Abstract
Objective
To evaluate whether computer-based prostate cancer screening decision aids enhance decision self-efficacy for African-American men, culturally relevant and reliable measures are needed. However, limited psychometric evidence exists on the health-related decision self-efficacy of African-American men. This study describes the development and psychometric evaluation of the 11-item Informed Prostate Cancer Screening Decision Self-Efficacy Scale among 354 African-American men.
Methods
Exploratory factor analysis was conducted with maximum-likelihood estimation and polychoric correlations followed by Promax and Varimax rotations.
Results
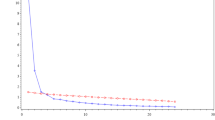
Exploratory factor analysis yielded a one-factor, 11-item model of the modified scale with excellent internal consistency reliability at 0.95 and factor loadings ranging from 0.70 to 0.90. Both parallel analysis and a scree plot confirmed the retention of one factor, and the standardized root mean square residual (0.06) indicated that the factor structure explained most of the correlations.
Conclusions
Findings suggest the one-factor, 11-item Informed Prostate Cancer Screening Decision Self-Efficacy Scale has excellent psychometric properties and utility in reliably measuring health-related decision self-efficacy in African-American men. Future research is needed to confirm this factor structure among socio-demographically diverse African Americans.

Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. https://doi.org/10.3322/caac.21551.
Kim EH, Andriole GL. Prostate-specific antigen-based screening: controversy and guidelines. BMC Med. 2015;13(1):61.
Fleshner K, Carlsson S, Roobol M. The effect of the USPSTF PSA screening recommendation on prostate cancer incidence patterns in the USA. Nat Rev Urol. 2017;14(1):26–37.
Gibson L, Tan AS, Freres D, Lewis N, Martinez L, Hornik RC. Nonmedical information seeking amid conflicting health information: negative and positive effects on prostate cancer screening. Health Commun. 2016;31(4):417–24.
Dhillon P, Grivas P, Raska P, Hickman D, Elson P, Awadalla A, et al. Informed decision making (IDM) for prostate cancer (PCa) screening in a high-risk population. J Clin Oncol. 2017;35(6_suppl):112. https://doi.org/10.1200/JCO.2017.35.6_suppl.112.
Jackson D, Owens O, Friedman DB, Hebert JR. An intergenerational approach to prostate cancer education: findings from a pilot project in the southeastern USA. J Cancer Educ. 2014;29(4):649–56. https://doi.org/10.1007/s13187-014-0618-x.
Drake B, Shelton R, Gilligan T, Allen J. A church-based intervention to promote informed decision-making for prostate cancer screening among African-American men. J Natl Med Assoc. 2010;102(3):164–71.
Ukoli F, Patel K, Hargreaves M, Beard K, Moton PJ, Bragg R, et al. A tailored prostate cancer education intervention for low-income African Americans: impact on knowledge and screening. J Health Care Poor Underserved. 2013;24(1):311–31.
Jackson D, Owens O, Friedman D, Dubose-Morris R. Innovative and community-guided evaluation and dissemination of a prostate cancer education program for African-American men and women. J Cancer Educ. 2015;30(4):779–85.
O’Connor A. User manual-decision self-efficacy scale. Ottawa Hospital Research Institute: Ottawa; 1995.
Ekúndayò OT, Tataw DB. Barriers to prostate cancer prevention and community recommended health education strategies in an urban African American community in Jackson, Mississippi. Soc Work Public Health. 2013;28(5):520–38.
O'Keefe EB, Meltzer JP, Bethea TN. Health disparities and cancer: racial disparities in cancer mortality in the United States, 2000–2010. Front Public Health. 2015;3:51. https://doi.org/10.3389/fpubh.2015.00051.
Wu I, Modlin CS. Disparities in prostate cancer in African American men: what primary care physicians can do. Cleve Clin J Med. 2012;79(5):313–20.
Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002;94(8):666.
Sanchez MA, Bowen DJ, Hart A, Spigner C. Factors influencing prostate cancer screening decisions among African American men. Ethn Dis. 2007;17(2):374–80.
