Abstract
Background
Medications with anticholinergic and/or sedative properties are commonly used in the management of psychiatric illnesses. The burden of anticholinergic and sedative medication use has been measured by the Drug Burden Index (DBI) score tool. A higher DBI score has been associated with increased risk of falls, bone and hip fractures, and functional and cognitive impairment, among other serious health outcomes, especially in older adults.
Objectives
We aimed to describe the drug burden in older adults with psychiatric illnesses using DBI, determine the factors that are associated with the drug burden measured by DBI, and examine the association between DBI score and Katz for activities of daily living (ADL) index.
Methods
A cross-sectional study was conducted in the psychogeriatric division of an aged-care home. The study sample comprised all inpatients, aged ≥ 65 years, diagnosed with psychiatric illness. The data obtained included demographic characteristics, duration of hospital stay, primary psychiatric diagnosis and comorbidities, functional status using the Katz ADL index, and cognitive status using the Mini-Mental State Examination (MMSE) score. DBI score was calculated for each anticholinergic and sedative medication used.
Results
Of the 200 patients eligible for analysis, 106 (53.1%) were females and the mean age was 76 ± 9 years. The most commonly encountered chronic disorders were hypertension 102 (51%) and schizophrenia 94 (47%). The use of drugs with anticholinergic and/or sedative effects was seen in 163 (81.5%) patients; the mean DBI score was 1.25 ± 1. The results of the multinomial logistic regression showed that schizophrenia (odds ratio (OR) = 2.1 (95% confidence interval (CI) 1.57–4.45), p = 0.01), level of dependency (OR = 3.50 (95% CI 1.38–5.70), p = 0.001), and polypharmacy (OR = 2.99 (95% CI 2.15–4.29), p = 0.003) were significantly associated with DBI score ≥ 1 compared to DBI score 0.
Conclusions
The study showed that anticholinergic and sedative medication exposure measured by DBI was associated with higher levels of dependency on the Katz ADL index in a sample of older adults with psychiatric illnesses from an aged-care home.
Similar content being viewed by others
Increasing exposure to medication with anticholinergic and sedative effects, measured with the Drug Burden Index (DBI), is associated with increased levels of dependence in the Katz for activities of daily living index in older adults with psychiatric illnesses. |
Older adults with schizophrenia and polypharmacy had higher odds for a higher DBI score. |
Anticholinergic and sedative medication use and their cumulative burden should be closely monitored to improve geriatric care. |
1 Introduction
Older adults are at a significant risk of developing psychiatric illnesses, and are frequently exposed to a high burden of drugs due to age-related changes in the brain and concurrent chronic conditions [1]. The treatment of psychiatric diseases frequently involves the use of drugs having anticholinergic and/or sedative properties [2]. Other medical diseases for which these drugs may be prescribed include Parkinson's disease, cardiovascular illness, gastrointestinal and metabolic abnormalities, and respiratory diseases.
The use of medications with anticholinergic and sedative properties has commonly been implicated with an increased risk of falls, bone and hip fractures, functional and cognitive impairment, among other serious adverse events [3,4,5,6,7,8,9]. These side effects are a significant concern for the residents of aged-care homes with psychiatric illnesses, given the high prevalence of polypharmacy, comorbidities, and age-related changes in this population [10,11,12]. Therefore, these medications are generally considered inappropriate in older adults, and it is recommended that their use be limited in this population [13].
The Drug Burden Index (DBI) is a clinical risk assessment tool that has been validated to quantify the cumulative exposure to sedative and anticholinergic drugs [14]. The DBI provides a dose-related measure of burden by accounting for the relationship between prescribed dose and dose-response curve, in contrast to other existing medication burden indices that evaluate anticholinergic and sedative load separately. By summing the scores for the pertinent drugs, the patient's overall DBI score is determined [14].
To determine the effect of these types of medications on cognitive and functional performance in older adults, associations between DBI scores and objective measures (i.e., Mini-Mental State Examination (MMSE), Addenbrooke's Cognitive Examination, Katz index for activities of daily living (ADL), etc.) were investigated. A higher DBI score was associated with a variety of detrimental health outcomes, including poor cognitive and functional performance, frailty, and falls in older adults [15,16,17,18].
