Abstract
Introduction
Data on triple therapy (long-acting muscarinic antagonist [LAMA] + inhaled corticosteroid/long-acting beta2-agonist [ICS/LABA]) in symptomatic patients with chronic obstructive pulmonary disease (COPD) are limited. This post hoc analysis aimed to determine the efficacy of once-daily umeclidinium (UMEC; 62.5 μg) or placebo (PBO) plus open-label fixed-dose ICS/LABA in symptomatic patients with COPD.
Methods
Data were pooled from four randomized, double-blind, parallel-group trials (ClincalTrials.gov identifiers: NCT01772134, NCT01772147, NCT01957163, NCT02119286). Inclusion criteria included COPD diagnosis, modified Medical Research Council dyspnea scale score ≥2 and forced expiratory volume in 1 s (FEV1) <70% predicted. Following a 4-week run-in with once-daily or twice-daily ICS/LABA, patients were randomized to UMEC 62.5 μg or PBO as add-on therapy for 12 weeks. The efficacy of UMEC 62.5 μg + ICS/LABA or PBO + ICS/LABA in the intent-to-treat (ITT) population and subgroups with Global initiative for chronic Obstructive Lung Disease (GOLD) B and D COPD, and once-daily or twice-daily ICS/LABA was investigated. Outcomes included: trough FEV1, rescue-medication use, St George’s Respiratory Questionnaire (SGRQ) score, moderate/severe exacerbations. Adverse events (AEs) were assessed.
Results
UMEC 62.5 μg + ICS/LABA (ITT: n = 819) provided clinically important improvements in trough FEV1 versus PBO + ICS/LABA [ITT: n = 818; 130 mL (95% CI 112, 147); P < 0.001] at Day 85. Similar improvements occurred in all four subgroups (119–147 mL; all P < 0.001). In the ITT population, UMEC 62.5 μg + ICS/LABA decreased rescue-medication use, improved SGRQ score, and reduced short-term exacerbation risk (all P ≤ 0.004 versus PBO + ICS/LABA). These three outcomes also improved consistently with UMEC 62.5 μg + ICS/LABA versus PBO + ICS/LABA with both ICS/LABAs and in the GOLD D subgroup. In the GOLD B subgroup a statistically significant benefit was observed in lung function and proportion of SGRQ responders. AE incidences were similar with UMEC 62.5 μg + ICS/LABA versus PBO + ICS/LABA.
Conclusion
In symptomatic patients with COPD, triple therapy with UMEC 62.5 μg + ICS/LABA improved lung function, reduced rescue-medication use, improved health-status and reduced exacerbation risk versus PBO + ICS/LABA, with similar safety profiles.
Funding
GSK (study number 202067).
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by persistent airflow obstruction and is a major contributor to global morbidity and mortality [1]. Bronchodilators [e.g., long-acting beta2 agonists (LABAs) and long-acting muscarinic antagonists (LAMAs)] are central to the pharmacological management of symptomatic COPD [1]. However, use of bronchodilator monotherapy is frequently associated with ongoing dyspnea [2]. Combining two bronchodilators with different mechanisms of action could increase bronchodilation with equivalent or fewer side effects compared with increasing the dose of a single agent [1]. A common stepwise treatment approach to attain dual bronchodilation is to co-administer LAMA and inhaled corticosteroid (ICS)/LABA as triple therapy [3, 4]. Retrospective large UK database studies have suggested that this triple regimen is associated with reductions in exacerbations and all-cause mortality compared with ICS/LABA alone [3, 5]. However, the efficacy and safety of adding a LAMA to ICS/LABA has been tested in a limited number of randomized, double-blind clinical trials, and therefore further investigation is warranted [6, 7].
Umeclidinium bromide 62.5 μg (UMEC, GSK573719; GSK, London, UK) is a once-daily LAMA indicated for the maintenance treatment of patients with symptomatic COPD [8, 9]. Four studies have examined the efficacy of UMEC added to once- or twice-daily ICS/LABA therapy, all of which demonstrated that UMEC (62.5 or 125 μg) + ICS/LABA improved trough forced expiratory volume in 1 s (FEV1) compared with placebo (PBO) + ICS/LABA [10, 11]. These individual studies were not powered to detect treatment differences on patient-reported outcomes (PROs) and individual studies failed to demonstrate consistent benefits on PROs [10, 11]. Consequently, an integrated analysis was designed, pooling the data from all four studies to examine PROs in greater detail and to also facilitate subgroup analysis.
