Abstract
Hispanics or Latinos residing in the USA are disproportionately affected by HIV when compared to whites. Health outcomes for Hispanics or Latinos diagnosed with HIV infection may vary by Hispanic or Latino subgroup. We analyzed national mortality data from the National Center for Health Statistics for the years 2006 to 2010 to examine differences in HIV-related mortality among Hispanics or Latinos by sociodemographic factors and by Hispanic or Latino subgroup. After adjusting for age, HIV-related death rates per 100,000 population were highest among Hispanics or Latinos who were male (45.6, 95 % confidence interval [CI], 44.4 to 46.9) compared to female (12.0, 95 % CI 11.4 to 12.6), or resided in the Northeast (75.1, 95 % CI 72.2 to 77.9) compared to other US regions at the time of death. The age-adjusted HIV-related death rate was highest among Puerto Ricans (100.9, 95 % CI 97.0 to 104.8) and lowest among Mexicans (16.9, 95 % CI 16.2 to 17.6). Among all deaths, the proportion of HIV-related deaths was more than four times as high among Puerto Ricans (adjusted prevalence ratio = 4.3, 95 % CI 4.1 to 4.5) compared to Mexicans. To ensure better health outcomes for Hispanics or Latinos living with HIV in the USA, medical care and treatment programs should be adapted to address the needs of various Hispanic or Latino subgroups.
Similar content being viewed by others
Introduction
Hispanics or Latinos in the USA benefit from higher overall life expectancies than certain racial/ethnic groups. In 2011, Hispanics or Latinos had a higher life expectancy compared to blacks or African Americans (hereafter referred to as blacks) and whites [1]. Both Hispanic or Latino females and males also had higher life expectancies (83.1 and 77.9 years, respectively) than white females or males (80.5 and 75.6 years, respectively) or black females or males (76.3 and 69.3, respectively), and at most ages [1, 2]. Life expectancy advantages are not however, maintained for Hispanics or Latinos diagnosed with HIV infection, who suffer greater morbidity and mortality than whites [3, 4]. In 2009, HIV ranked 17th among the leading causes of death for Hispanics or Latinos, 20th for all persons who were not Hispanic or Latino, and 25th for whites [2, 5]. During 2010, the estimated death rate among Hispanic or Latino adults and adolescents diagnosed with HIV infection was more than two times the rate for whites [6].
Previous reports involving national HIV surveillance data have substantiated disparities in diagnoses of HIV infection between HIV-infected Hispanics or Latinos and whites [7–10]. For HIV-infected Hispanics or Latinos living in the USA, disparities exist for diagnoses of HIV infection, early diagnosis, and achievement of viral suppression. During 2011, Hispanics or Latinos had the second highest rates of newly diagnosed HIV infections (19.5 per 100,000 population) and stage 3 (AIDS) classifications (16.2), both of which were nearly three times the rates for whites (7.0 and 4.9, respectively) [6, 11]. Hispanics or Latinos accounted for 21 % of persons aged 13 and older in the USA newly diagnosed with HIV infection in 2011, despite comprising only 17 % of the population [11]. Similar differences exist for new HIV infections (HIV incidence)—in 2010, the rate of new HIV infections for Hispanics or Latinos (27.5 per 100,000 population) was more than three times the rate for whites (8.7) [12].
HIV burden for Hispanics or Latinos extends beyond diagnosed infections, as many remain undiagnosed and unaware of their HIV infection. Compared to other racial/ethnic groups, the estimated prevalence of undiagnosed HIV among Hispanics or Latinos is relatively high. At the end of 2008, the prevalence rate for undiagnosed HIV infection among Hispanic or Latino males (897.3 per 100,000 population) was two times that of white males (419.4), and the rate for Hispanic or Latino females (263.1) was four times the rate for white females (66.4) [7]. Further, Hispanics or Latinos who learn of their HIV infection may be diagnosed at later stages [11]. During 2010, among adults and adolescents in 14 national HIV surveillance jurisdictions who were newly diagnosed with HIV, 31 % of Hispanics or Latinos were diagnosed with stage 3 infection (AIDS) as compared to 24 % of blacks and 25 % of whites [13]. Even after engagement in medical care and prescription of antiretroviral therapy, HIV-infected Hispanics or Latinos may still be less likely to achieve viral suppression than whites [10, 13, 14]. Other research has shown that HIV-infected Hispanics or Latinos with late initiation and early discontinuation of antiretroviral therapy have greater losses in years of life than other racial/ethnic groups [15].
