetraacetic acid (EDTA) with a serine protease inhibitor (Pefabloc SC, Sigma-Aldrich, Sydney, Australia) or serum separator tubes (SST) which was left to clot for ∼20 min before being centrifuged for 10 min at 4 °C and stored at − 80 °C until analysis. Concentrations of IL-6, CRP, TNF-α and insulin were determined using commercially available enzyme-linked immunosorbent assays (ELISA) kit. Serum was analysed for C-reactive protein (CRP) (Human CRP ELISA kit/catalogue No. EK-0040; Crux Biolabs, Scoresby, VIC, Australia), TNF-α (Human TNF-alpha ELISA kit/catalogue No. EK-0001; Crux Biolabs, Scoresby, VIC, Australia) and insulin (Human Insulin ELISA kit/catalogue No. ELH-Insulin-1; Raybiotech, Scoresby, VIC, Australia). Plasma was analysed for IL-6 (Human IL-6 ELISA kit/catalogue No. EK-0012; Crux Biolabs, Scoresby, VIC, Australia). The manufacturer’s specified assay and analytical methods were used throughout. All samples were analysed in duplicate with minimum detectable cytokine levels for each kit: IL-6 (< 5 pg/mL), TNF-α (< 5 pg/mL), CRP (< 0.1 ng/mL) and Insulin (< 4 µIU/mL) respectively. Duplicate readings for each standard, control and sample were averaged and the average zero standard optical density reading was subtracted. A standard curve was created using a 4-parameter logistic curve fit. Concentration values were than determined, using this curve for control and sample average optical densities per the ELISA kit instructions. The Pearson product-moment correlation coefficient (r) was determined by comparing the known standard concentration with the curve fit; r was shown to be greater than 0.98 for all the assays. The homeostasis model for insulin resistance (HOMA-IR) was calculated using the established formula, (fasting insulin [µIU/mL] x fasting glucose [mmol/L]/22.5) [8].
Oral Glucose Tolerance Test
Following an overnight fast of at least 12 h, baseline blood glucose (BGL) levels were obtained via venepuncture, before participants consumed a 75 g oral glucose load dissolved in 300 ml carbonated water (Carbotest, Thermo Fisher Scientific, Australia) within 5 min. BGL was incrementally assessed every 30 min for a total of 120 min post-ingestion via Accu-Chek Performa 2 blood glucose monitoring system (Roche Diagnostics, Castle Hill, NSW, Australia). Testing procedures and blood glucose values were defined in accordance with American Diabetes Association (ADA) and World Health Organisation (WHO) Guidelines [3]. The blood glucose area under the curve (AUC) was calculated using the linear trapezoidal method: ½ (C1 + C2) (T2 – T1) with the initial BGL value acting as a baseline.
Dual-energy x-ray Absorptiometry (DXA)
A supine DXA scan was undertaken to estimate whole-body composition (GE Lunar Prodigy, GE Healthcare, Madison, WI, USA). Participants assumed a supine position on the bench of the DXA machine and a whole-body scan was completed with a resolution of 4.5 × 9.0 mm and scanning speed of 130 mm/s. The scan was then analysed with customized software (Illuminatus DXA, version 4.2.0, Turnbull, CT, USA) for fat mass and fat free mass which are reported in absolute (kg) and relative (%) terms.
Training Intervention
The training intervention was designed to meet the current exercise guidelines described by the World Health Organisation [9]. Participants were required to exercise three days per week for 12 weeks in a semi-supervised setting. Each session was supervised by gym staff with a member of the research team supervising a minimum of one session per week. Both training groups completed a standardised 5 min warm up and cool down during the session. Outlined in Table 1, the program for the moderate-intensity continuous training (MICT) group consisted of 30–40 min of aerobic activity at 60%–75% of maximal heart rate (HRmax). Total session time could be accrued in a minimum of 10 min per aerobic mode including treadmill, stationary bike, or rower with mean sessional watts (W) or speed (km/h) recorded.
