Abstract
Background
The effect of low and high concentration of some hematological parameters in the blood can have a negative impact on health.
Aim
Therefore, we investigated the associations between hematological parameters and all-cause mortality among older people living in Poland.
Methods
The study was carried out among 75–80-year-old participants (n = 403) from Warsaw and Olsztyn regions, Poland. Information on lifestyle factors and food consumption were obtained at baseline (June 1, 1999) using a self-administered questionnaire. Red blood cell, haemoglobin, hematocrit, mean corpuscular volume (MCV), mean corpuscular haemoglobin (MCH), and mean corpuscular haemoglobin concentration (MCHC) were determined. The data on deaths from all-causes were collected from the baseline until October 31, 2006. During an average of 7.4 years of follow-up, we ascertained 154 cases of death from all-causes.
Results
Compared with men in the lowest tertile of MCV, MCH, and MCHC, the multivariable hazard ratios (HRs) of all-cause mortality in those in the highest tertile were 0.35 (95% CI, 0.17–0.73), 0.32 (95% CI, 0.16–0.67), and 0.44 (95% CI, 0.22–0.88), respectively. In contrast, among women after combining the second and the third tertiles of MCV, MCH, and MCHC, the HRs were 2.01 (95% CI, 1.01–3.99), 1.71 (95% CI, 0.85–3.43), and 1.09 (95% CI, 0.62–1.94), respectively.
Discussion/conclusion
We observed inverse associations between some hematological parameters and all-cause mortality among men, but not among women. This may be explained by a difference in iron metabolism, iron status, hormone regulations, or the occurrence of some diseases.
Similar content being viewed by others
Introduction
The prevalence of anaemia increases dramatically with advancing age, reaching nearly 50% in older people, and will be increased further due to population aging [1,2,3]. Most anaemia cases in older individuals result from iron deficiency, chronic inflammation, chronic kidney disease, or some of them may be unexplained [4,5,6]. Anaemia of inflammation is one of the main types of anaemia in the geriatric population and is connected to many age-related diseases such as: obesity, cancer, chronic renal disease, etc. Even mild anaemia is related to increased mortality [7, 8]. Low haemoglobin (Hb) concentration contributes to pathological conditions, such as poor functional status, cognitive decline and dementia, increased risk of hospitalization, morbidity, and mortality [9,10,11,12].
In contrast, a few studies have shown that a high red blood cell (RBC) count, even within the normal reference range, was strongly associated with an increased risk of all-cause mortality and cardiovascular (CVD) incidence and mortality in middle-aged and elderly people [13,14,15,16,17]. The Framingham Heart Study indicated that older men with hematocrit (HTC) above 48% compared to those with HTC 45–46% had a statistically significantly higher risk of CVD and a tendency to higher risk of coronary heart mortality [18].
Until now, most studies determined the associations between Hb and HTC and the risk of mortality among elderly, but did not test other hematological parameters, such as mean corpuscular volume (MCV), mean corpuscular haemoglobin (MCH) and mean corpuscular haemoglobin concentration (MCHC).
Given the inconsistent results of the studies on Hb and HTC and lack of studies on MCV, MCH, and MCHC and risk of morbidity and mortality among the older people, we investigated the associations of hematological parameters commonly tested by General Practitioners (GPs) with all-cause mortality in 75–80-year-old men and women living in two districts of Poland.
Methods
Study design and population
In the spring of 1999, 1200 free living respondents aged 75–80 years (born in 1914–1924) were randomly selected from the Census Bureau according to the Personal Identification Number (PESEL) by quota 600 participants from the Warsaw region and 600 from the Olsztyn region, Poland (Fig. 1). In each region, the proportion of selected men and women was 1:1 and the proportion of people living in cities, small towns, and rural areas was 1:1:1. The participation rate in the study was 54.4% (306 men and 347 women). Among these participants, 403 people (190 men and 213 women) have agreed to a blood test and those people were included in the analysis. The study was approved by the Regional Ethics Commission located at the National Food and Nutrition Institute, Warsaw, Poland.
Assessment of diet and other exposure
In the spring of 1999, after a pilot study carried out among 60 participants from the Warsaw region and 60 participants from the Olsztyn region, the main study was conducted. Data on food consumption were collected using 3-day records in Warsaw and 24-h recalls in the Olsztyn region. Information on physical activity, education, smoking status, avoiding alcohol, dietary supplement use, and medicine use was obtained at baseline using a self-administered questionnaire. The body mass index (BMI) was calculated by dividing the weight (kg) by the square of height (m).