Guidelines suggest patients with COPD can be categorized into one of four Global initiative for chronic Obstructive Lung Disease (GOLD) patient groups (A–D) and recommend that therapy should be prescribed accordingly [1]. As patients in GOLD groups A and C present with a lower symptom burden than those in groups B and D [1], groups A and C were excluded from all four clinical trials examining triple therapy included in this post hoc analysis [10, 11]. Specifically, patients in GOLD group B and D had moderate-to-severe dyspnea [1]. Additionally, GOLD B included patients with moderate airflow limitation (FEV1 ≥50% predicted) and a low future risk of exacerbations, whereas GOLD D included patients with severe-to-very-severe airflow limitation (FEV1 <50% predicted) and a high future risk of exacerbations [1].
When prescribing a LAMA added to ICS/LABA, physicians choose the LAMA and ICS/LABA combination they consider most likely to benefit their patients [1]. However, there is little information in the published literature on whether the specific type and/or posology of the ICS/LABA combination, for example, once- or twice-daily dosing, influences the incremental effect of LAMA add-on therapy as a component of open triple therapy.
The aim of this post hoc analysis was therefore to determine the robustness of the efficacy and safety of once-daily UMEC (62.5 μg) + fixed-dose ICS/LABA compared with PBO + fixed-dose ICS/LABA in symptomatic patients with COPD by pooling data from four similarly-designed clinical trials.
Methods
This article is based on previously conducted, individually reported clinical trials [10, 11], and did not involve any new clinical trials performed by any of the authors or any new primary data relating to patients from any other source.
This was a post hoc analysis of four 12-week, Phase III, multicenter, randomized, double-blind, parallel-group trials comparing once-daily inhaled UMEC 62.5 μg (delivering 55 μg) + ICS/LABA with PBO + ICS/LABA. Two trials assessed UMEC 62.5 μg + fluticasone propionate/salmeterol (FP/SAL; 250/50 μg twice daily; ClinicalTrials.gov identifiers: NCT01772134 [AC4116135] and NCT01772147 [AC4116136] [10]) and two trials assessed UMEC 62.5 μg + fluticasone furoate/vilanterol (FF/VI; 100/25 μg once daily; delivering 92/22 μg; ClinicalTrials.gov identifiers: NCT01957163 [200109] and NCT02119286 [200110] [11]). All four trials also investigated the add-on benefits of a higher unlicensed dose of once-daily UMEC 125 μg + ICS/LABA, but only the results from the approved dose of UMEC 62.5 μg + ICS/LABA are presented here. It has previously been shown that both UMEC 62.5 and 125 μg doses had similar efficacy and safety profiles when added to ICS/LABA combination therapy in all of the original studies [10, 11].
Key inclusion criteria of all studies included a diagnosis of COPD (predicted post-bronchodilator FEV1 <70% and FEV1/forced vital capacity <0.70), with a modified Medical Research Council dyspnea scale score ≥2 (i.e., all classified as GOLD B or GOLD D) [10, 11]. Patients with GOLD D COPD also had FEV1 <50% predicted or ≥2 exacerbations (or ≥1 COPD-related hospitalization) in the 12 months prior to enrollment.
All four studies had a similar treatment design. Enrolled patients entered a 4-week open-label run-in treatment period with once- or twice-daily ICS/LABA. At the end of this period, patients without a COPD exacerbation, who did not use any of the prohibited medications and who were 80–120% compliant with the study drug were randomized to receive UMEC or PBO added to the same ICS/LABA treatment for 12 weeks. Further details of the trial designs have been previously published [10, 11].
Post Hoc Analysis
The primary endpoint for the four studies and the first endpoint examined in this post hoc analysis was trough FEV1 on Day 85, defined as the mean of the FEV1 values obtained 23 and 24 h after dosing on Day 84 in the intent-to-treat (ITT) population. The ITT population was defined as all patients who were randomized and received at least one dose of study drug.