Geographic region of residence, place of birth, and Hispanic origin are important factors contributing to differences in HIV diagnosis rates and HIV-related outcomes for Hispanics or Latinos in the USA. In 2010, Hispanics or Latinos residing in the Northeast had a higher HIV diagnosis rate and a higher HIV prevalence than those residing in other regions of the USA [16]. Several studies have shown higher percentages of diagnosed HIV infection and/or worse health outcomes for Puerto Ricans diagnosed with HIV, which may be influenced by the greater likelihood for Puerto Rican-born Hispanics or Latinos to have HIV attributable to injection drug use (IDU) than Hispanics or Latinos born elsewhere [6, 16, 17]. Similar disparities have been reported for HIV-related deaths. Results from a 2002 analysis of HIV-related deaths among Hispanic or Latino subgroups showed Puerto Ricans as having a higher rate compared to other Hispanics or Latinos (i.e., Cubans, Mexicans, South/Central Americans, and other/unknown subgroups), with Puerto Ricans in the Northeast and Midwest regions of the USA having even higher HIV-related death rates than those of non-Hispanic blacks [18]. Additional studies have shown Mexican- or Central American-born Hispanics or Latinos diagnosed with HIV to experience better survival than those belonging to other subgroups [19].
Higher prevalence rates of undiagnosed HIV infection, higher percentages of late-stage diagnoses, and a lesser likelihood of achieving viral suppression could lead to higher HIV-related death rates for Hispanics or Latinos compared to whites. The goals of this analysis were to examine HIV-related death rates and the proportion of HIV-related deaths among all deaths that occurred during 2006 to 2010 for Hispanics or Latinos in the USA compared to other racial/ethnic groups and to assess whether Hispanic or Latino subgroups or other sociodemographic factors (age, sex, birth origin, geographic region of residence) contributed to the proportion of HIV-related death among all deaths for Hispanics or Latinos.
Methods
We analyzed vital statistics data from the National Center for Health Statistics for deaths occurring during 2006 to 2010 in adults and adolescents aged 18 and older who resided in the USA and for whom Hispanic or Latino ethnic origin had been reported on the death certificate [20]. A death was considered HIV related if an HIV-related illness was listed as a primary or other (non-primary) cause of death on the death certificate using ICD-10 codes [21]. We calculated crude (unadjusted) and age-adjusted HIV-related death rates for blacks, Hispanics or Latinos, whites, and other racial/ethnic groups (includes American Indians/Alaska Natives, Asians, and Native Hawaiians/other Pacific Islanders), and for Hispanics or Latinos by age group, sex, Hispanic or Latino subgroup, and US region of residence at the time of death. For death data, other Hispanic or Latino subgroup was comprised of deaths among persons who identified as Spaniard, Latin American, or other Hispanic or Latino with no further geographical specification. For unadjusted rates, we divided the number of HIV-related deaths for each group by the group population, per 100,000. We calculated population denominators using data from the Selected Population Tables of the American Community Survey (ACS) for 2006 to 2010 (i.e., 5-year estimates) [22]. The ACS is conducted in counties in the USA, has a coverage rate greater than 90 % for Hispanics or Latinos, and includes estimated population data for Hispanic or Latino subgroups (i.e., Cuban, Dominican, Mexican, Puerto Rican, South or Central American, and other subgroups [includes persons who identified as Spaniard or other Hispanic or Latino with no further geographical specification]). To control for potential confounding due to differences in the age distributions between racial/ethnic groups or between groups of Hispanics or Latinos, we calculated age-adjustment weights from the 2010 United States Census data for persons aged 18 and older and calculated age-adjusted HIV-related death rates using direct standardization to the 2010 United States Census population [23, 24]. We generated 95 % confidence intervals for crude and adjusted HIV-related death rates to allow for the comparison of rates [23]. To evaluate differences in HIV-related deaths among all deaths for Hispanics or Latinos by age and other socio-demographic factors, we calculated the median age at death for both HIV-related and all-cause deaths by Hispanic or Latino subgroup, as well as prevalence ratios and adjusted prevalence ratios (controlling for age) by age group, sex, Hispanic or Latino subgroup, and US region of residence at the time of death. To calculate prevalence ratios, we divided the proportion of HIV-related deaths (among all-cause deaths) for the group of interest by the proportion of HIV-related deaths (among all-cause deaths) for the reference group. For adjusted prevalence ratios, we performed a univariate binomial regression analysis, controlling for age [25]. We calculated 95 % confidence intervals for prevalence ratios and adjusted prevalence ratios to allow for the comparison of ratios.