In an Irish cohort of community-dwelling older adults, high DBI exposure (DBI score ≥ 1) versus none was significantly associated with impaired function as measured by the Katz ADL [19].
In older adults with psychiatric illnesses, polypharmacy with psychotropic medication is very common especially in those suffering from schizophrenia or depression, and patients often experience a high burden from the side effects of psychotropic medications in addition to the increased healthcare costs [20,21,22]. Determining the drug burden index and confirming its association with impaired cognitive and functional impairment in this population may assist physicians in the risk-benefit assessment when prescribing and therefore minimize drug-related risks. However, to the best of our knowledge no studies were conducted in older psychiatric patients as in other relevant patient groups [23]. Accordingly, we aimed in this study to (a) describe the drug burden in older adults with psychiatric illnesses using DBI; (b) identify the most frequently reported therapeutic classes contributing to the total burden; (c) determine the factors that are associated with the drug burden measured by the DBI; and (d) examine the association between the DBI score and Katz ADL index.
2 Methods
2.1 Study Setting
A cross-sectional study was conducted in one aged-care home in Beirut, Lebanon between March and June 2022. This facility has a geriatrics division that provides healthcare for about 300 resident-patients (long-stay inpatients) and is committed to optimizing the health of older adults with multiple chronic conditions, life-limiting illness, frailty or a disability that is associated with chronic disease, aging or injury. Additionally, the aged-care home includes a psychogeriatric division that provides care for 300 resident patients suffering from a psychiatric or psychological disorder, such as depression, anxiety, bipolar disorder or schizophrenia, which is where we conducted this study.
2.2 Participants, Recruitment and Ethics
The study sample comprised all current inpatients, aged ≥ 65 years, diagnosed with psychiatric illness, who received a comprehensive geriatric assessment by a trained physician, taking at least one chronic medication, and who had at least 6 months’ stay at the aged home-care facility. Exclusion criteria were patients with incomplete medical records. A researcher visited the psychogeriatric division over 2 months and completed a standardized assessment of medical records including the clinical case notes for all patients who met the inclusion criteria. The demographic and clinical information was retrieved from the hard-copy medical record of each patient and collected into an electronic data collection form. The form included demographic characteristics (i.e., age, gender, weight, height, marital status, education), duration of hospital stay (in months), primary psychiatric diagnosis, and comorbidities according to ICD-10, functional and cognitive status. Comorbidities were assessed using the Charlson Comorbidity Index (CCI), functional status using the Katz index ADL, and cognitive status using the MMSE score [24,25,26]. In addition, we recorded the number of medications currently taken including the name, dose, frequency and date on which each medication was initiated. All medications given were reported as generic and brand names and were then classified according to the Anatomical Chemical Therapeutic Classification codes [27]. Patients receiving five or more medications daily were considered as having polypharmacy. One clinical pharmacist independently reviewed and approved data accuracy.
The data in this study have been collected and processed in such a way as to comply with data protection and privacy. Written informed consent from the patients or caregivers was not needed since this study had no physiologic, psychologic, or social risks for the patients due to its observational nature. The Institutional Review Board approved the study protocol (2022RC-007-LIUSOP).
2.3 Measures
We relied on published guidelines to calculate the DBI score. The DBI for each medication was calculated by dividing the daily dose (D) by the sum of the minimum effective daily dose (δ) and the daily dose of each drug product (D) (DBI = D/(δ +D)) [14]. Then, the total, or cumulative, DBI was calculated through summation of scores associated with each medication. Medications with anticholinergic and/or sedative properties were identified using drug lists from the anticholinergic cognitive burden scale and sedative load model, respectively [28, 29].
The minimum effective daily dose for older adults was identified using the Lexicomp Geriatric Dosage Handbook; if dosing guidance for older adults was unavailable in this reference, the lowest recommended adult maintenance dose was used [30]. In case a medication had more than one indication, we used the dosing recommendation for the indication most commonly prescribed for older adults.
In accordance with Hilmer et al., medications with both anticholinergic and sedative properties were classified as anticholinergic [14]. As per previous studies, the following medications were excluded from the DBI calculation: topical formulations, inhaled formulations, medications taken on an “as required” or “prn” basis, and over-the-counter drugs unless used on a daily basis [17].