Other assessed efficacy endpoints included: the proportion of patients achieving an increase in trough FEV1 above baseline (Day 1) of ≥100 mL on Day 85, serial FEV1 post-dose on Days 1 and 84, weighted mean (WM) FEV1 over 0–6 h post-dose at Day 84, rescue salbutamol/albuterol use (puffs/day, % rescue-free days), total St George’s Respiratory Questionnaire (SGRQ) score, and the proportion of patients with a SGRQ response (defined as an improvement of ≥4 units from baseline) on Day 84. The incidence of COPD exacerbations was assessed as a safety endpoint in the original studies. A moderate/severe COPD exacerbation, for the purpose of this analysis, was defined as any acute worsening of COPD symptoms requiring the use of any antibiotics, systemic corticosteroids, emergency treatment or hospitalization.
In this post hoc analysis, these endpoints were examined in the ITT population and by subgroup: GOLD B status, GOLD D status, once-daily FF/VI treatment (studies 200109 and 200110) and twice-daily FP/SAL treatment (studies AC4116135 and AC4116135).
AEs and serious AEs (SAEs) after the run-in period were assessed across all studies and are reported here only for the full pooled ITT population. AEs of special interest included those associated with antimuscarinic agents such as UMEC.
Statistical Analyses
Trough FEV1, 0–6 h WM FEV1, and SGRQ total score analyses were performed using a repeated measures model with covariates of study, treatment, baseline measurement, smoking status, Day, Day by baseline, and Day by treatment interactions. Rescue-medication use (percentage of rescue-free days over the study duration and mean number of puffs per day) was analyzed using an analysis of covariance (ANCOVA) model with covariates of study, treatment, smoking status and baseline measurement. The proportion of patients achieving an increase in trough FEV1 above baseline of ≥100 mL on Day 85 and an SGRQ response were analyzed using logistic regression with covariates of study, treatment, baseline measurement and smoking status. Kaplan–Meier plots were used to plot the time to first on-treatment COPD exacerbation. Cox proportional hazard models with covariates of study, treatment and smoking status at screening were used to calculate the hazard ratios (HR) and 95% confidence intervals (CIs) associated with the time to first exacerbation. All statistical analyses were performed using SAS Version 9 (SAS Institute Inc., Cary, NC, USA).
Results
Baseline Characteristics
A total of 3191 patients were recruited to these four studies, with data from 2458 patients in the ITT population included in these post hoc analyses (1637 patients received UMEC 62.5 μg + ICS/LABA or PBO + ICS/LABA; Fig. 1). Patient demographics and baseline characteristics were similar across the two treatment groups (Table 1). In the subgroups analyzed, the number of patients with GOLD B COPD was 320 and 344, and with GOLD D COPD was 499 and 474 (UMEC 62.5 μg + ICS/LABA and PBO + ICS/LABA, respectively; Table 1). There were 96% and 98% of patients within the GOLD D subgroups that had severe airflow limitation (FEV1 <50% predicted; UMEC 62.5 μg + ICS/LABA and PBO + ICS/LABA, respectively), while 24% in each group had experienced one or more COPD exacerbations in the year prior to enrollment (Table 1).
Summary of patient disposition within the pooled analysis. (Asterisk) Only the results relating to the approved dose UMEC 62.5 μg are presented in this paper. The efficacy and safety outcomes of this investigational dose have been previously published [10, 11]. FEV 1 forced expiratory volume in 1 s, FF/VI fluticasone furoate/vilanterol, FP/SAL fluticasone propionate/salmeterol, ICS inhaled corticosteroid, LABA long-acting beta2 agonist, PBO placebo, UMEC umeclidinium
Efficacy
Lung Function
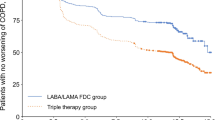
Changes from baseline in trough FEV1 at Day 85 showed clinically important (≥100 mL) and statistically significant improvements for UMEC 62.5 μg + ICS/LABA versus PBO + ICS/LABA in the ITT population (130 mL; 95% CI 112, 147; P < 0.001; Table 2; Fig. 2a). Clinically important, observed mean improvements in FEV1 were seen with UMEC 62.5 μg + ICS/LABA versus PBO + ICS/LABA from 3 h after the first dose of triple therapy (Fig. 2b). Patients were more likely to achieve a clinically important increase in trough FEV1 from baseline at Day 85 with UMEC 62.5 μg + ICS/LABA versus PBO + ICS/LABA (46% vs. 15%; odds ratio 4.9; 95% CI 3.9, 6.3; P < 0.001; Table 2). For the 0–6 h WM FEV1 at Day 84, UMEC 62.5 μg + ICS/LABA provided statistically significant improvements of 152 mL versus PBO + ICS/LABA (95% CI 134, 170; P < 0.001; Table 2).