Results
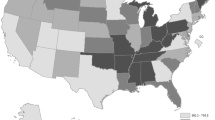
From 2006 to 2010, 58,707 HIV-related deaths were reported for adults and adolescents aged 18 and older who were residing in the USA; 7,728 of these deaths (13.2 %) were among Hispanics or Latinos. Both crude and age-adjusted HIV-related death rates (per 100,000 population) were highest for blacks (121.2, 95 % confidence interval [CI], 119.9 to 122.5 and 122.2, 95%CI 120.9 to 123.6, respectively) followed by Hispanics or Latinos (24.6, 95 % CI 24.1 to 25.2 and 28.3, 95 % CI 27.6 to 29.0, respectively), whites (11.5, 95 % CI 11.3 to 11.7 and 11.2, 95 % CI 11.0 to 11.4, respectively), and persons belonging to other racial/ethnic groups (6.1, 95 % CI 5.7 to 6.5 and 6.2, 95 % CI 5.8 to 6.6, respectively) (Fig. 1). Age-adjusted HIV-related death rates for Hispanics or Latinos were more than two times the rate of whites and nearly five times the rate of other racial/ethnic groups. Among Hispanics or Latinos, within each corresponding factor, unadjusted HIV-related death rates (per 100,000 population) were highest for Hispanics or Latinos who were 45–54 years old (53.6, 95 % CI 51.6 to 55.6), male (38.0, 95 % CI 37.0 to 38.9), Puerto Rican (91.0, 95 % CI 87.5 to 94.4), or resided in the Northeast at the time of death (64.4, 95 % CI 62.1 to 66.8) (Table 1). After adjusting for age, HIV-related death rates remained highest among Hispanics or Latinos who were male (45.6, 95 % CI 44.4 to 46.9), Puerto Rican (100.9, 95 % CI 97.0 to 104.8), or resided in the Northeast at the time of death (75.1, 95 % CI 72.2 to 77.9) (Table 1, Fig. 2).
Adjusted HIV-related death rates for persons (≥18 years) residing in the USA, by race/ethnicity—2006–2010. Death rates include deaths with a primary or other cause of death due to HIV infection or related conditions, as indicated by ICD 10 codes. Rates are per 100,000 population. Population denominators were calculated using the American Community Survey selected population tables for 2006–2010. Rates were adjusted for age using weights derived from the United States Census 2010 (available at: http://www.census.gov/popest/data/intercensal/national/nat2010.html). “USA” includes persons residing in the USA at the time of death; excludes US territories. Hispanics or Latinos can be of any race. Other race/ethnicity includes American Indians/Alaska Natives, Asians, and Native Hawaiians/other Pacific Islanders
Adjusted HIV-related death rates for Hispanics or Latinos (≥18 years) residing in the USA, by Hispanic or Latino subgroup—2006–2010. Death rates include deaths with a primary or other cause of death due to HIV infection or related conditions, as indicated by ICD 10 codes. Rates are per 100,000 population. Population denominators were calculated using the American Community Survey selected population tables for 2006–2010. Rates were adjusted for age using weights derived from the United States Census 2010 (available at: http://www.census.gov/popest/data/intercensal/national/nat2010.html). Hispanics or Latinos can be of any race. “USA” includes persons residing in the USA at the time of death; excludes US territories. Other subgroup includes Latin Americans (1.7 % of all deaths), Spaniards (4.1 % of all deaths), and Hispanic or Latino subgroups with no geographical specification (94.2 % of deaths)
Among Hispanics or Latinos, the median age at death was 46 years for those who died of HIV-related causes and 71 years for all causes. Among Hispanic or Latino subgroups, the median age at HIV-related death ranged from 42 (South/Central Americans) to 52 years (Cubans) (Fig. 3). Within each corresponding factor, the largest percentage of Hispanics or Latinos with HIV-related deaths was among those who were 45–54 years old (35 %), male (78 %), Mexican (37 %), and residents of the Northeast region of the USA at the time of death (38 %) (Tables 1 and 2).