Hematological parameters and total serum cholesterol level
Blood parameters were determined in the medical laboratory of the National Food and Nutrition Institute in Warsaw and in the medical laboratory of the Municipal Polyclinic Hospital in Olsztyn. RBC, Hb, HCT, MCV, MCH, and MCHC in blood were determined using the Biocode Hycel Celly Hematology Analyzer (Biocode Hycel, Rennes, France) in Warsaw and the Minos analyzer (ABX, France) in Olsztyn. Total cholesterol was measured in serum using the Vitros 250 analyzer (Johnson & Johnson Clinical Diagnostic, New Zealand) in Warsaw and the Cobas Mira E analyzer (La Roche, Switzerland) in Olsztyn.
Case ascertainment
The data on deaths from all causes were collected from June 1, 1999 until October 31, 2006. The data on deaths were obtained from the Register Offices individually for each participant.
Statistical analysis
Cox proportional hazards regression models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) of all-cause mortality. We categorized participants into tertiles of RBC, Hb, HCT, MCV, MCH, and MCHC, separately for men and women. Among women in the result description, the second and third quartiles of hematological parameters were combined because of a relatively small number of deaths and unstable HRs.
The multivariable models included the following variables: age (continuous variable), region (Warsaw or Olsztyn), physical activity (very low and low, or moderate and high), education (lower then higher, or higher and university), smoking status (yes or no), avoiding alcohol (yes or no), supplement use (yes or no), medicine use (yes or no), body mass index (≤25 or >25 kg/m2), serum cholesterol level (tertiles), and intake of energy and iron (tertiles). The multivariable models were calculated separately for each tested hematological parameter.
To compare survival curves, the Kaplan–Meier method and the log-rank test were used. The proportional hazards’ assumption was evaluated by regressing scaled Schoenfeld residuals against survival time. There was no evidence of departure from the assumption. To calculate p values for trend, the median values of tertiles for RBC, Hb, HCT, RBC, MCV, MCH, and MCHC were used as a continuous variable. Using the likelihood ratio test, we tested statistical interactions between tested hematological parameters in predicting all-cause mortality according to sex, physical activity, BMI, smoking status, and avoiding alcohol.
The statistical analyses were performed using Statistica version 10.0 PL and IBM SPSS Statistics version 21. The Shapiro–Wilk test was used to check the data distribution. Average values of the tested parameters were compared using the Mann–Whitney U test, while categorical data were analyzed using the Chi2 Pearson test. All reported p values were two-sided, and p values ≤0.05 were considered as statistically significant.
Results
The mean age of participants was 77.0 ± 1.7 years (Table 1). Over half of the respondents were women (52.9%) and lived in the Warsaw region (53.3%). Most participants evaluated their physical activity as moderate or high and had primary or secondary education. Twenty percent of men and about six percent of women were current smokers, and 14 and 22%, respectively, declared to avoid alcohol. In the past 12 months, dietary supplements and medicine were used by 41 and 72% of participants, respectively. About 73% of respondents had a BMI higher than 25 kg/m2. The concentration of serum cholesterol was statistically significantly higher in women compared to men, while the intake of energy and iron was significantly lower in women.
RBC and concentration of Hb, HCT, MCH, and MCHC were significantly higher among men than they were among women (Table 2). We observed a higher percentage of men compared to women with the following parameters below reference values: RBC (43.1 vs. 15.5%, respectively), Hb (12.6 vs. 1.4%, respectively), and HCT (27.5 vs. 16.0%, respectively). At the same time, the percentage of men with MCV (21.7%) and MCH (24.5%) above reference values was higher in comparison to women (15.1% and 13.5%, respectively).
During an average of 7.4 years (3784 person-years, 1999–2006) of follow-up, we ascertained 154 cases of deaths from all-causes, including 81 deaths in men (42.6%) and 73 deaths in women (34.3%). This difference between men and women was not significant (p = 0.08).
We observed statistically significant interactions between hematological parameters (MCV and MCH) and sex in relation to all-cause mortality (p for interaction: 0.004 and 0.005, respectively); therefore, all analysis were conducted separately for men and women.