The resistance training (RT) group program comprised of two different sessions to be completed alternatively on pin-loaded weight machines targeting the major muscle groups. Session one: chest press, lat pull down, leg press, bicep curl, shoulder press and plank. Session two included chest press, seated row, seated leg extension, seated hamstring curl, triceps extension and plank. Plank involves participants laying in a prone position with the forearm and toes on the ground with core muscle engaged to maintain a stable posture. Participants completed 3 sets of 8–12 repetitions on all weight machine exercises with planks completed in sets of 3, progressing from 30 isometric hold to 60 s per repetition. Progressive overload was provided to participants via increased weight incrementally over the 12 weeks when 12 repetitions were completed for each of the 3 sets. Further, participants progressed from 3 sets per exercise to 4 sets for weeks 7–12. Repetitions and weight were recorded for each exercise in all sessions and used to assess training adaptation. Total session time including dynamic warm up and static stretch cool down was approximately 50 min, which when performed 3 days a week to meet the current PA guidelines [9].
Data Analysis
Statistical analyses were conducted with SPSS software (version 26.0 IBM SPSS, Armonk, NY, USA) and significance set at P < 0.05. The assumption of normality was assessed using the Shapiro-Wilk W test with violations reported. Baseline characteristics (Table 2) were analysed using one-way analysis of variance (ANOVA), with paired samples T test used to investigate pre-to-post performance measures. A repeated within-between ANOVA, with the between factor, group (3 levels) and the within subject factor, time (2 levels) was used to assess training pre-to-post training effect. If a significant group*time interaction was identified, the intervention was deemed to influence response over time and simple main effects of time were evaluated by group using Tukey’s honestly significant difference (Tukey’s HSD). Main effects of time were consulted where group*time interactions did not reach significance, and significant time effects were followed up with Tukey’s HSD. Following statistical analyses data were re-grouped for total sessions attended to assess the effect of exercise adherence (defined as equal to or greater than 2 sessions per week) regardless of training mode, on health outcomes. The same statistical approach was used for the regrouped data. Group data are reported as mean ± standard deviation.
Results
Baseline Descriptive Characteristics
No significant differences were observed between intervention groups at baseline for age, anthropometry, blood pressure (BP) or oxygen uptake [F (2, 35) ≤ 2.248; P ≥ 0.114; Table 2].
Exercise Adherence and Performance Measures
No significant difference was observed in total sessions attendance between the two exercise groups (P > 0.05; Table 3). A significant pre-to-post training increase was observed in sessional workload (kg) for the three major RT exercises (chest press, lat pull down and leg press) (P < 0.05; Table 3). A significant pre-to-post increase was observed in the average sessional workload (W or km/h) for the aerobic exercise modes (treadmill, bike, and rower) (P < 0.05; Table 3).
Actigraphy Sleep Assessment
Due to technical difficulties 11 (4 MICT, 2 RT and 5 CON) post-training actigraphy measures were not recorded and excluded from analysis, resulting in an n = 27. All data were normally distributed except MICT pre intervention for sleep latency (P = 0.001) and post intervention for efficiency (P = 0.001). No significant differences were observed in pre-to-post training intervention for actigraphy variables, including TIB, TST, sleep efficiency, latency, WASO, number of awakenings, number of awakening per hour or time awake after sleep onset (Table 4) (P > 0.05). Sleep variables following a night shift were non-normally distributed for MICT group at pre and post intervention for both latency (P < 0.049) and efficiency (P < 0.05). A significant main effect for time [F (1, 20) = 7.572, P = 0.012, eta squared = 0.275]. Post hoc analysis identified a significant pre-to-post increase in TST for MICT (P = 0.04) and RT (P = 0.02) (Table 4).
Inflammatory Profile and Glucose Metabolism
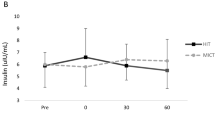
Multiple participants reported metabolite levels below detectable ranges for both TNF-α (n = 30) and IL-6 (n = 23) resulting in the exclusion of analyses for those cytokines. A significant main effect for time was identified [F (1, 27) = 4.233, P = 0.049, eta squared = 0.136] with post hoc analysis revealing a significant effect for MICT to reduce CRP from pre-to-post exercise (P = 0.038; Table 5). No significant difference was observed for insulin (MICT: pre 5.8 ± 2.2, post 5.0 ± 1.6; RT: pre 6.4 ± 3.6, post 6.4 ± 4.3; CON: pre 6.3 ± 2.9, post 6.4 ± 2.1 µIU/mL, P > 0.05). No significant time*group interaction as observed at any time point for the glucose response to an OGTT (Fig. 1) or AUC (MICT: pre 263.2 ± 115.1, post 260.0 ± 224.6; RT: pre 266.0 ± 102.5, post 211.0 ± 164.9; CON: 211.1 ± 121.0, post 270.3 ± 124.6 pg/mL/min). No significant difference was observed pre-to-post intervention for HOMA-IR (P > 0.05; Fig. 2).