DBI scores for participants were calculated as a continuous variable and then transformed into a categorical variable with three levels: DBI score 0 (no DBI exposure), DBI score 0 > 1 (low), and DBI score ≥ 1 (high). This reflects the categories used elsewhere in the literature [31].
Of the most commonly used functionality scores, the Katz ADL is more conducive to a long-term hospital setting or for patients who are severely sick [32]. In our study the Katz score measured the performance in activities of daily living and individuals were graded on a binary scale of dependent or independent for 6 ADL: bathing, dressing, toileting, transferring, continence, and feeding. Patients were classified into: independent (Katz score = 6), partially dependent (Katz score = 1–5), or dependent (Katz score = 0) [25].
The most recent MMSE score was recorded, the test was performed by the attending physician to measure cognitive impairment, not more than 2 months prior to data collection. The MMSE ranges from 0 to 30 and patients were classified as having severe (MMSE = 0–9), moderate (MMSE = 10–19)|, mild (MMSE = 20–24), and no cognitive impairment (MMSE = 25–30) [26].
2.4 Data Analysis
Descriptive analysis of patients’ demographic and clinical characteristics was performed. We used Student’s t test for continuous variables and the Chi-square test for categorical data to identify the demographic and clinical variables associated with the DBI score. Variables with a p value < 0.2 were entered into the logistic regression model. Multinomial logistic regression was used to identify the independent variables that remained associated with the DBI score. A set of clinical variables, scores, and side effects were entered into the regression model as independent variables, and the DBI score (0, > 0 <1, ≥ 1) was entered as the dependent variable; a DBI score of 0 was used as the reference category. In this model, the statistical test used was Pearson’s χ2 test. The odds ratio (OR) with 95% confidence interval (CI) was used as a measure of association. Statistical significance was set at p < 0.05. Analysis of covariance (ANCOVA) was used to compare the mean of the continuous variable for the Katz ADL index between subjects exposed to three different levels of DBI score.
3 Results
Of the 300 patients present at the psychogeriatric unit, 200 met the inclusion criteria and were eligible for analysis. The study cohort included 106 (53.1%) females and the mean age was 76 ± 9 years. The most commonly recorded psychiatric illness and comorbidity were schizophrenia 94 (47%) and hypertension 102 (51%), respectively, while the most common geriatric syndrome experienced was falls and fractures 125 (62.5%). Almost half of enrolled patients were dependent according to a Katz score of 98 (49.0%) and had cognitive impairment according to an MMSE score 106 (53.0%). Severe CCI was identified in 86 (43%) of participants, and the majority were on polypharmacy 136 (68%).
The use of drugs with anticholinergic and/or sedative effects was seen in 163 (81.5%) patients, the mean DBI score was 1.25 ± 1 and 102 (51%) of participants had a high DBI score ≥ 1 (Table 1).
The total number of drugs with anticholinergic and/or sedative effects used was 363 with an average of 2.2 drugs per patient. Of those, the most commonly used drug class was antipsychotics 180 (49.6%), followed by antidepressants 33 (9.1%), antihistamines 31 (8.5%), and benzodiazepines 22 (6.1%). The most frequent medication identified was risperidone 52 (14.3%) (Table 2).
Patients’ demographic and clinical characteristics associated with a DBI score are shown in Table 3. The bivariate analysis results showed that age p < 0.001, schizophrenia p < 0.001, level of dependency (Katz index) p = 0.001, MMSE score p = 0.02, CCI p = 0.02, and polypharmacy p = 0.03 were statistically significant. The results of the multinomial logistic regression showed that only age (OR = 0.84 (95% CI 0.65–0.91), p < 0.001), schizophrenia (OR = 2.1 (95% CI 1.57–4.45), p = 0.010), level of dependency (OR = 3.50 (95% CI 1.38–5.70), p = 0.001), and polypharmacy (OR = 2.99 (95% CI 2.15–4.29), p = 0.003) were significantly associated with a DBI score ≥ 1 compared to a DBI score of 0.
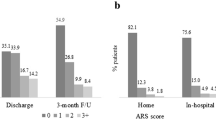
Figure 1 shows the adjusted means for Katz index for ADL.