Change from baseline in trough FEV1 at Day 85 (a; ITT population), first and last dose treatment differences (UMEC 62.5 μg ICS/LABA versus PBO + ICS/LABA) in 24-h serial FEV1 (b; ITT population). CI confidence interval, FEV 1 forced expiratory volume in 1 s, ICS inhaled corticosteroid, ITT intent-to-treat, LABA long-acting beta2 agonist, LS least squares, MCID minimal clinically important difference (defined as ≥100 mL: change from baseline in a and treatment difference in b), PBO placebo, UMEC umeclidinium
When analyzed by GOLD B/D subgroup, clinically important and statistically significant improvements in trough FEV1 from baseline at Day 85 were achieved with UMEC 62.5 μg + ICS/LABA versus PBO + ICS/LABA in both subgroups (GOLD B: 147 mL, 95% CI 118, 175; GOLD D: 119 mL, 95% CI 98, 141; both P < 0.001; Table 3). The 24-h serial FEV1 treatment differences were greater at Days 84–85 versus Days 1–2 in both GOLD subgroups and appeared to be greater in the GOLD B population (Fig. 3a, b).
First and last dose treatment differences (UMEC 62.5 μg ICS/LABA versus PBO + ICS/LABA) in 24-h serial FEV1 by the GOLD patient subgroup B (a), subgroup D (b), and by ICS/LABA combination FF/VI (c) and FP/SAL (d). CI confidence interval, FEV 1 forced expiratory volume in 1 s, GOLD Global initiative for chronic Obstructive Lung Disease, ICS inhaled corticosteroid, LABA long-acting beta2 agonist, LS least squares, MCID minimal clinically important difference (defined as a ≥100 mL treatment difference), PBO placebo, UMEC umeclidinium
When analyzing lung function by ICS/LABA combination, UMEC 62.5 μg added to FF/VI statistically improved trough FEV1 from baseline at Day 85 versus PBO + FF/VI (122 mL, 95% CI 101, 144; P < 0.001), with similar results obtained for UMEC 62.5 μg + FP/SAL versus PBO + FP/SAL (137 mL, 95% CI 110, 164; P < 0.001; Table 3). The likelihood of patients in the UMEC 62.5 μg + FF/VI treatment arm achieving an increase of ≥100 mL in trough FEV1 at Day 85 versus PBO + FF/VI was statistically significant, as was the likelihood in UMEC 62.5 μg + FP/SAL versus PBO + FP/SAL (both P < 0.001; Table 3). The magnitude of these treatment differences appeared similar (Table 3). The sustained 24-h efficacy versus PBO + ICS/LABA, as assessed via serial FEV1, appeared similar in patients receiving either ICS/LABA treatment in combination with UMEC 62.5 μg (Fig. 3c, d).
Patient-Reported Outcomes
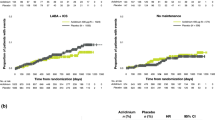
Improvements in rescue-medication use (mean puffs/day and % rescue-free days; weeks 1–12), as well as SGRQ total score and SGRQ responders (at Day 84) were seen with UMEC 62.5 μg + ICS/LABA versus PBO + ICS/LABA in the ITT population (Table 2). The SGRQ improvement of −1.55 units was statistically significant (95% CI −2.51, −0.59; P = 0.002) and was achieved in addition to ICS/LABA change from baseline benefits in SGRQ. Fewer patients experienced a COPD-related exacerbation with UMEC 62.5 μg + ICS/LABA (n = 31, 4%) versus PBO + ICS/LABA (n = 57, 7%). Treatment with UMEC 62.5 μg + ICS/LABA resulted in a 47% risk reduction of a first exacerbation versus PBO + ICS/LABA (HR 0.53; 95% CI 0.34, 0.82; P = 0.004; Fig. 4a).