Pre-to-post 12 week training response for CRP and insulin resistance (HOMA-IR index). A Pre-to-post CRP values B Pre-to-post insulin resistance as calculated by HOMA-IR C Re-grouped pre-to-post CRP values D Re-grouped Pre-to-post insulin resistance as calculated by HOMA-IR. Pre; pre intervention, post; post intervention. Values are calculated mean ± SD. * denotes significant difference from pre (P <0.05)
Body Composition
A significant main effect for time was observed [F (1, 30) = 7.206, P = 0.012, eta squared = 0.194] for WHR. Post hoc analysis identified a significant increase for the CON group WHR from pre-to-post (P = 0.001). No significant differences were observed for DXA measures of body composition including fat mass, fat free mass and fat mass as a percentage (%) (P > 0.05) (Table 5).
Re-grouped Data Relative to Exercise Adherence
Mean total session attendance for the ≥ 24 sessions (adherence; ADHERE; n = 11) group was 31 ± 4 sessions, while the < 24 sessions (non-adherence; N-ADHERE; n = 14) group was 19 ± 2 sessions. No significant difference was observed in pre-to-post VO2peak for ADHERE and N-ADHERE (ADHERE: pre 32.7 ± 5.6, post 34.6 ± 6.0 mL/kg/min; N-ADHERE: pre 30.9 ± 5.7, post 30.6 ± 5.2 mL/kg/min). A significant group by time interaction was observed for body composition fat mass for ADHERE decreasing from pre (32.9 ± 4.7 kg) to post (30.6 ± 3.6 kg, P = 0.013) while no difference was observed for N-ADHERE (pre 36.7 ± 14.4 and post 37.1 ± 13.6 kg). A significant decrease in BF percentage was observed for ADHERE (pre 33.4% ± 2.9% and post 31.7% ± 3.2%; P = 0.009); and no difference was observed for N-ADHERE (pre 35.3% ± 5.8% and post 35.7% ± 4.7%; P < 0.05). No significant difference was observed for WHR (indexed) ADHERE (pre 0.95 ± 0.06, post 0.96 ± 0.07) and N-ADHERE (pre 0.99 ± 0.9; post 1.0 ± 0.09; P > 0.05). No significant difference was observed for insulin / ADHERE: pre 6.4 ± 3.8, post 5.2 ± 2.3 µIU/mL; N-ADHERE: pre 5.7 ± 1.6, post 6.3 ± 4.0 µIU/mL (P > 0.05) or pre-to-post CRP or HOMA-IR (P > 0.05). No significant difference was observed for glucose response to OGTT (P > 0.05). No significant difference was observed for AUC (ADHERE: pre 254.7 ± 140.6, post 209.6 ± 142.2 pg/mL/min; N-ADHERE: pre 273.3 ± 114.5, post 302.0 ± 177.4 pg/mL/min, P > 0.05).
Discussion
The current project sought to investigate the effect of MICT and RT on sleep and cardio-metabolic function among rotational shift workers. The key observation was 12 weeks of MICT significantly reduced CRP levels from pre-to-post interventions, while both MICT and RT increased TST following a night shift. In contradiction to the research hypothesis, no change was observed in the participants’ average sleep characteristics, maximal oxygen uptake, or glucose metabolism. Results which may be impacted by session attendance, with participants averaging 25 (± 7) total sessions across the 12 weeks. Cumulatively, the findings suggest that the risk of developing cardio-metabolic disorders in apparently healthy male shift works may be reduced by engaging in exercise interventions, but several barriers exist within rotational shift work populations.
Shift work is associated with an increased circulation of CRP [31], a biomarker of systemic inflammation and strong univariate predictor of future adverse cardio-metabolic outcomes [31]. A 12-week MICT program significantly reduced CRP levels and may reduce the relative risk of future cardio-metabolic disorders. Conversely, RT did not influence CRP levels, and with no significant difference in group exercise adherence, the results suggest MICT may be a more effective exercise mode to improve inflammatory status among shift workers. A plausible explanation may be the differences in mode-based oxidative adaptations between exercise groups. Endurance exercise is associated with enhanced muscle metabolism, specifically increased oxidative capacity due to mitochondrial biogenesis [18]. Consequently, MICT may have improved skeletal oxidative capacity and reduced a potential stimulant for CRP production [2]. Alternatively, chronic training may have upregulated anti-inflammatory mediators including IL-6, capable of inhibiting the pro-inflammatory cascade and reducing systemic inflammatory markers [11]. Unfortunately, as the supplementary inflammatory markers (TNF-α and IL-6) were below detectable ranges within the current project, interpretations of potential mechanisms responsible for the divergent training adaptations are limited and require further elucidation.