Median age at death for Hispanics or Latinos (≥18 years) residing in the USA, by Hispanic or Latino subgroup and cause of death—2006–2010. Hispanics or Latinos can be of any race. “USA” includes persons residing in the USA at the time of death; excludes US territories. HIV-related causes include deaths with a primary or other cause of death due to HIV infection or related conditions, as indicated by ICD 10 codes. Other subgroup includes Latin Americans (1.7 % of all deaths), Spaniards (4.1 % of all deaths), and Hispanic or Latino subgroups with no geographical specification (94.2 % of deaths)
Compared to Hispanics or Latinos who died (decedents) at 45–54 years old, the proportion of HIV-related death among all deaths was significantly higher among 35–44 year old Hispanic or Latino decedents (prevalence ratio [PR] = 1.5, 95 % CI 1.4 to 1.6) and significantly lower for all other age groups (Table 2). After controlling for age, the proportion of HIV-related deaths among all deaths was significantly lower among female than male Hispanic or Latino decedents (adjusted prevalence ratio [APR] = 0.5, 95 % CI 0.5 to 0.6) and among Hispanic or Latino decedents who resided in the South (APR = 0.4, 95 % CI 0.3 to 0.4), West (APR = 0.2, 95 % CI 0.2 to 0.3), or Midwest (APR 0.2, 95 % CI 0.2 to 0.3) than in the Northeast. Among all deaths, the proportion of HIV-related deaths was significantly higher for all Hispanic or Latino subgroups compared to Mexicans, with Puerto Ricans having the highest adjusted prevalence ratio (APR = 4.3, 95 % CI 4.1 to 4.5) (Table 1).
Discussion
Our analysis focused specifically on Hispanics or Latinos in the USA with HIV-related illness as a cause of death and revealed disparities in HIV-related death for Hispanics or Latinos and blacks compared to whites and other racial/ethnic groups. Other studies have identified high all-cause death rates or low survival rates for Hispanics or Latinos diagnosed with HIV infection compared to whites [6, 15, 19]. Among Hispanics or Latinos, we discovered disparities for both HIV-related death rates and the proportion of HIV-related deaths (among all deaths) by age group, sex, Hispanic or Latino subgroup, and region of residence. For Hispanic or Latino subgroups, differences in HIV-related death rates and in the proportion of HIV-related deaths (among all deaths) were most pronounced between Puerto Ricans and Mexicans. By standardizing crude HIV-related death rates to the age distribution of the US 2010 population for persons 18 years and older, we were able to make comparisons between Hispanics or Latinos and other racial/ethnic groups, and between groups of Hispanics or Latinos without the potentially confounding effects of age. Hispanics or Latinos included in our population denominator were younger than the standard population—67 % of Hispanics or Latinos were 18–44 years old, compared to 49 % in the standard population [24]. After adjusting for age, the HIV-related death rate for Puerto Ricans was approximately six times the rate of Mexicans. Also, among all deaths, the proportion of HIV-related deaths was four times as high among Puerto Ricans as among Mexicans. Although our analysis focused primarily on Hispanic or Latino populations, the greatest disparity in HIV-related death rates was for blacks, who had approximately five times the rate of Hispanics or Latinos, 11 times the rate of whites, and 20 times the rate of other racial ethnic groups.
Our analysis of HIV-related mortality is consistent with a previous analysis of national mortality data from 1996 to 2000, which found Puerto Ricans to have the highest age-adjusted HIV-related death rate overall, by sex, and by geographic region compared to other Hispanic or Latino subgroups [18]. Other studies have shown HIV-positive Hispanics or Latinos born in Puerto Rico to have greater risk of HIV-related death or worse survival than persons born in the continental USA [19]. Factors contributing to this disparity may include risk-taking behaviors or medication adherence issues. For example, for diagnoses of HIV infection among adults and adolescents during 2011, the percentages of both males and females with HIV attributable to injecting drugs were highest among persons born in Puerto Rico (males, 23 %; females, 17 %) versus Central America, Cuba, Mexico, or South America [6]. This population also had a higher percentage of HIV infection stage 3 (AIDS) diagnoses (males, 33 %; females, 19 %) than persons from other Latin countries [6]. Further, Hispanic or Latino men born in Puerto Rico are more likely to have HIV infection attributable to injecting drugs compared to Hispanics or Latinos born in other Latin American countries, who are more likely to have HIV attributable to sexual contact [6, 17, 26]. Injecting drugs could serve as a barrier to accessing medical care or adhering to antiretroviral therapy, which could in turn affect HIV-related morbidity and mortality. We did not assess HIV risk behaviors, as national mortality data do not include this information for decedents. Additional research is needed to further examine the link between HIV-related mortality and HIV risk behaviors for various Hispanic or Latino subgroups and to provide information for tailoring programs aimed at improving the continuum of care, especially for Hispanics or Latinos who may be injecting drugs or other substances and at higher risk for non-adherence to antiretroviral medication and/or medical care [27].