Analysis of covariance for the association of adjusted means of KATZ index with increasing drug burden index. Significantly lower scores of the Katz index for ADL were identified for those with a DBI score of ≥ 1 (p = 0.001; mean score 1.98, 95% CI 1.54–2.42) compared to those with DBI 0 (mean score 3.29, 95% CI 2.22–4.36) after adjusting for confounders (gender, age, CCI, and history of falls and fractures)
4 Discussion
To the best of our knowledge, this is the first study to investigate DBI in a sample of older adults with psychiatric illnesses in Lebanon. Our results show that, in contrast to previous research on aged home-care older adults, those with psychiatric illnesses had a higher cumulative exposure to both sedative and anticholinergic drugs; more than 80% of the study population had a DBI score > 0 [15, 33, 34]. A longitudinal analysis of data from Dutch aged home-care residents between June 2005 and April 2014 revealed that 76% of participants had significant exposure to anticholinergic and sedative medications (as measured by the DBI) [33]. Furthermore, in Australia’s residential aged care facilities, 78% of older adults had DBI scores greater than 1 [34].
After adjusting for confounders, the results of the multinomial logistic regression showed that the oldest-old group had lower odds for higher DBI scores, whereas those with schizophrenia, a higher level of dependency, and polypharmacy had higher odds for higher DBI score.
The analysis of covariance identified higher levels of dependence in the Katz ADL index as DBI scores increased. This is similar to the findings of previous studies that examined the association of DBI score with Katz index activities of daily living in Irish older adults, and DBI score with instrumental activities of daily living in older Australian men [19, 35].
Schizophrenia was the most common psychiatric illness identified and the only comorbidity associated with a higher DBI score. This is not surprising and could be explained by the fact that patients with schizophrenia are highly exposed to antipsychotics with anticholinergic and sedative burden. While the use of these classes of medications may be inevitable for the treatment of these chronic illnesses, other agents from the same therapeutic class may have lower anticholinergic/sedative activity with retained effectiveness, and therefore their use should be favored [36].
In the present study, DBI was significantly associated with polypharmacy. This is in concordance with the findings of Okudur et al. [37], where the highest relationship between polypharmacy and medication burden scales was with DBI score among outpatient older adults.
The association of DBI score with cognitive function measured by MMSE did not remain
significant after adjusting for covariates. This is in line with the results of Cao et al. and Wouters et al., and is largely attributable to the neurodegenerative processes that could be a stronger determinant of cognitive decline in aged-care residents, many of whom have dementia, than anticholinergic and sedative medication burden [33, 38].
The use of the DBI in clinical practice is supported by the results of current and past longitudinal and cross-sectional studies [23]. The DBI score may be a valuable tool for identifying people who have high exposure to sedatives and anticholinergics, which may worsen their functional impairment, especially those with psychiatric illnesses. Such individuals are probably candidates for deprescribing practices and pharmacist-performed medication reviews [39].
Although this is the first study to examine DBI scores in older adults with psychiatric illnesses, it should be viewed in light of its limitations. Our cross-sectional design precludes drawing causal conclusions. As a result, longitudinal research is required to determine whether older adults with psychiatric illnesses and a high drug burden experience faster functional decline, especially that impairments in functional performance are characteristic of people with schizophrenia. Despite having an equal number of male and female participants, our cohort was single-centered. Future research should therefore replicate these findings in a more diverse and multi-centered cohort.
5 Conclusion
The present study showed that anticholinergic and sedative medication exposure measured by DBI was associated with higher levels of dependency on Katz ADL index in a sample of older adults with psychiatric illnesses from an aged-care facility. With growing concerns about polypharmacy in the elderly, the current study findings suggest that anticholinergic and sedative medication use and their cumulative burden should be closely monitored to improve geriatric care.
References
Khandelwal SK. In: Ageing in India. Situational analysis and planning for the future. New Delhi: Rakmo Press; 2003. Mental health of older people
Santosh PJ, Baird G. Psychopharmacotherapy in children and adults with intellectual disability. Lancet. 1999;354:233–42.