Cardio-metabolic function is additionally moderated by sleep-wake cycles and poor sleep, particularly reduced TST, is hypothesised to facilitate pathogenesis [20]. Employment in rotational shift work is associated with reductions in sleep quality [27], with night shift demonstrated to reduce TST of the subsequent sleep opportunity [13]. The MICT and RT intervention significantly increased post nightshift TST by 31 and 35 min respectively. No significant differences were observed in supplementary actigraphy measures or values averaged over the collection period (Table 4). Actigraphy and sleep diary assessment was averaged over a 14-day period, including days on, off and different shift rotations such as night shift. Consequently, strategies including naps or extended sleep on days off may mask the differences in acute sleep bouts, or acute improvements in sleep quality induced by exercise training [37]. Further, the presence of undiagnosed sleep disorders including obstructive sleep apnea may have impacted sleep assessment among participants. Screening for diagnosed sleep disorders were conducted by subjective health questionnaires, however given the inactive and overweight status of participants, undiagnosed disorders may have been present [34]. Further research incorporating polysomnography assessment of sleep quality is required to support and explore the current observation.
Despite exercise interventions eliciting a range of health benefits [36], no significant improvements were observed in body composition, oxygen uptake or glucose metabolism post-intervention. Exercise-based adaptations are specific to the exercise stimulus and total dose [5] with the reduced adherence observed in the current study likely resulting in an insufficient stimulus to significantly improve body composition, oxygen uptake and glucose metabolism within the 12-week period. Shift work-specific restrictions may have contributed to reduced exercise adherence within the current project, alternatively, the sessional attendance may reflect current trends of non-adherence among the general population [10]. Re-distribution of interventions groups based on sessional attendance rather that training modality resulted in observable changes in body composition. A significant decrease in body fat (–2.3 ± 3.2 kg) and body fat percentage (–1.7% ± 2.0%) is reported within the ADHERE group who averaged 31 of a prescribed 36 session. Increased adiposity is classified as a risk factor for the development of cardio-metabolic disorders [29] with hypertrophic adipocytes undergoing molecular and cellular alterations, secreting pro-inflammatory mediators and decreasing insulin sensitivity [6, 15, 16]. Consequently, the reduction in adipose tissue induced by higher exercise adherence may reduce the associated relative risk of developing cardio-metabolic disorders [6, 35] among shift workers.
A mechanistic link underlying the association of obesity with cardio-metabolic conditions, is the observed effect of adipose tissue and inflammation on decreasing insulin sensitivity [6, 16]. However, neither the normal or re-distributed data demonstrated a significant effect on the on glucose metabolism. Results which may be explained by the pre-intervention screening process excluding participants with diagnosed cardio-metabolic disorders. Resultantly, the mean baseline variables were within healthy ranges and potentially created a ceiling effect with minimal room for improvement. Further, the reduced exercise adherence may be a limitation in interpreting the current observations. Previous interventions, conducted with similar methodology among comparable participants have resulted in significant changes in body composition, fasting glucose and HOMA-IR [19, 32]. However the protocols prescribed increased intensity and volume in comparison to the current project, and participants reported higher adherence rates, completing 94% of exercise sessions [32]. A final limitation of note is the exclusive recruitment of male rotational shift workers. The approach to recruitment does not allow the application of results to fixed shift or female employees. Additional research is required to replicate results among a wider population group more reflective of shift work as a whole.
Cumulatively, exercise presents as a viable intervention method to improve cardio-metabolic health among male shift workers. Aerobic interventions appear to be a more effective mode, eliciting improvements in both inflammatory status and TST following night shift. The current research project attempted to increase exercise adherence via providing a semi-autonomous (regarding cardio mode), structured and flexible training intervention. However, the mean session attendance indicate that more research is required to facilitate shift work exercise intervention to increase exercise adherence and thus gain potential anthropometric and physiological improvements.