Time to first exacerbation in the ITT population (Kaplan–Meier plot, a) and the hazard ratios of this event in the ITT population and each subgroup (b). CI confidence interval, FF/VI fluticasone furoate/vilanterol, FP/SAL fluticasone propionate/salmeterol, GOLD Global initiative for chronic Obstructive Lung Disease, ICS inhaled corticosteroid, ITT intent-to-treat, LABA long-acting beta2 agonist, LS least squares, PBO placebo, UMEC umeclidinium
UMEC 62.5 μg + ICS/LABA statistically improved rescue-medication use, change from baseline in SGRQ total score and the proportion of SGRQ responders versus PBO + ICS/LABA in the GOLD D subgroup (Table 3). Although there was a trend for improvements in PROs in the GOLD B subgroup, only the proportion of SGRQ responders with UMEC 62.5 μg + ICS/LABA was statistically significant versus PBO + ICS/LABA (Table 3). Only patients in GOLD D showed a statistically significant reduction in the risk of a first exacerbation with UMEC 62.5 μg + ICS/LABA (23 patients with an exacerbation; 5%) versus PBO + ICS/LABA (39 patients with an exacerbation; 8%; reduction of 49%; HR 0.51; 95% CI 0.30, 0.86; P = 0.012; Fig. 4b). The magnitude of effect seen in the GOLD B subgroup was similar to that in the GOLD D subgroup, with an apparent risk reduction of 56% for a first exacerbation with UMEC 62.5 μg + ICS/LABA (8 patients with an exacerbation; 3%) versus PBO + ICS/LABA (18 patients with an exacerbation; 5%), but this difference failed to reach statistical significance (HR 0.44; 95% CI 0.19, 1.02; P = 0.055; Fig. 4b).
UMEC 62.5 μg added to either FF/VI or FP/SAL resulted in similar improvements in rescue-medication use and SGRQ scores (Table 3). Each of these improvements were statistically significant versus PBO + ICS/LABA (all P < 0.05; Table 3). A total of 12 patients (3%) treated with UMEC 62.5 μg + FF/VI experienced a moderate/severe exacerbation versus 24 patients (6%) treated with PBO + FF/VI (HR 0.47; 95% CI 0.23, 0.94; P = 0.033). There appeared to be a reduction in the risk of COPD exacerbations for patients treated with UMEC 62.5 μg + FP/SAL (19 patients with an exacerbation; 5%) compared with PBO + FP/SAL (33 patients with an exacerbation; 8%); however, this was not statistically significant (HR 0.58; 95% CI 0.33, 1.02; P = 0.058; Fig. 4b).
Safety
The overall incidence of AEs was similar across treatment groups, with nasopharyngitis, headache and back pain the most commonly reported AEs (Table 4). The incidences of AEs of special interest (which included pneumonia, lower respiratory tract infection and cardiovascular events) were similar or lower in the UMEC 62.5 μg + ICS/LABA versus PBO + ICS/LABA groups.
A total of eight fatal SAEs were reported in these two treatment arms, none of which was considered related to the study treatment. Two deaths occurred in the UMEC 62.5 μg + ICS/LABA group (one due to gastric ulcer hemorrhage with myocardial infarction and one to lymphoma). There were six deaths in the PBO + ICS/LABA group (three due to myocardial infarctions, one to cardio-respiratory arrest, one to cardiac arrest and one to pneumonia). Further details on these events have been previously published [10, 11].
Discussion
In this pooled analysis of four replicated 12-week lung-function studies performed in patients with symptomatic COPD, UMEC 62.5 μg added to a background of open-label ICS/LABA treatment resulted in clinically important improvements in trough FEV1 (≥100 mL) versus PBO + ICS/LABA in the ITT population and all subgroups. Improvements in serial FEV1 were evident 15 min after the first dose of UMEC 62.5 μg + ICS/LABA, and by 3 h a mean increase of ≥100 mL from PBO + ICS/LABA was achieved. This level of improvement was maintained to the last study dose in all four study subgroups. In the overall ITT population, UMEC 62.5 μg + ICS/LABA improved all PROs including daily rescue medication use (a marker of a patient’s daily symptomatology) and health-related quality of life, as well as reducing the risk of a first moderate/severe COPD exacerbation versus PBO + ICS/LABA. This study therefore demonstrates that a stepwise increase to triple therapy may be beneficial for many patients with symptomatic COPD receiving ICS/LABA therapy.