Previous research on mortality among Hispanics or Latinos residing in the USA has identified reverse migration—the return of foreign-born Hispanics or Latinos to their country of birth after developing a serious illness—as a factor that may contribute to lower national death rates for certain Hispanic or Latino subgroups [28]. For example, political climate may serve as a barrier to emigration for Cubans, but not necessarily for Mexicans [28]. In our analysis, Mexicans had a lower HIV-related death rate and a lower proportion of HIV-related deaths (among all-cause deaths) than all other Hispanic or Latino subgroups. Reverse migration may have contributed to this outcome, especially for foreign-born Mexicans. Puerto Ricans residing in the USA or its dependencies are included in national mortality data and are not considered to contribute to the reverse migration effect. However, we excluded data from Puerto Rico and other US dependencies due to the unavailability of Hispanic or Latino subgroup data or population denominators. During 2011, the metropolitan statistical area of San Juan-Caguas-Guaynabo, Puerto Rico had the third highest all-cause death rate for adults and adolescents diagnosed with HIV [29]. Additional research is needed to examine deaths due to HIV-related illness specifically among Hispanics or Latinos residing in Puerto Rico. In addition to migration patterns, socioeconomic factors may also play a role in differences in HIV-related deaths among Hispanic or Latino subgroups. Cubans residing in the USA have reported higher levels of educational attainment and income than other Hispanic or Latino subgroups, and thus may benefit from better healthcare access and higher health literacy, which could in turn lead to better HIV-related health outcomes [30].
Data from previous studies have shown HIV-infected Hispanics or Latinos in the USA to consistently present to care later than whites and with more advanced HIV disease [19]. Recently published data on Medicaid enrollees in the southern USA showed Hispanic or Latino enrollees as receiving less optimal care and being less likely to receive antiretroviral therapy than both blacks and whites [31, 32]. Our analysis did not assess receipt of medical care and/or antiretroviral therapy among decedents; however, our results showed higher age-adjusted rates for death due specifically to HIV-related illnesses for Hispanics or Latinos compared to whites, which could be the result of delayed diagnosis of HIV infection and/or access to medical care and treatment. Our analysis did not examine acculturation, interactions between place of birth and Hispanic or Latino subgroup, HIV risk behaviors, or access to HIV testing and treatment (which could influence the time of diagnosis [i.e., early versus delayed] and health outcomes). Further research is needed to examine the factors that may contribute to HIV-related death among Hispanics or Latinos.
During 2010, Hispanics or Latinos residing in the Midwestern USA had the lowest HIV diagnosis rate (per 100,000 population) (19.2) and the second lowest HIV prevalence rate (per 100,000 population) (293.5) compared to other regions [16]. Our analysis revealed similar results for HIV-related death among Hispanics or Latinos in the Midwest, who had the lowest crude HIV-related death rate (per 100,000 population; 12.4, 95 % CI 11.1 to 13.7) and for whom the proportion of HIV-related death among all deaths was significantly lower when compared to Hispanics or Latinos residing in the Northeast (APR = 0.2, 95 % CI 0.2 to 0.3). Our results are consistent with previous analyses that have demonstrated similar regional differences, with Hispanic or Latino residents of the Northeast having a higher rate of HIV-related death and a higher HIV prevalence rate than Hispanic or Latino residents of other areas in the USA [16, 18]. The higher death rate and prevalence ratio among Hispanics or Latinos residing in the Northeast may be explained by Puerto Ricans, who are both more likely to reside in the Northeastern region of the USA than in other regions and to have HIV attributable to injecting drugs [6, 16, 33]. Our results are also consistent with the health and socioeconomic status of Hispanics or Latinos residing in the Midwest, who have higher percentages of health insurance coverage and less poverty than Hispanics or Latinos in the USA, overall [34].
