Abstract
Background
Perioperative cerebral oxygen saturation (ScO2) has been reported to associate with postoperative delirium (POD) which is a common postoperative complication, however, the results were inconclusive. Therefore, we aimed to conduct an up-to-date review and meta-analyze the relationship between perioperative ScO2 and POD.
Methods
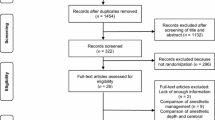
We systematically searched PubMed, Embase and Web of science through January 13, 2022. The pooled results were estimated through a random-effects model meta-analysis and expressed as odds ratios (ORs) and standard mean differences (SMDs), accompanied with 95% confident intervals (CIs).
Results
Finally, of 467 searched articles, ten articles were included. A total of six studies reported the baseline ScO2 value and the pooled result showed that preoperative baseline ScO2 was lower in POD groups (SMD = − 0.41, 95% CI − 0.64 to − 0.18). And beyond that, the pooled OR across four literatures about preoperative low ScO2 on POD was 3.44 (95% CI 1.69, 7.02). In contrast, insignificant differences were detected in baseline/lowest ScO2 value during intraoperative and postoperative period. Additionally, there were no statistically significant associations for intraoperative and postoperative low ScO2 effect on POD risk. Meta-regress analysis has found no significant impact factors.
Conclusions
Based on current evidence, POD patients have a lower ScO2, and ScO2 desaturation may increase POD incidence, indicating the role of ScO2 underlying pathological mechanisms. For generalizability of evidence, we should rely on high-quality, considering more comprehensively longitudinal, interdisciplinary studies.


Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Inouye SK, Westendorp RGJ, Saczynski JS (2014) Delirium in elderly people. Lancet 383:911–922
Djaiani G, Silverton N, Fedorko L et al (2016) Dexmedetomidine versus propofol sedation reduces delirium after cardiac surgery: a randomized controlled trial. Anesthesiology 124:362–368
Chang Y-L, Tsai Y-F, Lin P-J et al (2008) Prevalence and risk factors for postoperative delirium in a cardiovascular intensive care unit. Am J Crit Care 17:567–575
Eertmans W, De Deyne C, Genbrugge C et al (2020) Association between postoperative delirium and postoperative cerebral oxygen desaturation in older patients after cardiac surgery. Br J Anaesth 124:146–153
Wu J, Yin Y, Jin M et al (2021) The risk factors for postoperative delirium in adult patients after hip fracture surgery: a systematic review and meta-analysis. Int J Geriatr Psychiatry 36:3–14. https://doi.org/10.1002/gps.5408
Maldonado JR (2017) Acute brain failure: pathophysiology, diagnosis, management, and sequelae of delirium. Critical Care Clin 33:461–519
Tilley E, Psaltis PJ, Loetscher T et al (2018) Meta-analysis of prevalence and risk factors for delirium after transcatheter aortic valve Implantation. Am J Cardiol 122:1917–1923
Oe S, Daisuke Togawa Yu, Yamato TH et al (2019) Preoperative age and prognostic nutritional index are useful factors for evaluating postoperative delirium among patients with adult spinal deformity. Spine 44:472–478
Thompson C, Brienza VJM, Sandre A et al (2018) Risk factors associated with acute in-hospital delirium for patients diagnosed with a hip fracture in the emergency department. CJEM 20:911–919
Morino T, Hino M, Yamaoka S et al (2018) Risk factors for delirium after spine surgery: an age-matched analysis. Asian Spine J 12:703–709
Tanak M, Tani N, Maruo T et al (2018) Risk factors for postoperative delirium after deep brain stimulation surgery for parkinson disease. World Neurosurgery 114:e518–e523
Fong TG, Bogardus ST Jr, Daftary A et al (2006) Cerebral perfusion changes in older delirious patients using 99mTc HMPAO SPECT. J Gerontol A Biol Sci Med Sci 61:1294–1299
Yu Y, Zhang K, Zhang L et al (2018) Cerebral near-infrared spectroscopy (NIRS) for perioperative monitoring of brain oxygenation in children and adults. Cochrane Database Syst Rev 1:Cd010947
Schenning KJ, Deiner SG (2015) Postoperative delirium in the geriatric patient. Anesthesiol Clin 33:505–516
Momeni M, Meyer S, Docquier M-A et al (2019) Predicting postoperative delirium and postoperative cognitive decline with combined intraoperative electroencephalogram monitoring and cerebral near-infrared spectroscopy in patients undergoing cardiac interventions. J Clin Monit Comput 33:999–1009
Clemmesen CG, Pedersen LM, Hougaard S et al (2018) Cerebral oximetry during preoperative resuscitation in elderly patients with hip fracture: a prospective observational study. J Clin Monit Comput 32:1033–1040
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. PLoS Med 6:e1000100. https://doi.org/10.1371/journal.pmed.1000100