A surprising finding of this pooled post hoc analysis was that the magnitude of improvements in lung function were remarkably consistent in all subgroups, as well as with those reported in previous trials investigating UMEC 62.5 μg as a monotherapy [12–14]. This suggests that symptomatic patients treated with combination ICS/LABA often have the potential for clinically important improvements in lung function [15]. The consistency of improvement observed with all other endpoints when examining UMEC 62.5 μg + ICS/LABA versus PBO + ICS/LABA in the overall ITT population is also supportive of this view. Moreover, in contrast with the individual studies, which were powered to only examine lung function outcomes, the analysis of pooled data resulted in far more consistent changes in PROs [10, 11].
When analyzing patients by GOLD B and GOLB D subgroups, improvements in lung function with UMEC 62.5 μg + ICS/LABA versus PBO + ICS/LABA were numerically greater in patients with better lung function at study entry, i.e., patients with GOLD B versus GOLD D COPD. These improvements in symptomatic patients with GOLD B COPD using ICS/LABA therapy could challenge recommendations that triple therapy should be reserved for patients only with GOLD D COPD.
In contrast to the lung function findings, patients in the GOLD D subgroup showed a greater symptomatic benefit with triple therapy versus PBO + ICS/LABA than patients in GOLD B based on reductions in daily rescue-medication use and changes in SGRQ total score. Despite this finding, it was notable that a similar increase in the proportion of patients deriving a clinically important increase in health status (SGRQ improvement of ≥4 units [16]) was observed with triple therapy versus PBO + ICS/LABA in both GOLD B and GOLD D patient subgroups. In support of this finding, similar reductions in COPD exacerbation risk (UMEC 62.5 μg + ICS/LABA versus PBO + ICS/LABA) were also observed in both GOLD B and D subgroups, although the reduction in the GOLD B subgroup was not statistically significant.
In this post hoc pooled analysis, we also examined the influence of the type of ICS/LABA therapy used concomitantly in the four studies, as well as whether once-daily or twice-daily ICS/LABA therapy provided a different opportunity to demonstrate an incremental efficacy gain when stepping up therapy with the addition of UMEC 62.5 μg. Reassuringly, we found that this aspect of the study design had little impact on the study findings, as efficacy improvements were consistently seen with UMEC 62.5 μg as part of an open triple regimen, irrespective of the dosing regimen of the concurrent ICS/LABA therapy.
Currently, there is a paucity of data showing the benefit of open triple therapy compared with ICS/LABA on COPD exacerbations. For both moderate (requiring a prescription of oral corticosteroids) and severe (resulting in hospitalizations) exacerbations, the benefit of adding a LAMA to ICS/LABA therapy is currently only well-documented in the context of a large real-world database study [5]. Data from large long-term randomized controlled trials (RCTs) to corroborate this finding are lacking. Among the limited number of RCTs reported, Aaron et al. [17] failed to show a clear benefit of triple therapy (tiotropium + FP/SAL) versus tiotropium on moderate exacerbations in a small, 12-month study confounded by very high dropout rates. However, they were able to show a reduction in severe exacerbations with triple therapy [17]. In this post hoc analysis of over 1600 patients, despite the short study length, we found a statistically significant reduction in the risk of a first moderate/severe exacerbation when adding UMEC 62.5 μg to ICS/LABA therapy. This finding was consistent across subgroups, despite the low number of events reported. One other larger, but shorter (3 months) study of triple therapy versus tiotropium corroborates these findings [18]. As high dropout rates may confound many long-term exacerbation studies performed in high-risk patients [17, 19], the approach of pooling data from short-term studies may provide an alternative insight on how best to examine exacerbations in higher-risk patients with COPD. However, it is important to recognize a key limitation of our findings: that they have been obtained as part of a post hoc analysis. Caution is also needed in generalizing the magnitude of the exacerbation benefits observed here, as experience of a previous exacerbation was not an inclusion criteria for the study, thereby potentially minimizing the level of events observed.
UMEC 62.5 μg open triple therapy was well tolerated and did not increase the overall incidence of AEs or cardiovascular AEs or SAEs versus PBO + ICS/LABA. The overall incidence of SAEs (fatal and non-fatal) in this short study period was low in both treatment groups and numerically lower in patients receiving triple therapy. Further research is therefore warranted to verify these findings in a large, prospective RCT. The InforMing the PAthway of COPD Treatment (IMPACT; ClinicalTrials.gov identifier: NCT02164513) study is currently ongoing and may answer some of these critical questions regarding COPD treatment [20]. Active pharmacovigilance evaluation of these treatments is also underway to further characterize their safety profiles.