There are several limitations associated with this analysis. The number of HIV-related deaths for Hispanics or Latinos may be underestimated due to incomplete reporting of Hispanic ethnicity on death certificates. In 2008, the ACS changed the layout of the question for Hispanic or Latino origin from a grid format to a sequential layout and saw increased reporting for Hispanics or Latinos overall, as well as a lower nonresponse rate for the Hispanic origin question. Our analysis focused on the years 2006 to 2010; thus, our population estimates for Hispanics or Latinos could be slightly underestimated due to the data that were collected prior to 2008 using the previous method [35]. For age-adjustment, we applied weights derived from the 2010 United States Census, which differs from the time period for our study population (2006 to 2010). Any HIV-related deaths in which HIV was not mentioned as a cause of death on the death certificate were not captured in this analysis; therefore, we may have underestimated HIV-related mortality and the proportion of HIV-related deaths among all deaths during 2006 to 2010. Finally, despite differences in both HIV-related outcomes and socioeconomic status, we were unable to analyze data separately for Central Americans and South Americans. South Americans have been shown to have better survival following an HIV diagnosis and higher socioeconomic status than Central Americans [30, 36].
In 2009, Hispanics or Latinos with diagnosed HIV infection were less likely than whites to have been prescribed antiretroviral therapy or to have achieved viral suppression [10]. Results from our analysis may be used to inform HIV treatment programs for Hispanics or Latinos residing in the USA and to target specific Hispanic or Latino subgroups for continued access to and engagement and maintenance in HIV-related medical care, with the ultimate goal of reducing HIV-related mortality. The proportion of HIV-related death among all deaths was significantly higher among Puerto Ricans than Mexicans. In 2010, Puerto Ricans comprised the second largest percentage (9 %) of Hispanic or Latino subgroups (i.e., Mexicans, Puerto Ricans, Cubans, Dominicans, South Americans, Central Americans, and other Hispanics or Latinos) residing in the USA [33]. As Hispanic or Latino populations in the USA continue to grow, interventions or programs that focus on engagement and maintenance in HIV medical care and/or adherence to antiretroviral therapy must be tailored to address the needs of Hispanics or Latinos living with HIV disease. For Puerto Ricans, who are more likely than other Hispanic or Latino subgroups to have HIV attributable to injecting drugs, such programs may need to incorporate substance abuse counseling and/or treatment or harm-reduction approaches [6, 16, 17, 29]. Effective HIV prevention interventions for reducing sexual or drug risk behaviors among Hispanics or Latinos have addressed gender norms, used non-peers to deliver the intervention, and delivered the intervention in a setting other than outreach [37]. These characteristics, along with adherence-related barriers such as socioeconomic factors, acculturation, communication issues with providers, and fear of deportation (for those without US citizenship or legal residence status) should be considered as components of interventions aimed at improving the continuum of care for Hispanics or Latinos with HIV attributed to sexual or drug risk behaviors [27, 31, 32, 37–43].
The CDC prioritizes death ascertainment as one of the key activities for jurisdictions that collect and report HIV surveillance data. As the completeness of mortality and cause of death data continues to improve, more detailed analyses on the factors contributing to racial/ethnic disparities in HIV-related and other types of deaths for persons diagnosed with HIV in the USA will be possible.
References
Minino AM. Death in the United States. 2011. NCHS data brief, no 115. Hyattsville, MD: National Center for Health Statistics. March 2013. Available at: http://www.cdc.gov/nchs/data/databriefs/db115.htm. Accessed 6 Aug 2013.
Arias E. United States life tables by Hispanic origin. National Center for Health Statistics. Vital Health Stat 2010;2(152).
McDavid Harrison K, Song R, Zhang X. Life expectancy after HIV diagnosis based on national HIV surveillance data from 25 states, United States. J Acquir Immune Defic Syndr. 2010;53(1):124–30.
McGinnis KA, Fine MJ, Sharma RK, et al. Understanding racial disparities in HIV using data from the veterans aging cohort 3-site study and VA administrative data. Am J Public Health. 2003;93(10):1728–33.
Heron M. Deaths: Leading causes for 2009. National vital statistics reports; vol. 61 no 7. Hyattsville, MD: National Center for Health Statistics. October 26, 2012. Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_07.pdf. Accessed 28 Jun 2013.
CDC. HIV Surveillance Report, 2011; vol. 23. February 2013. Available at: http://www.cdc.gov/hiv/topics/surveillance/resources/reports/. Accessed 1 Aug 2103.