American Cancer Society. Prostate Cancer: Early Detection. Atlanta, GA. 2013. http://www.cancer.org/acs/groups/cid/documents/webcontent/003182-pdf.pdf
Carter HB, Albertsen PC, Barry MJ, Etzioni R, Freedland SJ, Greene KL, et al. Early detection of prostate cancer: AUA guideline. J Urol. 2013;190(2):419–26.
Bibbins-Domingo K, Grossman DC, Curry SJ. The US Preventive Services Task Force 2017 draft recommendation statement on screening for prostate cancer: an invitation to review and comment. JAMA. 2017;317(19):1949–50.
Briss P, Rimer B, Reilley B, Coates RC, Lee NC, Mullen P, et al. Promoting informed decisions about cancer screening in communities and healthcare systems. Am J Prev Med. 2004;26(1):67–80.
Mullen PD, Allen JD, Glanz K, Fernandez ME, Bowen DJ, Pruitt SL, et al. Measures used in studies of informed decision making about cancer screening: a systematic review. Ann Behav Med. 2006;32(3):188–201.
Dy SM. Instruments for evaluating shared medical decision making: a structured literature review. Med Care Res Rev. 2007;64(6):623–49.
Allen JD, Mohllajee AP, Shelton RC, Drake BF, Mars DR. A computer-tailored intervention to promote informed decision making for prostate cancer screening among African American men. Am J Mens Health. 2009;3(4):340–51.
Allen JD, Othus MK, Hart A, Tom L, Li Y, Berry D, et al. A randomized trial of a computer-tailored decision aid to improve prostate cancer screening decisions: results from the take the wheel trial. Cancer Epidemiol Biomark Prev. 2010;19(9):2172–86.
Allen JD, Othus MK, Hart A Jr, Mohllajee AP, Li Y, Bowen D. Do men make informed decisions about prostate cancer screening? Baseline results from the “take the wheel” trial. Med Decis Mak. 2011;31(1):108–20.
Owens OL, Felder T, Tavakoli AS, Revels AA, Friedman DB, Hughes-Halbert C, et al. Evaluation of a computer-based decision aid for promoting informed prostate cancer screening decisions among African-American men: iDecide. Am J Health Promot. 2019;33(2):267–78. https://doi.org/10.1177/0890117118786866.
Lepore SJ, Wolf RL, Basch CE, Godfrey M, McGinty E, Shmukler C, et al. Informed decision making about prostate cancer testing in predominantly immigrant black men: a randomized controlled trial. Ann Behav Med. 2012 Jul 24;44(3):320–30.
Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 1982;37(2):122.
Bandura A. Social cognitive theory of self-regulation. Organ Behav Hum Decis Process. 1991;50(2):248–87.
Guntzviller LM, King AJ, Jensen JD, Davis LA. Self-efficacy, health literacy, and nutrition and exercise behaviors in a low-income, Hispanic population. J Immigr Minor Health. 2017;19(2):489–93.
de Menezes MC, Roux AVD, Lopes ACS. Fruit and vegetable intake: influence of perceived food environment and self-efficacy. Appetite. 2018;127:249–56.
Ha FJ, Hare DL, Cameron JD, Toukhsati SR. Heart failure and exercise: a narrative review of the role of self-efficacy. Heart Lung Circ. 2018;27(1):22–7.
Iwasaki Y, Honda S, Kaneko S, Kurishima K, Honda A, Kakinuma A, et al. Exercise self-efficacy as a mediator between goal-setting and physical activity: developing the workplace as a setting for promoting physical activity. Saf Health Work. 2017 Mar 1;8(1):94–8.
Pérez-Stable EJ, El-Toukhy S. Communicating with diverse patients: how patient and clinician factors affect disparities. Patient Educ Couns. 2018;101(12):2186–94.
Peek ME, Wilson SC, Gorawara-Bhat R, Odoms-Young A, Quinn MT, Chin MH. Barriers and facilitators to shared decision-making among African-Americans with diabetes. J Gen Intern Med. 2009;24(10):1135–9.