Data Availability
Data will be made available upon reasonable request.
References
Abd El-Kader SM. Aerobic versus resistance exercise training in modulation of insulin resistance, adipocytokines and inflammatory cytokine levels in obese type 2 diabetic patients. J Adv Res. 2011;2(2):179–83.
Abramson JL, Hooper WC, Jones DP, Ashfaqc S, Rhodes SD, Weintraub WS, Harrison DG, Quyyumi AA, Vaccarino V. Association between novel oxidative stress markers and C-reactive protein among adults without clinical coronary heart disease. Atherosclerosis. 2005;178(1):115–21.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Supplement 1):S62–9.
Atkinson G, Fullick S, Grindey C, Maclaren D. Exercise, energy balance and the shift worker. Sports Med. 2008;38(8):671–85.
Baar K. The signaling underlying FITness applied physiology. Nutr Metabolism. 2009;34(3):411–9.
Berg AH, Scherer PE. Adipose tissue, inflammation, and cardiovascular disease. Circul Res. 2005;96(9):939–49.
Blake H, Stanulewicz N, Mcgill F. Predictors of physical activity and barriers to exercise in nursing and medical students. J Adv Nurs. 2017;73(4):917–29.
Bonora E, Formentini G, Calcaterra F, Lombardi S, Marini F, Zenari L, Raffaelli A. HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in type 2 diabetic subjects: prospective data from the verona diabetes complications study. Diabetes Care. 2002;25(7):1135–41.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, Carty C, Chaput JP, Chastin S, Chou R, Dempsey PC, DiPietro L, Ekelund U, Firth J, Friedenreich CM, Garcia L, Gichu M, Jago R, Katzmarzyk PT, Lambert E, Leitzmann M, Milton K, Ortega FB, Ranasinghe C, Stamatakis E, Tiedemann A, Troiano RP, van der Ploeg HP, Wari V, Willumsen JF. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62.
Burnet K, Higgins S, Kelsch E, Moore JB, Stoner L. The effects of manipulation of frequency, intensity, time, and type (FITT) on exercise adherence: a meta-analysis. Translational Sports Medicine. 2020;3(3):222–34.
Del Giudice M, Gangestad SW. Rethinking IL-6 and CRP: Why they are more than inflammatory biomarkers, and why it matters. Brain Behav Immun. 2018;70:61–75.
Donges C, Duffield R, Drinkwater E. Effect of resistance or aerobic exercise training on interleukin-6, C-reactive protein, and body. Med Sci Sports Exerc. 2010;42(2):304–13.
Ferguson B, Shoff H, Shreffler J, McGowan J, Huecker M. Does my emergency department doctor sleep? The trouble with recovery from night shift. J Emerg Med. 2019;57(2):162–7.
Flahr H, Brown WJ, Kolbe-Alexander TL. A systematic review of physical activity-based interventions in shift workers. Prev Med Rep. 2018;10:323–31.
Golbidi S, Mesdaghinia A, Laher I. Exercise in the metabolic syndrome. Oxid Med & Cellu Longev. 2012;1–13. https://doi.org/10.1155/2012/349710.
Greenberg AS, Obin MS. Obesity and the role of adipose tissue in inflammation and metabolism. Am J Clin Nutr. 2006;83(2):461S–465S.
Hargens TA, Kaleth AS, Edwards ES, Butner KL. Association between sleep disorders, obesity, and exercise: a review. Nat Sci sleep. 2013;5:27.
Hood DA. Mechanisms of exercise-induced mitochondrial biogenesis in skeletal muscle. Appl Physiol Nutr Metab. 2009;34(3):465–72.
Jorge MLMP, de Oliveira VN, Resende NM, Paraiso LF, Calixto A, Diniz ALD, Resende ES, Ropelle ER, Carvalheira JB, Espindola FS, Jorge PT, Geloneze B. The effects of aerobic, resistance, and combined exercise on metabolic control, inflammatory markers, adipocytokines, and muscle insulin signaling in patients with type 2 diabetes mellitus. Metabolism. 2011;60(9):1244–52.
Kecklund G, Axelsson J. Health consequences of shift work and insufficient sleep. BMJ. 2016;355:i5210. https://doi.org/10.1136/bmj.i5210.