Chen M, Rhodes PH, Hall IH, Kilmarx PH, Branson BM, Valleroy LA. Prevalence of undiagnosed HIV infection among persons aged ≥13 years—National HIV Surveillance System, United States, 2005–2008. MMWR. 2012;61(02):57–64.
CDC. Disparities in diagnoses between blacks/African Americans and other racial/ethnic populations – 37 states, 2005–2008. MMWR. 2011;60(4):93–8.
CDC. Estimated lifetime risk for diagnosis of HIV infections among Hispanics/Latinos—37 states and Puerto Rico, 2007. MMWR. 2010;59(40):1297–301.
Satcher Johnson A, Beer L, Sionean C, et al. HIV infection—United States, 2008 and 2010. MMWR. 2013;62(3):112–9.
HIV surveillance—epidemiology of HIV infection (through 2011) [slide set]. February 2013. Available at: http://www.cdc.gov/hiv/library/slideSets/index.html. Accessed 1 Aug 2013.
CDC. Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report 2012;17(No. 4). December 2012. Available at: http://www.cdc.gov/hiv/topics/surveillance/resources/reports/#supplemental. Accessed 7 Jan 2013.
CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 U.S. dependent areas—2010. HIV Surveillance Supplemental Report 2013;18(No. 2, part B). January 2013. Available at: http://www.cdc.gov/hiv/topics/surveillance/resources/reports/#supplemental. Accessed 1 Aug 2013.
Hall IH, Frazier EL, Rhodes P, et al. Differences in human immunodeficiency virus care and treatment among subpopulations in the United States. JAMA Intern Med; Published online June 17, 2013. E1-E7.
Losina E, Schackman BR, Sadownik SN, et al. Racial and sex disparities in life expectancy losses among HIV-infected persons in the United States: impact of risk behavior, late initiation, and early discontinuation of antiretroviral therapy. Clin Infect Dis. 2009;49:1570–8.
CDC. Geographic differences in HIV infection among Hispanics or Latinos—46 states and Puerto Rico, 2010. MMWR. 2012;61(40):805–10.
Espinoza L, Hall HI, Selk RM, Hu X. Characteristics of HIV infection among Hispanics, United States 2003–2006. J Acquir Immune Defic Syndr. 2008;49(1):94–101.
Selik RM. Death due to HIV disease among Hispanics of different national origins, 2000 [Poster 912]. Presented at the 10th Conference on Retroviruses and Opportunistic Infections, 2003.
Chen NE, Gallant JE, Page KR. A systematic review of HIV/AIDS survival and delayed diagnosis among Hispanics in the United States. J Immigr Minor Health. 2012;14:65–81.
National Center for Health Statistics. Mortality—All County (2006–2010), as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program.
International Classification for Diseases, 10th Edition Medical Data Code Sets. Available at: http://www.cms.gov/Medicare/Coding/ICD10/index.html. Accessed 13 Aug 2013.
American Community Survey Office. The 2006–2010 ACS 5-year selected population tables summary file technical documentation. Data Products, Version 1. May 24, 2012. Available at: http://www2.census.gov/acs2010_SPT_AIAN/SelectedPopulationTables/ACS_SPT_SF_Tech_Doc.pdf. Accessed 21 Jun 2013.
National Center for Health Statistics. A guide to state implementation of ICD-10 for mortality. part ii: applying comparability ratios. December 4, 2000. Available at: http://www.cdc.gov/nchs/data/statab/Document%20for%20the%20States.pdf. Accessed 10 Jan 2014.
United States Census Bureau. Population estimates [entire data set]. Available at: http://www.census.gov/popest/data/intercensal/national/nat2010.html. Accessed 20 Aug 2013.
Petersen MR, Deddens JA. A comparison of two methods for estimating prevalence ratios. BMC Med Res Methodol. 2008;8:9.
Diaz VA. Hispanic male health disparities. Prim Care Clin Office Pract. 2006;33:45–60.
Gonzalez JS, Setsuko Hendriksen E, Collins EM, et al. Latinos and HIV/AIDS: examining factors related to disparity and identifying opportunities for psychosocial intervention research. AIDS Behav. 2009;13:582–602.
Fuller Thomson E, Nuru-Jeter A, Richardson D, Raza F, Minkler M. The Hispanic paradox and older adults’ disabilities: is there a healthy migrant effect? Int J Environ Res Public Health. 2013;10:1786–814.