Richardson K, Bennett K, Kenny RA. Polypharmacy including falls risk increasing medications and subsequent falls in community-dwelling middle aged and older adults. Age Ageing. 2015;44:90–6.
Chatterjee S, Bali V, Carnahan RM, et al. Anticholinergic medication use and risk of fracture in elderly adults with depression. J Am Geriatr Soc. 2016;64:1492–7.
Fox C, Smith T, Maidment I, et al. Effect of medications with anticholinergic properties on cognitive function, delirium, physical function and mortality: a systematic review. Age Ageing. 2014;43:604–15.
Pasina L, Djade CD, Lucca U, et al. Association of anticholinergic burden with cognitive and functional status in a cohort of hospitalized elderly: comparison of the anticholinergic cognitive burden scale and anticholinergic risk scale: results from the REPOSI study. Drugs Aging. 2013;30:103–12.
Gray SL, Penninx BW, Blough DK, et al. Benzodiazepine use and physical performance in community-dwelling older women. J Am Geriatr Soc. 2003;51:1563–70.
Landi F, Russo A, Liperoti R, et al. Anticholinergic drugs and physical function among frail elderly population. Clin Pharmacol Ther. 2007;81:235–41.
Ancelin ML, Artero S, Portet F, et al. Non-degenerative mild cognitive impairment in elderly people and use of anticholinergic drugs: longitudinal cohort study. BMJ. 2006;332:455–9.
Doraiswamy PM, Husain MM. Anticholinergic drugs and elderly people: a no brainer? Lancet Neurol. 2006;5:379–80.
Mintzer J, Burns A. Anticholinergic side-effects of drugs in elderly people. J R Soc Med. 2000;93:457–62.
Peters N. Antimuscarinic side-effects of anticholinergic medications in the elderly. Arch Intern Med. 1989;149:2414–20.
The American Geriatrics Society. American geriatrics society updated beers criteria for potentially inappropriate medication use in older adults. Beers criteria update expert panel. J Am Geriatr Soc. 2012;2012:616–31.
Hilmer SN, Mager DE, Simonsick EM, Coa Y, Ling SM, Windham BG. A drug burden index to define the functional burden of medications in older people. Arch Intern Med. 2007;167:781–7.
Wilson NM, Hilmer SN, March LM, Cameron ID, Lord SR, Seibel MJ, et al. Associations between drug burden index and falls in older people in residential aged care. J Am Geriatr Soc. 2011;59:875–80.
Gnjidic D, Le Couteur DG, Naganathan V, Cumming RG, Creasey H, Waite LM, et al. Effects of drug burden index on cognitive function in older men. J Clin Psychopharmacol. 2012;32:273–7.
Nishtala PS, Narayan SW, Wang T, et al. Associations of drug burden index with falls, general practitioner visits, and mortality in older people. Pharmacoepidemiol Drug Saf. 2014;23:753–8.
Dauphinot V, Faure R, Omrani S, et al. Exposure to anticholinergic and sedative drugs, risk of falls, and mortality: an elderly inpatient, multicenter cohort. J Clin Psychopharmacol. 2014;4:565–70.
Byrne CJ, Walsh C, Cahir C, Bennett K. Impact of drug burden index on adverse health outcomes in Irish community-dwelling older people: a cohort study. BMC Geriatr. 2019;19(1):121. https://doi.org/10.1186/s12877-019-1138-7. (Published 2019 Apr 29).
Patel MX, Bishara D, Jayakumar S, Zalewska K, Shiers D, Crawford MJ, et al. Quality of prescribing for schizophrenia: evidence from a national audit in England and Wales. Eur Neuropsychopharmacol. 2014;24(4):499–509.
Jureidini J, Tonkin A. Overuse of antidepressant drugs for the treatment of depression. CNS Drugs. 2006;20(8):623–32.
Young SL, Taylor M, Lawrie SM. BFirst do no harm. A systematic review of the prevalence and management of antipsychotic adverse effects. J Psychopharmacol. 2015;29(4):353–62.
Wouters H, van der Meer H, Taxis K. Quantification of anticholinergic and sedative drug load with the Drug Burden Index: a review of outcomes and methodological quality of studies. Eur J Clin Pharmacol. 2017;73(3):257–66. https://doi.org/10.1007/s00228-016-2162-6.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. J Am Med Assoc. 1963;185:914–9.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. https://doi.org/10.1016/0022-3956(75)90026-6.