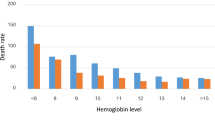
After adjusted HRs for possible confounders (multivariable HRs), we observed statistically significant inverse associations of some hematological parameters with risk of all-cause mortality among men (Table 3). Compared with men in the lowest tertile of MCV, MCH, and MCHC, the HRs of all-cause mortality in those in the highest tertile were 0.35 (95% CI, 0.17–0.73), 0.32 (95% CI, 0.16–0.67) and 0.44 (95% CI, 0.22–0.88), respectively. Among women in the second tertile versus those in the first tertile, the HR of all-cause mortality was 2.43 (95% CI, 1.20–4.92) for MCV and 2.12 (95% CI, 0.99–4.50) for MCH, while among women in the third tertile, the HRs were 1.44 (95% CI, 0.65–3.19%) and 1.40 (95% CI, 0.66–2.99), respectively. After combining the second and the third tertiles of MCV, MCH, and MCHC in women, the HRs were 2.01 (95% CI, 1.01–3.99), 1.71 (95% CI, 0.85–3.43), and 1.09 (95% CI, 0.62–1.94), respectively. Survival curves by tertiles of MCV, MCH, and MCHC in the group of men and women were presented in Fig. 2. We did not observe statistically significant associations by tertiles of RBC, Hb, and HCT with all-cause mortality among men and women.
Moreover, there were no statistically significant interactions between the tested hematological parameters and the smoking status, physical activity, alcohol consumption, and BMI (all p-interaction > 0.1).
Discussion
In this study of older people, some hematological parameters were inversely associated with a risk of all-cause mortality among men, but not among women. Men in the highest versus those in the lowest tertile of MCV, MCH, and MCHC had a statistically significant 65, 68, and 56% lower risk of all-cause mortality, respectively. In contrast, women in the higher tertiles of MCV (the second and the third tertiles combined) in comparison to those in the first tertile had a twofold higher risk of all-cause mortality. No similar associations were observed for RBC, Hb, and HCT. Moreover, in our previous study in the same population of men and women, we observed that women with iron serum concentration above the median had a statistically significantly fourfold (HR: 4.10; 95% CI: 1.16–14.5) higher risk of all-cause mortality than those with lower iron serum concentration. In men, a similar association was not observed [19].
To the best of our knowledge, there are no previously published studies on MCV, MCH, and MCHC in relation to all-cause and specific-cause mortality. Most epidemiological studies have investigated the association between Hb [9, 20,21,22,23] and HCT [24,25,26] and the risk of all-cause mortality [9, 20,21,22,23] and CVD mortality [23,24,25,26] among people aged 55 years and older. The HRs of all-cause mortality increased from 33% in men and women with low Hb concentration to twofold in people with mild anaemia and sixfold in those with moderate and severe anaemia [23]. Results of a large prospective cohort study (n = 49,983) indicate a U-shape relationship between HCT and all-cause and CVD mortality in women; low and high values of HCT were associated with higher risk of death [24]. In addition, in a case–control study HCT ≥ 50% resulted in an 80% higher risk of coronary heart disease (CHD) mortality in men [22]. No similar associations between HCT and CHD were observed in the Second National Health and Nutrition Examination Survey [26].
In our study, we did not find any significant associations between Hb and HCT and all-cause mortality among men and women. However, among men, the HRs were 32 and 23% lower in the third tertile compared to the first tertile of Hb and HCT, respectively, while among women, the HR was 24% lower only for HCT. These results are consistent with the percentage of people below reference levels for these parameters. We suppose that the lack of a significant impact of Hb on all-cause mortality was a result of a small number of anemic women in our study (1.4% of women) and a relatively low percentage of anemic men (12.6%).
We can speculate that the gender differences in the presented results can depend on different iron metabolism and iron status as well as different hormone regulations and health condition. It is known that androgen and estrogen concentrations may play an important role in erythro- and myelopoiesis processes [27]. Based on a clinical trial, it was observed that a testosterone-induced increase in Hb and HCT was associated with stimulation of erythropoietin and reduced ferritin and hepcidin concentrations among elderly men [28]. Moreover, high risk of all-cause mortality among women may be caused by a potential adverse effect of iron. It is known that an excess of iron has pro-inflammatory and pro-oxidative properties [29, 30]. By catalysing the formation of free radicals, high levels of iron may lead to lipid peroxidation [31,32,33], protein, and DNA modifications [33, 34]. It was observed that MCH and MCHC were inversely correlated with C-reactive protein [35], and MCHC was associated with carotid intima media thickness and with interleukin-6 (IL-6) among hypertensive patients [36]. It seems feasible that the observed lower mortality in men in the highest versus those in the lowest tertile of MCV may be related to the level of red cell distribution width (RDW). It has been shown that the level of RDW inversely correlated with MCV [15, 37] and higher RDW is a strong predictor of all-cause mortality in adults of 45 and older [15, 38] as well as in older people with and without age-associated diseases [38].