CDC. Diagnosed HIV infection among adults and adolescents in metropolitan statistical areas—United States and Puerto Rico, 2011. HIV Surveillance Supplemental Report 2013;18(No. 8). October 2013. Available at: http://www.cdc.gov/hiv/library/reports/surveillance. Accessed 15 Nov 2013.
United States Census Bureau. Annual social and economic supplement to the Current Population Survey. Hispanic Population in the United States; 2010. Available at: http://www.census.gov/population/hispanic/data/2010.html. Accessed 25 Jun 2014.
Zhang S, Senteio C, Felizzola J, Rust G. Racial/Ethnic disparities in antiretroviral treatment among HIV-infected pregnant Medicaid enrollees, 2005–2007. Am J Public Health. 2013;103:e46–53.
Zhang S, McGoy SL, Dawes D, Fransua M, Rust G, Satcher D. The potential for elimination of racial-ethnic disparities in HIV treatment initiation in the medicaid population among 14 southern states. The potential for elimination of racial-ethnic disparities in HIV treatment initiation in the medicaid population among 14 southern states. PLoS ONE. 2014;9(4):e96148.
Ennis SR, Ríos-Vargas M, Albert NG. The Hispanic population. 2010 Census Briefs. May 2011. Available at: http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf. Accessed 20 Aug 2013.
Mendes de Leon CF, Eschbach K, Markides KS. Population trends and late-life disability in Hispanics from the Midwest. J Aging Health. 2011;23(7):1166–88.
United States Census Bureau. Effects of using a grid versus a sequential form on the ACS basic demographic data (final report). March 6, 2008. Available at: http://www.census.gov/acs/www/methodology/demographic_question/#latino. Accessed 20 Aug 2013.
Espinoza L, Hall IH, Hu X. Diagnoses of HIV infection among Hispanics/Latinos in 40 states and Puerto Rico, 2006–2009. J Acquir Immune Defic Syndr. 2012;60(2):205–13.
Herbst JH, Kay LS, Passin WF, et al. A systematic review and meta-analysis of behavioral interventions to reduce HIV risk behaviors of Hispanics in the United States and Puerto Rico. AIDS Behav. 2007;11:25–47.
Vissman AT, Hergenrather KC, Rojas G, Langdon SE, Wilkin AM, Rhodes SD. Applying the theory of planned behavior to explore HAART adherence among HIV-positive immigrant Latinos: elicitation interview results. Patient Educ Couns. 2011;85:454–60.
Zuniga ML, Munoz F, Kozo J, Blanco E, Scolari R. A binational study of patient-initiated changes to antiretroviral therapy regimen among HIV-positive Latinos living in the Mexico–U.S. border region. AIDS Behav. 2012;16:1622–9.
Oh DL, Sarafian F, Silvestre A, Brown T, Jacobson L, Badri S, et al. Evaluation of adherence and factors affecting adherence to combination antiretroviral therapy among white, Hispanic, and black men in the MACS cohort. J Acquir Immune Defic Syndr. 2009;52(2):290–3.
Robbins RN, D’Aquila E, Morgello S, et al. Cultural influences on antiretroviral therapy adherence among HIV-infected Puerto Ricans. JANAC. 2012;23(6):531–8.
Sanchez M, Rice E, Stein J, et al. Acculturation, coping styles, and health risk behaviors among HIV positive Latinas. AIDS Behav. 2010;14:401–9.
Cobos DG, Jones JW. Promoting passage through care: how best to serve undocumented immigrants with HIV. JANAC. 2008;19(4):320–4.
Acknowledgments
The authors would like to acknowledge Richard Selik, MD, of the Centers for Disease Control and Prevention for his significant contributions to the development of this research concept and for his publication of the original abstract from which this research concept was developed.
Conflicts of Interest
Authors Clark, Babu, Harris, and Hardnett declare that they have no conflicts of interest.
Ethical Standard Statements
No animal or human studies were carried out by the authors for this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Rights and permissions
About this article
Cite this article
Clark, H., Surendera Babu, A., Harris, S. et al. HIV-Related Mortality Among Adults (≥18 years) of Various Hispanic or Latino Subgroups—United States, 2006–2010. J. Racial and Ethnic Health Disparities 2, 53–61 (2015). https://doi.org/10.1007/s40615-014-0047-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-014-0047-x