World Health Organization. Anatomical chemical therapeutic classification system. WHO; 2011.
Indiana University of Aging Research ABP. The anticholinergic cognitive burden scale (2012 Update) Aging Brain Care, 2012. http://www.agingbraincare.org/uploads/products/ACB_scale_-_legal_size.pdf.
Linjakumpu T, Hartikainen S, Klaukka T, Koponen H, Kivelä SL, Isoaho R. A model to classify the sedative load of drugs. Int J Geriatr Psychiatry. 2003;18:542–5.
Semla T, Beizer J, Higbee M, editors. Geriatric dosage handbook: including clinical recommendations and monitoring guidelines. 21st ed. Lexicomp; 2016.
O’Connell J, Burke É, Mulryan N, et al. Drug burden index to define the burden of medicines in older adults with intellectual disabilities: an observational cross-sectional study. Br J Clin Pharmacol. 2018;84(3):553–67. https://doi.org/10.1111/bcp.13479.
Hartigan I. A comparative review of the Katz ADL and the Barthel Index in assessing the activities of daily living of older people. Int J Older People Nurs. 2007;2(3):204–12. https://doi.org/10.1111/j.1748-3743.2007.00074.x.
Wouters H, Hilmer SN, Twisk J, et al. Drug burden index and cognitive and physical function in aged care residents: a longitudinal study. J Am Med Dir Assoc. 2020;21(8):1086-1092.e1. https://doi.org/10.1016/j.jamda.2020.05.037.
Bosboom PR, Alfonso H, Almeida OP, Beer C. Use of potentially harmful medications and health-related quality of life among people with dementia living in residential aged care facilities. Dement Geriatr Cogn Dis Extra. 2012;2(1):361–71. https://doi.org/10.1159/000342172.
Gnjidic D, Cumming RG, Le Couteur DG, Handelsman DJ, Naganathan V, Abernethy DR, et al. Drug burden index andphysical function in older Australian men. Br J Clin Pharmacol. 2009;68:97–105.
Alexopoulos GS, Streim J, Carpenter D, Docherty JP. Expert consensus panel for using antipsychotic drugs in older patients. Using antipsychotic agents in older patients. J Clin Psychiatry. 2004;65(Suppl 2):5–104.
Okudur SK, Dokuzlar O, Aydin AE, Kocyigit SE, Soysal P, Isik AT. The evaluation of relationship between polypharmacy and anticholinergic burden scales. North Clin Istanb. 2021;8(2):139–44. https://doi.org/10.14744/nci.2020.17136. (Published 2021 Mar 11).
Cao YJ, Mager DE, Simonsick EM, Hilmer SN, Ling SM, Windham BG, et al. Physical and cognitive performance and burden of anticholinergics, sedatives, and ACE inhibitors in older women. Clin Pharmacol Ther. 2008;83(3):422–9.
Castelino RL, Hilmer SN, Bajorek BV, Nishtala P, Chen TF. Drug Burden Index and potentially inappropriate medications in community-dwelling older people: the impact of Home Medicines Review. Drugs Aging. 2010;27(2):135–48. https://doi.org/10.2165/11531560-000000000-00000.
Acknowledgements
We would like to thank Gracia Yaghi who assisted in the collection and cross-checking of data as it was transferred from hard copy records to the electronic survey.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Not applicable.
Conflict of Interest
The author has no conflicts of interest to declare.
Ethical Approval
This study was approved by the Institutional Review Board at the Lebanese International University (approval number 2022RC-007-LIUSOP).
Consent for Publication
Not applicable.
Availability of Data and Material
The data are available on request from the corresponding author.
Code Availability
Not available.
Author Contribution
Design/conduct of the study (BC); acquisition of subjects and/or data (BC); analysis and interpretation of data (BC); preparation of manuscript (BC).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chahine, B. Drug Burden Index in Older Adults with Psychiatric Illnesses: A Cross-Sectional Study. Drugs - Real World Outcomes 10, 283–290 (2023). https://doi.org/10.1007/s40801-023-00357-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-023-00357-3