The strengths of this post hoc analysis were that it included four studies with high completion and retention rates. The design of these double-blind, PBO-controlled studies was robust. Two replicate studies were performed for addition of UMEC to FP/SAL and to FF/VI, thus confirming efficacy and safety results. Although these post hoc analyses used data pooled from four studies of short duration, they provide new information about UMEC 62.5 μg added to ICS/LABA. Additional studies could compare triple therapy to LAMA/LABA dual therapy, to ascertain the treatment benefits of ICS in the triple combination. Our analysis also focused only on the GOLD guidelines in place at the time of the study, dividing patients into subgroups based on the A–D classification, but lacked data in less symptomatic patients in groups A and C. As the GOLD guidelines are updated annually, future analyses may require further refinement. The current GOLD guidelines have limited information on phenotypes such as the asthma–COPD overlap syndrome [1]. In an attempt to address such limitations, other national guidelines for the treatment of patients with COPD have been developed, for example, in Spain [21], Finland [22] and the Czech Republic [23]. Future studies could investigate which specific phenotypes, highlighted in these national guidelines [21–23], would benefit from triple therapy with LAMA + ICS/LABA.
Conclusions
UMEC 62.5 μg added to ICS/LABA provided clinically important improvements in lung function from the first to the last dose of treatment, versus PBO + ICS/LABA in symptomatic patients with COPD. These lung function improvements occurred irrespective of GOLD B or D classification or the ICS/LABA regimen used. UMEC 62.5 μg triple therapy was well tolerated and improved daily rescue medication use and health-related quality of life, and reduced the risk of moderate/severe COPD exacerbations in the short 3-month follow-up period.
References
GOLD. Global Initiative for Chronic Obstructive Lung Disease (GOLD). 2015. Available from: http://www.goldcopd.org/. Accessed August 10, 2015.
Dransfield MT, Bailey W, Crater G, et al. Disease severity and symptoms among patients receiving monotherapy for COPD. Prim Care Respir J. 2011;20:46–53.
Manoharan A, Short PM, Anderson WJ, Lipworth BJ. Impact of long-acting bronchodilators and exposure to inhaled corticosteroids on mortality in COPD: a real-life retrospective cohort study. Lung. 2014;192:649–52.
Kozma CM, Paris AL, Plauschinat CA, Slaton T, Mackowiak JI. Comparison of resource use by COPD patients on inhaled therapies with long-acting bronchodilators: a database study. BMC Pulm Med. 2011;11:61.
Short PM, Williamson PA, Elder DH, et al. The impact of tiotropium on mortality and exacerbations when added to inhaled corticosteroids and long-acting beta-agonist therapy in COPD. Chest. 2012;141:81–6.
Frith PA, Thompson PJ, Ratnavadivel R, et al. Glycopyrronium once-daily significantly improves lung function and health status when combined with salmeterol/fluticasone in patients with COPD: the GLISTEN study-a randomised controlled trial. Thorax. 2015;70:519–27.
Singh D, Brooks J, Hagan G, Cahn A, O’Connor BJ. Superiority of “triple” therapy with salmeterol/fluticasone propionate and tiotropium bromide versus individual components in moderate to severe COPD. Thorax. 2008;63:592–8.
GlaxoSmithKline. INCRUSE® Summary of product characteristics. 2014. Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/002809/human_med_001755.jsp&mid=WC0b01ac058001d124. Accessed August 26, 2015.
GlaxoSmithKline. INCRUSE® Prescribing Information. 2014. Available from: https://www.gsksource.com/pharma/content/dam/GlaxoSmithKline/US/en/Prescribing_Information/Incruse_Ellipta/pdf/INCRUSE-ELLIPTA-PI-PIL.PDF. Accessed September 7, 2015.
Siler TM, Kerwin E, Singletary K, Church A. Efficacy and safety of umeclidinium added to fluticasone propionate/salmeterol in patients with COPD: results of two randomized, double-blind studies. COPD. 2015;13(1):1–10.
Siler TM, Kerwin E, Sousa AR, et al. Efficacy and safety of umeclidinium added to fluticasone furoate/vilanterol in chronic obstructive pulmonary disease: results of two randomized studies. Respir Med. 2015;109:1155–63.
Donohue JF, Anzueto A, Brooks J, et al. A randomized, double-blind dose-ranging study of the novel LAMA GSK573719 in patients with COPD. Respir Med. 2012;106:970–9.
