Abstract
Objective
Attempts to discontinue calcineurin inhibitors (CNIs) early after renal transplantation without conversion to an alternative immunosuppressive have failed due to high rates of acute rejection. Data on “late” CNI withdrawal are lacking so far.
Design and method
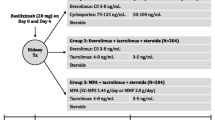
We carried out a matched case-control study on the effects of CNI withdrawal on graft loss and mortality in 90 patients (1500 screened) with advanced graft dysfunction (serum creatinine > 3.5 mg/dl) and a cyclosporine-based triple immunosuppressive regimen at the Charité University Hospital, Berlin.
Results
Cyclosporine was withdrawn at a mean of 54.0 ± 32.8 months post-transplant in 45 subjects. Whereas estimated glomerular filtration rate (eGFR) did not significantly differ between the groups at this time (12.4 ± 2.7 vs. 14.7 ± 8.9 in the control group, p = 0.08), it was significantly higher in subjects undergoing withdrawal after 120 months (Δ 4.1 ml/min; p < 0.001). In a Cox regression analysis adjusted for age, gender and eGFR, patients with CNI withdrawal showed better survival rates for the combined endpoint death/graft loss (hazard ratio, HR [95% confidence interval]: 0.19 [0.12–0.33], p = 0.001) compared to matched controls. The survival benefit was significant for the endpoints death (p = 0.01) and graft loss (p = 0.001).
Conclusions
CNI withdrawal was associated with improved survival rates in patients with advanced graft dysfunction in this retrospective analysis.


Similar content being viewed by others
References
Meier-Kriesche HU, Schold JD, Srinivas TR, Kaplan B (2004) Lack of improvement in renal allograft survival despite a marked decrease in acute rejection rates over the most recent era. Am J Transpl 4(3):378–383
Nankivell BJ, Borrows RJ, Fung CL, O’Connell PJ, Chapman JR, Allen RD (2004) Calcineurin inhibitor nephrotoxicity: longitudinal assessment by protocol histology. Transplantation 78(4):557–565
Ojo AO, Held PJ, Port FK, Wolfe RA, Leichtman AB, Young EW, Arndorfer J, Christensen L, Merion RM (2003) Chronic renal failure after transplantation of a nonrenal organ. N Engl J Med 349(10):931–940. https://doi.org/10.1056/NEJMoa021744
Schwarz A, Haller H, Schmitt R, Schiffer M, Koenecke C, Strassburg C, Lehner F, Gottlieb J, Bara C, Becker JU, Broecker V (2010) Biopsy-diagnosed renal disease in patients after transplantation of other organs and tissues. Am J Transpl 10(9):2017–2025. https://doi.org/10.1111/j.1600-6143.2010.03224.x
Ekberg H, Grinyo J, Nashan B, Vanrenterghem Y, Vincenti F, Voulgari A, Truman M, Nasmyth-Miller C, Rashford M (2007) Cyclosporine sparing with mycophenolate mofetil, daclizumab and corticosteroids in renal allograft recipients: the CAESAR Study. Am J Transpl 7(3):560–570. https://doi.org/10.1111/j.1600-6143.2006.01645.x
Budde K, Becker T, Arns W, Sommerer C, Reinke P, Eisenberger U, Kramer S, Fischer W, Gschaidmeier H, Pietruck F, Investigators ZS (2011) Everolimus-based, calcineurin-inhibitor-free regimen in recipients of de-novo kidney transplants: an open-label, randomised, controlled trial. Lancet 377(9768):837–847. https://doi.org/10.1016/S0140-6736(10)62318-5
De Geest S, Schafer-Keller P, Denhaerynck K, Thannberger N, Kofer S, Bock A, Surber C, Steiger J (2006) Supporting medication adherence in renal transplantation (SMART): a pilot RCT to improve adherence to immunosuppressive regimens. Clin Transpl 20(3):359–368. https://doi.org/10.1111/j.1399-0012.2006.00493.x
Schena FP, Pascoe MD, Alberu J, del Carmen Rial M, Oberbauer R, Brennan DC, Campistol JM, Racusen L, Polinsky MS, Goldberg-Alberts R, Li H, Scarola J, Neylan JF, Sirolimus CTSG (2009) Conversion from calcineurin inhibitors to sirolimus maintenance therapy in renal allograft recipients: 24-month efficacy and safety results from the CONVERT trial. Transplantation 87(2):233–242. https://doi.org/10.1097/TP.0b013e3181927a41
Schulte K, Vollmer C, Klasen V, Brasen JH, Puchel J, Borzikowsky C, Kunzendorf U, Feldkamp T (2017) Late conversion from tacrolimus to a belatacept-based immuno-suppression regime in kidney transplant recipients improves renal function, acid-base derangement and mineral-bone metabolism. J Nephrol 30(4):607–615. https://doi.org/10.1007/s40620-017-0411-0
Marcen R, Morales JM, Fernandez-Rodriguez A, Capdevila L, Pallardo L, Plaza JJ, Cubero JJ, Puig JM, Sanchez-Fructuoso A, Arias M, Alperovich G, Seron D (2010) Long-term graft function changes in kidney transplant recipients. NDT Plus 3(Suppl_2):ii2–ii8. https://doi.org/10.1093/ndtplus/sfq063
Pestana JO, Grinyo JM, Vanrenterghem Y, Becker T, Campistol JM, Florman S, Garcia VD, Kamar N, Lang P, Manfro RC, Massari P, Rial MD, Schnitzler MA, Vitko S, Duan T, Block A, Harler MB, Durrbach A (2012) Three-year outcomes from BENEFIT-EXT: a phase III study of belatacept versus cyclosporine in recipients of extended criteria donor kidneys. Am J Transpl 12(3):630–639. https://doi.org/10.1111/j.1600-6143.2011.03914.x
Midtvedt K, Neumayer HH (2000) Management strategies for posttransplant hypertension. Transplantation 70(11 Suppl):SS64–S69
Fellstrom B (2000) Impact and management of hyperlipidemia posttransplantation. Transplantation 70(11 Suppl):SS51–S57
Jindal RM, Hjelmesaeth J (2000) Impact and management of posttransplant diabetes mellitus. Transplantation 70(11 Suppl):SS58–S63
Acknowledgements
We thank Simone Voigt for her indefatigable efforts in this study.
Funding
None.
Author information
Authors and Affiliations
Contributions
NP: designed and performed study, analyzed data. KY, FSS, FB, KM, BS, WZ, RV, NB: collected data. TG, PS: analyzed data. THW: designed and performed study, wrote the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Pagonas, N., Yusefi, K., Seibert, F.S. et al. Effects of late cyclosporine withdrawal on renal graft function and survival. J Nephrol 32, 315–321 (2019). https://doi.org/10.1007/s40620-018-0554-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-018-0554-7