Hawkins JM, Mitchell J. The doctor never listens: older African American men’s perceptions of patient–provider communication. Soc Work Res. 2018;42(1):57–63.
Ogedegbe G, Mancuso CA, Allegrante JP, Charlson ME. Development and evaluation of a medication adherence self-efficacy scale in hypertensive African-American patients. J Clin Epidemiol. 2003;56(6):520–9.
Fernandez S, Chaplin W, Schoenthaler AM, Ogedegbe G. Revision and validation of the medication adherence self-efficacy scale (MASES) in hypertensive African Americans. J Behav Med. 2008;31(6):453–62. https://doi.org/10.1007/s10865-008-9170-7.
Sallis JF, Pinski RB, Grossman RM, Patterson TL, Nader PR. The development of self-efficacy scales for health-related diet and exercise behaviors. Health Educ Res. 1988;3(3):283–92.
Shin Y, Jang H, Pender NJ. Psychometric evaluation of the exercise self-efficacy scale among Korean adults with chronic diseases. Res Nurs Health. 2001;24(1):68–76.
Resnick B, Jenkins LS. Testing the reliability and validity of the self-efficacy for exercise scale. Nurs Res. 2000;49(3):154–9.
de Vries H, Dijkstra M, Kuhlman P. Self-efficacy: the third factor besides attitude and subjective norm as a predictor of behavioural intentions. Health Educ Res. 1988;3(3):273–82.
Hansen PE, Siersma V, Ross L, Mortensen EL, Riegels M, Tjørnhøj-Thomsen T, et al. Psychometric properties of brief indexes designed to measure social-cognitive predictors of smoking initiation. Drug Alcohol Depend. 2007;88(1):64–74.
Champion VL, Scott CR. Reliability and validity of breast cancer screening belief scales in African American women. Nurs Res. 1997;46(6):331–7.
DiIorio C, Maibach E, O'Leary A, Sanderson CA, Celentano D. Measurement of condom use self-efficacy and outcome expectancies in a geographically diverse group of STD patients. AIDS Educ Prev. 1997;9(1).
Brafford LJ, Beck KH. Development and validation of a condom self-efficacy scale for college students. J Am Coll Heal. 1991;39(5):219–25.
van der Bijl J. Van Poelgeest-Eeltink, Shortridge-Baggett L. the psychometric properties of the diabetes management self-efficacy scale for patients with type 2 diabetes mellitus. J Adv Nurs. 1999;30(2):352–9.
Shortridge-Baggett LM. Self-efficacy: measurement and intervention in nursing. Sch Inq Nurs Pract. 2001;15(3):183–8.
Shieh C, Weaver MT, Hanna KM, Newsome K, Mogos M. Association of self-efficacy and self-regulation with nutrition and exercise behaviors in a community sample of adults. J Community Health Nurs. 2015;32(4):199–211.
Stephens JD, Althouse A, Tan A, Melnyk BM. The role of race and gender in nutrition habits and self-efficacy: results from the young adult weight loss study. J Obes. 2017;2017.
Reumkens K, Tummers MH, Gietel-Habets JJ, van Kuijk SM, Aalfs CM, van Asperen CJ, et al. Online decision support for persons having a genetic predisposition to cancer and their partners during reproductive decision-making. J Genet Couns. 2018;28(3):533–42.
Scaffidi RM, Posmontier B, Bloch JR, Wittmann-Price R. The relationship between personal knowledge and decision self-efficacy in choosing trial of labor after cesarean. J Midwifery Womens Health. 2014;59(3):246–53. https://doi.org/10.1111/jmwh.12173.
Hall AK, Bernhardt JM, Dodd V. Older adults’ use of online and offline sources of health information and constructs of reliance and self-efficacy for medical decision making. J Health Commun. 2015;20(7):751–8. https://doi.org/10.1080/10810730.2015.1018603.
Nahm E-S, Zhu S, Bellantoni M, Keldsen L, Russomanno V, Rietschel M, et al. The effects of a theory-based patient portal e-learning program for older adults with chronic illnesses. Telemed J E Health. 2018. https://doi.org/10.1089/tmj.2018.0184.