Donohue JF, Maleki-Yazdi MR, Kilbride S, et al. Efficacy and safety of once-daily umeclidinium/vilanterol 62.5/25 mcg in COPD. Respir Med. 2013;107:1538–46.
Trivedi R, Richard N, Mehta R, Church A. Umeclidinium in patients with COPD: a randomised, placebo-controlled study. Eur Respir J. 2014;43:72–81.
Donohue JF. Minimal clinically important differences in COPD lung function. COPD. 2005;2:111–24.
Jones PW. St. George’s Respiratory Questionnaire: MCID. COPD. 2005;2:75–9.
Aaron SD, Vandemheen KL, Fergusson D, et al. Tiotropium in combination with placebo, salmeterol, or fluticasone–salmeterol for treatment of chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2007;146:545–55.
Welte T, Miravitlles M, Hernandez P, et al. Efficacy and tolerability of budesonide/formoterol added to tiotropium in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;180:741–50.
Vestbo J, Anderson JA, Calverley PM, et al. Bias due to withdrawal in long-term randomised trials in COPD: evidence from the TORCH study. Clin Respir J. 2011;5:44–9.
GlaxoSmithKline. A Study Comparing the Efficacy, Safety and Tolerability of Fixed Dose Combination (FDC) of FF/UMEC/VI With the FDC of FF/VI and UMEC/VI; Administered Once-daily Via a Dry Powder Inhaler (DPI) in Subjects With Chronic Obstructive Pulmonary Disease (COPD). 2015. Availble from: https://clinicaltrials.gov/ct2/results?term=NCT02164513&Search=Search. Accessed August 30, 2015.
Miravitlles M, Soler-Cataluňa JJ, Calle M, et al. Spanish COPD Guidelines (GesEPOC): Pharmacological Treatment of Stable COPD. Arch Bronconeumol. 2012;48:247–57.
Kankaanranta H, Harju T, Kilpeläinen M, et al. Diagnosis and pharmacotherapy of stable chronic obstructive pulmonary disease: the finnish guidelines. Basic Clin Pharmacol Toxicol. 2015;116:291–307.
Koblizek V, Chlumsky J, Zindr V, et al. Chronic Obstructive Pulmonary Disease: Official diagnosis and treatment guidelines of the Czech Pneumological and Phthisiological Society; a novel phenotypic approach to COPD with patient-oriented care. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2013;157:189–201.
Acknowledgments
This post hoc analysis was performed by GSK (study number 202067). The article processing charges for this publication were funded by GSK. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. Editorial support in the form of developing the first draft based on author input, referencing, editing and incorporation of author comments, was provided by Gillian Groeger, PhD, Fishawack Indicia Ltd, UK, and funded by GSK. Data within this manuscript were presented at ATS 2015 (poster number: P548; abstract: Siler T, et al. AJRCCM 2015;191:A5778) and at ERS 2015 (PA1490).
Disclosures
Thomas M. Siler is part of a speaker bureau for AstraZeneca, and Boehringer Ingelheim; and has received research support from AstraZeneca, Boehringer Ingelheim, Forest Research Institute, GSK, Novartis, Pearl Therapeutics, Theravance and Sunovion. Edward Kerwin has served on advisory boards, speaker panels or received travel reimbursement from Amphastar, AstraZeneca (Pearl), Boehringer Ingelheim, Forest, Mylan, Novartis, Sunovion, Teva and Theravance, and has conducted multicenter clinical research trials for approximately 40 pharmaceutical companies. Lee Tombs is a contingent worker on assignment at GSK. William A. Fahy is an employee of GSK and owns stocks/shares in GSK. Ian Naya is an employee of GSK and owns stocks/shares in GSK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This article is based on previously conducted studies, and does not contain any new studies with human or animal subjects performed by any of the authors.
Additional information
Enhanced content for this article can be found http://www.medengine.com/Redeem/2244F0605D4F8341.
Lee Tombs is a Contingent worker who is working on assignment at GSK.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Siler, T.M., Kerwin, E., Tombs, L. et al. Triple Therapy of Umeclidinium + Inhaled Corticosteroids/Long-Acting Beta2 Agonists for Patients with COPD: Pooled Results of Randomized Placebo-Controlled Trials. Pulm Ther 2, 43–58 (2016). https://doi.org/10.1007/s41030-016-0012-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-016-0012-4