The major strengths of the present study were the broad use of hematology parameters, a random selection of people from two different districts of Poland as well as data collection in both regions based on the same questionnaires. We adjusted the Cox proportional hazard models for the main potential confounders, which could affect the final results; however, we were not able to rule out residual or unmeasured confounding. The main limitation of this study was a relatively small number of participants and instances of death from all-causes. People who refused to participate in the study were characterized by a worse health status than those who took part; thus, the study population was healthier than the older Polish public. Another limitation of the study was the lack of data on the ferritin, transferrin receptor concentrations, and red cell distribution width as well as inflammation markers. Parameters such ferritin and transferrin receptor concentrations are more specific to determine iron status; however, hematological parameters are commonly examined in older people by GPs and they are useful prognostic factors of morbidity and mortality.
Conclusions
The findings from this prospective study indicate that some hematological parameters were inversely associated with the risk of all-cause mortality among older men, but not among women. The differences in the results between genders can be explained by different iron metabolism, iron status, and hormone regulations among men and women, and also by the occurrence of diseases, which can have an impact on hematological parameters. This finding warrants confirmation in further prospective studies conducted on a bigger population.
References
Tettamanti M, Lucca U, Gandini F et al (2010) Prevalence, incidence and types of mild anemia in the elderly: the “Health and Anemia” population-based study. Haematologica 95:1849–1856
Gaskell H, Derry S, Andrew Moore R et al (2008) Prevalence of anemia in older persons: systematic review. BMC Geriatr 8:1
Guralnik JM, Eisenstaedt RS, Ferrucci L et al (2004) Prevalence of anemia in persons 65 years and older in the United States: evidence for a high rate of unexplained anemia. Blood 104:2263–2268
Eisenstaedt R, Penninx BWJH, Woodman RC (2006) Anemia in the elderly: current understanding and emerging concepts. Blood Rev 20:213–226
Izaks GJ, Westendorp RG, Knook DL (1999) The definition of anemia in older persons. JAMA 281:1714–1717
Ania BJ, Suman VJ, Fairbanks VF et al (1997) Incidence of anemia in older people: an epidemiologic study in a well defined population. J Am Geriatr Soc 45:825–831
Turusheva A, Frolova E, Hegendoerfer E et al (2016) Predictors of short-term mortality, cognitive and physical decline in older adults in northwest Russia: a population-based prospective cohort study. Aging Clin Exp Res. doi:10.1007/s40520-016-0613-7
Semba RD, Ricks MO, Ferrucci L et al (2007) Types of anemia and mortality among older disabled women living in the community: the Womenʼs Health and Aing Study I. Aging Clin Exp Res 19:259–264
den Elzen WPJ, Willems JM, Westendorp RGJ et al (2009) Effect of anemia and comorbidity on functional satus and mortality in old age: results from the Leiden 85-plus Study. CMAJ 181:151–157
Riva E, Tettamanti M, Mosconi P et al (2009) Association of mild anemia with hospitalization and mortality in the elderly: The Health and Anemia population-based study. Haematologica 94:22–28
Patel KV (2008) Epidemiology of anemia in older adults. Semin Hematol 45:210–217
Peters R, Burch L, Warner J et al (2008) Haemoglobin, anemia, dementia and cognitive decline in the elderly, a systematic review. BMC Geriatr 8:18
Cavusoglu E, Chopra V, Gupta A et al (2010) Relation between red blood cell width (RDW) and all-cause mortality at 2 years in an unselected population referred for coronary angiography. Int J Cardiol 141:141–146
Ani C, Ovbiagele B (2009) Elevated red blood cell distribution width predicts mortality in persons with known stroke. J Neurol Sci 277:103–108
Patel KV, Ferrucci L, Ershelr WB et al (2009) Red cell distribution width and the risk of death in middle-age and older adults. Arch Intern Med 169:515–523
Perlstein TS, Wenve J, Pfeffer MA et al (2009) Red blood cell distribution width and mortality risk in a community-based prospective cohort. Arch Intern Med 169:588–594