Arterburn DE, Westbrook EO, Bogart TA, Sepucha KR, Bock SN, Weppner WG. Randomized trial of a video-based patient decision aid for bariatric surgery. Obesity. 2011;19(8):1669–75.
O’Brien M, Crickard E, Lee J, Holmes C. Attitudes and experience of youth and their parents with psychiatric medication and relationship to self-reported adherence. Community Ment Health J. 2013;49(5):567–75.
Peek ME, Harmon SA, Scott SJ, Eder M, Roberson TS, Tang H, et al. Culturally tailoring patient education and communication skills training to empower African-Americans with diabetes. Transl Behav Med. 2012;2(3):296–308. https://doi.org/10.1007/s13142-012-0125-8.
Bailey RA, Pfeifer M, Shillington AC, Harshaw Q, Funnell MM, VanWingen J, et al. Effect of a patient decision aid (PDA) for type 2 diabetes on knowledge, decisional self-efficacy, and decisional conflict. BMC Health Serv Res. 2016;16(1):10. https://doi.org/10.1186/s12913-016-1262-4.
Bailey RA, Shillington AC, Harshaw Q, Funnell MM, VanWingen J, Col N. Changing patients’ treatment preferences and values with a decision aid for type 2 diabetes mellitus: results from the treatment arm of a randomized controlled trial. Diabetes Ther. 2018;9(2):803–14. https://doi.org/10.1007/s13300-018-0391-7.
Chen NH, Lin YP, Liang SY, Tung HH, Tsay SL, Wang TJ. Conflict when making decisions about dialysis modality. J Clin Nurs. 2018;27(1–2):e138–e46.
Belkora J, Stupar L, O’Donnell S, Loucks A, Moore D, Jupiter C, et al. Decision support by telephone: randomized controlled trial in a rural community setting. Patient Educ Couns. 2012;89(1):134–42.
Shepherd SC, Hacking B, Wallace LM, Murdoch SE, Belkora J. Randomised controlled trial of a repeated consultation support intervention for patients with colorectal cancer. Psycho-Oncology. 2018.
Braun KL, Fong M, Kaanoi ME, Kamaka ML, Gotay CC. Testing a culturally appropriate, theory-based intervention to improve colorectal cancer screening among native Hawaiians. Prev Med. 2005;40(6):619–27.
Frosch DL, Kaplan RM, Felitti V. The evaluation of two methods to facilitate shared decision making for men considering the prostate-specific antigen test. J Gen Intern Med. 2001;16(6):391–8.
McCormack L, Treiman K, Bann C, Williams-Piehota P, Driscoll D, Poehlman J, et al. Translating medical evidence to promote informed health care decisions. Health Serv Res. 2011;46(4):1200–23.
Wray RJ, Vijaykumar S, Jupka K, Zellin S, Shahid M. Addressing the challenge of informed decision making in prostate cancer community outreach to African American men. Am J Mens Health. 2011;5(6):508–16.
Holt C, Wynn TA, Litaker MS, Southward P, Jeames SE, Schulz EK. A comparison of a spiritually based and non-spiritually based educational intervention for informed decision making for prostate cancer screening among church-attending African-American men. Urol Nurs. 2009;29(4):249–58.
Holmes-Rovner M, Kroll J, Schmitt N, Rovner DR, Breer ML, Rothert ML, et al. Patient satisfaction with health care decisions: the satisfaction with decision scale. Med Decis Mak. 1996;16(1):58–64. https://doi.org/10.1177/0272989x9601600114.
Gattellari M, Ward JE. Does evidence-based information about screening for prostate cancer enhance consumer decision-making? A randomised controlled trial. J Med Screen. 2003;10(1):27–39. https://doi.org/10.1258/096914103321610789.
Bunn H, O'Connor A. Validation of client decision-making instruments in the context of psychiatry. Can J Nurs Res. 1996;28(3):13–27.