McGrath S, Zhao X, Steele R et al (2020) Estimating the sample mean and standard deviation from commonly reported quantiles in meta-analysis. Stat Methods Med Res 29:2520–2537. https://doi.org/10.1177/0962280219889080
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F et al (2006) Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods 11:193–206
Di D, Zhang L, Xiaoxiao Wu et al (2020) Long-term exposure to outdoor air pollution and the risk of development of rheumatoid arthritis: a systematic review and meta-analysis. Semin Arthritis Rheum 50:266–275
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Sterne JA, Gavaghan D, Egger M (2000) Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol 53:1119–1129
Mailhot T, Cossette S, Lambert J et al (2016) Cerebral oximetry as a biomarker of postoperative delirium in cardiac surgery patients. J Critical Care 34:17–23
Schoen J, Meyerrose J, Paarmann H et al (2011) Preoperative regional cerebral oxygen saturation is a predictor of postoperative delirium in on-pump cardiac surgery patients: a prospective observational trial. Crit Care 15:R218
Schoen J, Meyerrose J, Paarmann H et al (2020) Preoperative transcranial doppler and cerebral oximetry as predictors of delirium following valvular heart surgery: a case-control study. J Clin Monit Comput 34:715–723
Soh S, Shim J-K, Song J-W et al (2017) Postoperative delirium in elderly patients undergoing major spinal surgery: role of cerebral oximetry. J Neurosurg Anesthesiol 29:426–432
Wang X, Feng K, Liu H et al (2019) Regional cerebral oxygen saturation and postoperative delirium in endovascular surgery: a prospective cohort study. Trials 20:504. https://doi.org/10.1186/s13063-019-3586-y
Roberts ML, Lin H-M, Tinuoye E et al (2020) The association of cerebral desaturation during one-lung ventilation and postoperative recovery: a prospective observational cohort study. J Cardiothorac Vasc Anesth 35:542–550. https://doi.org/10.1053/j.jvca.2020.07.065
Cui F, Zhao W, Mu DL et al (2021) Association between cerebral desaturation and postoperative delirium in thoracotomy with one-lung ventilation: a prospective cohort study. Anesth Analg 133:176–186
Sinclair S, James S, Singer M (1997) Intraoperative intravascular volume optimisation and length of hospital stay after repair of proximal femoral fracture: randomised controlled trial. BMJ 315:909–912
Wiles MD, William JDW, Chris GM et al (2011) The use of LiDCO based fluid management in patients undergoing hip fracture surgery under spinal anaesthesia: neck of femur optimisation therapy—targeted stroke volume (NOTTS): study protocol for a randomized controlled trial. Trials 12:213
Seung-Taek Oh (2019) Jin Young park. Postopera Delirium Korean J Anesthesiol 72:4–12
Aldecoa C, Bettelli G, Bilotta F et al (2017) European society of anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol 34:192–214
Heringlake M, Heinze H, Misfeld M et al (2008) Goal-directed hemodynamic optimization in high-risk cardiac surgery patients: a tale from the past or a future obligation? Minerva Anestesiol 74:251–258
Funding
This work was supported by the Fundamental Research Funds for the Central Universities (New medicine of USTC, WK9110000082), Postdoctoral funded projects in Anhui Province (2019B301) and Funding for key disciplines of Anesthesiology (13th five-year plan, ZD135_0005).
Author information
Authors and Affiliations
Contributions
K-QH contributed to study concept and design; K-QH, SW, WZ, QL took part in acquisition of data including risk of bias assessment; K-QH, QL involved in analysis and interpretation of data; K-QH, X-QC took part in drafting of the manuscript; all declared authors participated in critical revision of the manuscript for important intellectual content; administrative, technical, or material support is not applicable; K-QH, X-QC involved in study supervision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declared that they do not have a conflicting interest.
Ethical approval
Not applicable.
Statement of human and animal rights
This article does not contain any studies with human participants performed by any of the authors.
Consent to participate
Not applicable.
Consent for publication
Authors are responsible for correctness of the statements provided in the manuscript.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
He, Kq., Wang, S., Zhang, W. et al. What is the impact of perioperative cerebral oxygen desaturation on postoperative delirium in old population: a systemic review and meta-analysis. Aging Clin Exp Res 34, 1761–1770 (2022). https://doi.org/10.1007/s40520-022-02128-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02128-6