Tonelli M, Sacks F, Arnold M et al (2008) Relation between red blood cell distribution width and cardiovascular event rate in people with coronary disease. Circulation 117:163–168
Ganon DR, Zhang TJ, Brand FN et al (1994) Hematocrit and the risk of cardiovascular disease-the Framingham Study: a 34-year follow-up. Am Heart J 127:674–682
Kaluza J, Jeruszka-Bielak M (2006) The relationship between iron nutritional status and mortality among older people from the Warsaw region. Polish J Environ Sud 15:329–335
De la Cruz-Góngora V, Manrique-Espinoza B, Villalpando S et al (2014) Short-term impact of anemia on mortality: evidence from a sample of Mexican older adults. J Aging Health 26:750–765
Shavelle RM, MacKenzie R, Paculdo DR (2012) Anemia and mortality in older persons: does the type of anemia affect survival? Int J Hematol 95:248–256
Landi F, Russo A, Danese P et al (2007) Anemia status, hemoglobin concentration, and mortality in nursing home older residents. J Am Med Dir Assoc 8:322–327
Zakai NA, Kaiz R, Hirsch C et al (2005) A prospective study of anemia status, hemoglobin concentration, and mortality in an elderly cohort. Arch Intern Med 165:2214–2220
Boffetta P, Islami F, Vedanthan R et al (2013) A U-shaped relationship between haematocrit and mortality in a large prospective cohort study. Int J Epidemiol 42:601–615
Kunnas T, Solakivi T, Huuskonen K et al (2009) Hematocrit and the risk of coronary heart disease mortality in the TAMRISK study, a 28-year follow-up. Prev Med 49:45–47
Brown DW, Giles WH, Croft JB (2001) Hematocrit and the risk of coronary heart disease mortality. Am Heart J 142:657–663
Ikeda Y, Tajima S, Izawa-Ishizawa Y et al (2012) Estrogen regulates hepcidin expression via GPR30-BMP-dependent signaling in hepatocytes. PLoS One 7:e40465
Bachman E, Travison TG, Basaria S et al (2014) Testosterone induces erythrocitosis via increased erythropoietin and suppressed hepcidin: evidence for a new erythropoietin/hemoglobin set point. J Gerontol A Biol Sci Med Sci 69:725–735
Jamova K, Valko M (2011) Advances in metal-induced oxidative stress a human disease. Toxicology 283:65–87
Selim MH, Ratan RR (2004) The role of iron neurotoxicity in ischemic stroke. Ageing Res Rev 3:345–353
King SM, Donangelo CM, Knutson MD et al (2008) Daily supplementation with iron increases lipid peroxidation in young women with low iron stores. Exp Biol Med (Maywood) 233:701–707
Lasheras C, Gonzales S, Huerta JM et al (2003) Plasma iron is associated with lipid peroxidation in an elderly population. J Trace Elem Med Biol 17:171–176
Zago MP, Verstraeten SV, Oteiza PI (2000) Zinc in the prevention of Fe2 +-initiated lipid and protein oxidation. Biol Res 33:143–150
Hori A, Mizoue T, Kasai H et al (2010) Body iron store as a predictor of oxidative DNA damage in healthy men and women. Cancer Sci 101:517–522
Okada Y, Takahashi A, Ohmiya H et al (2011) Genome-wide association study for C-reactive protein levels identified pleiotropic associations in the IL6 locus. Hum Mol Genet 20:1224–1231
Fornal M, Wizner B, Cwynar M et al (2014) Association of red blood cell distribution width, inflammation markers and morphological as well as rheological erythrocyte parameters with target organ damage in hypertension. Clin Hemorheol Microcirc 56:325–335
Hsieh YP, Chang CC, Kor CT et al. (2016) The predictive role of red cell distribution width in mortality among chronic kidney disease patients. PLoS ONE 11:e0162025. doi:10.1371/journal.pone.0162025
Patel KV, Semba RD, Ferrucci L et al (2010) Red cell distribution width and mortality in older adults: a meta-analysis. J Gerontol A Biol Sci Med 65A: 258–266
Acknowledgements
We are grateful to Prof. Wojciech Roszkowski from the Department of Human Nutrition WULS–SGGW for general support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any potential conflicts of interest to declare.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Frąckiewicz, J., Włodarek, D., Brzozowska, A. et al. Hematological parameters and all-cause mortality: a prospective study of older people. Aging Clin Exp Res 30, 517–526 (2018). https://doi.org/10.1007/s40520-017-0791-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-017-0791-y