Sultan DH, Rivers BM, Osongo BO, Wilson DS, Schenck A, Carvajal R, et al. Affecting African American men’s prostate cancer screening decision-making through a mobile tablet-mediated intervention. J Health Care Poor Underserved. 2014;25(3):1262–77.
Dickey SL, Whitmore A, Campbell E. The relation among prostate cancer knowledge and psychosocial factors for prostate cancer screening among African American men: a correlational study. AIMS public health. 2017;4(5):446–65.
Pearson RH, Mundform DJ. Recommended sample size for conducting exploratory factor analysis on dichotomous data. J Mod Appl Stat Methods. 2010;9(2):5.
Comrey AL, Lee HB. A first course in factor analysis. 1992.
Osborne JW, Costello AB, Kellow JT. Best practices in exploratory factor analysis. Best Practices in Quantitative Methods. 2008:86–99.
Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55.
Spiliotopoulou G. Reliability reconsidered: Cronbach’s alpha and paediatric assessment in occupational therapy. Aust Occup Ther J. 2009;56(3):150–5.
Levine RS, Foster JE, Fullilove RE, Fullilove MT, Briggs NC, Hull PC, et al. Black–white inequalities in mortality and life expectancy, 1933–1999: implications for healthy people 2010. Public Health Rep. 2016.
Gökce MI, Wang X, Frost J, Roberson P, Volk RJ, Brooks D, et al. Informed decision making before prostate-specific antigen screening: initial results using the American Cancer Society (ACS) decision aid (DA) among medically underserved men. Cancer. 2017;123(4):583–91. https://doi.org/10.1002/cncr.30367.
Orom H, Underwood W 3rd, Homish DL, Kiviniemi MT, Homish GG, Nelson CJ, et al. Prostate cancer survivors’ beliefs about screening and treatment decision-making experiences in an era of controversy. Psychooncology. 2015;24(9):1073–9. https://doi.org/10.1002/pon.3721.
Diefenbach MA, Mohamed NE. Regret of treatment decision and its association with disease-specific quality of life following prostate cancer treatment. Cancer Investig. 2007;25(6):449–57.
Owens OL, Tavakoli AS, Rose T, Wooten NR. Development and psychometric properties of a prostate cancer knowledge scale for African American men. Am J Mens Health. 2019; In Press.
Cormier L, Kwan L, Reid K, Litwin MS. Knowledge and beliefs among brothers and sons of men with prostate cancer. Urology. 2002;59(6):895–900.
Owens OL, Wooten NR, Tavakoli AS. Development and initial psychometric evaluation of the computer-based prostate cancer screening decision aid acceptance scale for African-American men. BMC Med Res Methodol. 2019; In Press.
Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Q. 2003:425–78.
Hubley AM. Discriminant validity. In: Michalos AC, editor. Encyclopedia of quality of life and well-being research. Dordrecht: Springer Netherlands; 2014. p. 1664–7.
Chin C-L, Yao G. Convergent validity. In: Michalos AC, editor. Encyclopedia of quality of life and well-being research. Dordrecht: Springer Netherlands; 2014. p. 1275–6.
Brown TA. Confirmatory factor analysis for applied research. New York, NY: Guilford Press; 2006.
Harrington D. Confirmatory factor analysis. Oxford University Press. USA; 2008.
Kline R. Principles and practice of structural equation modeling. 2nd ed. New York, NY: Guilford Press; 2005.
Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10(7):1–9.
Schmitt TA, Sass DA. Rotation criteria and hypothesis testing for exploratory factor analysis: implications for factor pattern loadings and interfactor correlations. Educ Psychol Meas. 2011;71(1):95–113.
Velicer WF, Eaton CA, Fava JL. Construct explication through factor or component analysis: a review and evaluation of alternative procedures for determining the number of factors or components. Problems and solutions in human assessment. Springer; 2000. p. 41–71.
Zwick WR, Velicer WF. Comparison of five rules for determining the number of components to retain. Psychol Bull. 1986;99(3):432.
Çokluk Ö, Koçak D. Using Horn’s parallel analysis method in exploratory factor analysis for determining the number of factors. Educational Sciences: Theory and Practice. 2016;16(2):537–51.