Kervezee L, Kosmadopoulos A, Boivin DB. Metabolic and cardiovascular consequences of shift work: the role of circadian disruption and sleep disturbances. Eur J Neurosci. 2020;51(1):396–412.
Korsiak J, Tranmer J, Day A, Aronson KJ. Sleep duration as a mediator between an alternating day and night shift work schedule and metabolic syndrome among female hospital employees. Occup Environ Med. 2018;75(2):132–8.
Leproult R, Holmbäck U, Van Cauter E. Circadian misalignment augments markers of insulin resistance and inflammation, independently of sleep loss. Diabetes. 2014;63(6):1860–9.
Lim S-T, Min S-K, Kwon Y-C, Park S-K, Park H. Effects of intermittent exercise on biomarkers of cardiovascular risk in night shift workers. Atherosclerosis. 2015;242(1):186–90.
Liu Q, Shi J, Duan P, Liu B, Li T, Wang C, Li H, Yang T, Gan Y, Wang X, Cao S, Lu Z. Is shift work associated with a higher risk of overweight or obesity? A systematic review of observational studies with meta-analysis. Int J Epidemiol. 2018;47(6):1956–71.
Nea FM, Pourshahidi LK, Kearney J, Livingstone MBE, Bassul C, Corish CA. A qualitative exploration of the shift work experience: the perceived barriers and facilitators to a healthier lifestyle and the role of the workplace environment. J Occup Environ Med. 2017;59(12):1153–60.
Niu S-F, Chung M-H, Chen C-H, Hegney D, O’Brien A, Chou K-R. The effect of shift rotation on employee cortisol profile, sleep quality, fatigue, and attention level: a systematic review. J Nurs Res. 2011;19(1):68–81.
Park W, Jung W-S, Hong K, Kim Y-Y, Kim S-W, Park H-Y. Effects of moderate combined resistance-and aerobic-exercise for 12 weeks on body composition, cardiometabolic risk factors, blood pressure, arterial stiffness, and physical functions, among obese older men: a pilot study. Int J Environ Res Public Health. 2020;17(19):7233.
Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, Eckel RH. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113(6):898–918.
Puttonen S, Härmä M, Hublin C. Shift work and cardiovascular disease—pathways from circadian stress to morbidity. Scand J Work Environ Health. 2010;36(2):96–108.
Puttonen S, Viitasalo K, Härmä M. Effect of shiftwork on systemic markers of inflammation. Chronobiol Int. 2011;28(6):528–35.
Saremi A, Asghari M, Ghorbani A. Effects of aerobic training on serum omentin-1 and cardiometabolic risk factors in overweight and obese men. J Sports Sci. 2010;28(9):993–8.
Schilperoort M, Rensen PC, Kooijman S. Time for novel strategies to mitigate cardiometabolic risk in shift workers. Trends Endocrinol Metab. 2020;31(12):952–64.
Smith SS, Doyle G, Pascoe T, Douglas JA, Jorgensen G. Intention to exercise in patients with obstructive sleep apnea. J Clin Sleep Med. 2007;3(7):689–94.
Wallberg-Henriksson H, Zierath JR. Exercise remodels subcutaneous fat tissue and improves metabolism. Nat Reviews Endocrinol. 2015;11(4):198–200.
Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. Can Med Assoc J. 2006;174(6):801–9.
Wickwire EM, Geiger-Brown J, Scharf SM, Drake CL. Shift work and shift work sleep disorder: clinical and organizational perspectives. Chest. 2017;151(5):1156–72.
Zimmet P, Alberti K, Stern N, Bilu C, El-Osta A, Einat H, Kronfeld‐Schor N. The Circadian syndrome: is the metabolic syndrome and much more! J Intern Med. 2019;286(2):181–91.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This study was funded solely by the Australian Government Research Training Program.
Author information
Authors and Affiliations
Contributions
Review and editing (equal). BC: conceptualisation (lead); writing – original draft (lead); formal analysis (lead): supervision (lead). TH: conceptualisation. FM: conceptualisation. MS; conceptualisation; supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors have not disclosed any competing interests.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent to Publish
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Collins, B.E.G., Hartmann, T.E., Marino, F.E. et al. The Effect of a 12 Week Mixed-Modality Training Intervention on the Cardio-Metabolic Health of Rotational Shift Workers. J. of SCI. IN SPORT AND EXERCISE (2022). https://doi.org/10.1007/s42978-022-00207-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s42978-022-00207-8