Hayton JC, Allen DG, Scarpello V. Factor retention decisions in exploratory factor analysis: a tutorial on parallel analysis. Organ Res Methods. 2004;7(2):191–205.
Shultz K, Whitney D, Zickar M. Measurement theory in action: case studies and exercises: Routledge; 2013.
Hooper D, Coughlan J, Mullen M. Structural equation modelling: guidelines for determining model fit. Electron J Bus Res Methods. 2008;6(1):53–60.
Williams B, Onsman A, Brown T. Exploratory factor analysis: a five-step guide for novices. Australasian Journal of Paramedicine. 2010;8(3).
Siegel R, Miller K, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30. https://doi.org/10.3322/caac.21442.
Powell IJ, Dyson G, Land S, Ruterbusch J, Bock CH, Lenk S, et al. Genes associated with prostate cancer are differentially expressed in African American and European American men. Cancer Epidemiol Biomark Prev. 2013;22(3):891–7.
Powell IJ, Bock CH, Ruterbusch JJ, Sakr W. Evidence supports a faster growth rate and/or earlier transformation to clinically significant prostate cancer in black than in white American men, and influences racial progression and mortality disparity. J Urol. 2010;183(5):1792–7.
Mahal BA, Chen MH, Bennett CL, Kattan MW, Sartor O, Stein K, et al. The association between race and treatment regret among men with recurrent prostate cancer. Prostate Cancer Prostatic Dis. 2015;18(1):38–42. https://doi.org/10.1038/pcan.2014.42.
Loeb S, Bjurlin MA, Nicholson J, Tammela TL, Penson DF, Carter HB, et al. Overdiagnosis and overtreatment of prostate cancer. Eur Urol. 2014;65(6):1046–55.
Gökce M, Sundi D, Schaeffer E, Pettaway C. Is active surveillance a suitable option for African American men with prostate cancer? A systemic literature review. Prostate Cancer Prostatic Dis. 2017;20(2):127–36.
Collingwood SA, McBride RB, Leapman M, Hobbs AR, Kwon YS, Stensland KD et al., editors. Decisional regret after robotic-assisted laparoscopic prostatectomy is higher in African American men. Urologic Oncology: Seminars and Original Investigations; 2014: Elsevier.
Christie DR, Sharpley CF, Bitsika V. Why do patients regret their prostate cancer treatment? A systematic review of regret after treatment for localized prostate cancer. Psycho-Oncology. 2015;24(9):1002–11.
Morris BB, Farnan L, Song L, Addington EL, Chen RC, Nielsen ME, et al. Treatment decisional regret among men with prostate cancer: racial differences and influential factors in the North Carolina health access and prostate cancer treatment project (HCaP-NC). Cancer. 2015;121(12):2029–35. https://doi.org/10.1002/cncr.29309.
Davison BJ, So AI, Goldenberg SL. Quality of life, sexual function and decisional regret at 1 year after surgical treatment for localized prostate cancer. BJU Int. 2007;100(4):780–5.
Clark JA, Wray NP, Ashton CM. Living with treatment decisions: regrets and quality of life among men treated for metastatic prostate cancer. J Clin Oncol. 2001;19(1):72–80. https://doi.org/10.1200/jco.2001.19.1.72.
Acknowledgments
This study was funded by the University of South Carolina’s Office of the Vice President for Research and an American Cancer Society Institutional Research Grant from the University of South Carolina’s School of Pharmacy.
Author information
Authors and Affiliations
Contributions
Each author listed on the publication has contributed significantly to the conception, implementation, and analysis of the study and the production of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Research Involving Human Participants and/or Animals
This research involved the inclusion of human subjects. We certify that all procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board at the University of South Carolina (Pro00045407) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Owens, O.L., Wooten, N.R. & Tavakoli, A.S. Adaptation and Initial Psychometric Evaluation of an Informed Prostate Cancer Screening Decision Self-Efficacy Scale for African-American Men. J. Racial and Ethnic Health Disparities 7, 746–759 (2020). https://doi.org/10.1007/s40615-020-00702-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-020-00702-0