Abstract
Purpose of Review
Despite advanced technologies to avoid corrosion of dental implants, the mechanisms toward the release of metals and their role in the onset of peri-implant diseases are still under-investigated. Effective knowledge on the etiopathogenesis of corrosive products and preventive strategies mitigating the risks for surface degradation are thus in dire need. This review aimed to summarize evidence toward biocorrosion in the oral environment and discuss the current strategies targeting the improvement of dental implants and focusing on the methodological and electrochemical aspects of surface treatments and titanium-based alloys.
Recent Findings
Recent studies suggest the existence of wear/corrosion products may correlate with peri-implantitis progress by triggering microbial dysbiosis, the release of pro-inflammatory cytokines, and animal bone resorption. Furthermore, current clinical evidence demonstrating the presence of metal-like particles in diseased tissues supports their possible role as a risk factor for peri-implantitis. For instance, to overcome the drawback of titanium corrosion, researchers are primarily focusing on developing corrosion-resistant alloys and coatings for dental implants by changing their physicochemical features.
Summary
The current state-of-art discussed in this review found corrosion products effective in affecting biofilm virulence and inflammatory factors in vitro. Controversial and unstandardized data are limitations, making the premise of corrosion products being essential for peri-implantitis onset. On the other hand, when it comes to the strategies toward reducing implant corrosion rate, it is evident that the chemical and physical properties are crucial for the in vitro electrochemical behavior of the implant material. For instance, it is foreseeable that the formation of films/coatings and the incorporation of some functional compounds into the substrate may enhance the material’s corrosion resistance and biological response. Nevertheless, the utmost challenge of research in this field is to achieve adequate stimulation of the biological tissues without weakening its protective behavior against corrosion. In addition, the translatability from in vitro findings to clinical studies is still in its infancy. Therefore, further accumulation of high-level evidence on the role of corrosion products on peri-implant tissues is expected to confirm the findings of the present review besides the development of better methods to improve the corrosion resistance of dental implants. Furthermore, such knowledge could further develop safe and long-term implant rehabilitation therapy.
Similar content being viewed by others
Introduction
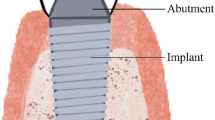
Since the introduction of titanium (Ti) dental implants in the 1960s by Branemark [1], the therapy with Ti-based dental implants has evolved from an accidental experimental discovery to a predictable standard of care for replacing missing teeth presenting a survival rate above 96% [2•]. This achievement is primarily due to the good mechanical properties as well as resistance to corrosion and excellent biological performance of Ti, which are mainly led by their inherent ability to form a spontaneous Ti oxide layer after exposure to oxygen atmosphere (mainly TiO2) [3]. Nevertheless, the biomaterials currently used for dental implant design are still far from perfect. Although the passivation provided by the nano-scale amorphous TiO2 layer is well known to act as a protective barrier against corrosion in physiological conditions (i.e., neutral pH), when dental implants are inserted into the complex in vivo oral environment, the constant exposure to acidic substances and microbial metabolites may proceed in reduced pH and consequent irreversible rupture of the passive film. Additionally, the TiO2 barrier presents a poor tribological efficacy and can be easily removed/disrupted under loading [4]. As such, the implant becomes more susceptible to electrochemical reactions between the surface and oral fluids, resulting in partial or complete dissolution of the metal [5•, 6–8].
The endurance of these corrosive factors over time, along with wear induced by implantation procedures (e.g., friction, micro-motion), is the process that can cause the undesired release of metallic ions and particles from the implant to the surrounding tissues. In consequence, it may eventually lead to severe biological complications such as peri-implant diseases and even systemic toxicity, in a worst-case scenario [9•, 10–12]. Importantly, recent reports have hypothesized the contribution of the Ti particles to the onset and progression of peri-implant bone loss. In fact, it has been pointed out by the 2017 AAP/EFP World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions [13•] as a potential risk factor for peri-implantitis but with no conclusive evidence based on the currently available data. Thus, from this standpoint and considering the current prevalence of peri-implantitis (about 57% at patient-level) [14•], studying the influence of corrosion-induced release of ions and particles as a driving factor for peri-implant diseases and early/late failure of dental implants remains clinically relevant. Additionally, even though the problem of corrosion of dental implants has been successfully addressed through innovative surface modifications and alternative biomaterials using nobler metal alloys, the race for an ideal dental implant design capable of protecting the material from corrosion effects has disclosed numerous techniques and strategies that are stagnated in the bench, thus providing no consensus for a solid advance for clinical application.
Therewith, this review provides a close look at the available information regarding the corrosive factors/mechanisms of metal ions released from dental implants materials and their consequent biological side effects on peri-implant tissue and systemic health. Furthermore, a compilation of key factors driving the anticorrosive effect of current surface modification techniques and metal alloys is presented, targeting a safer design of dental implants to ensure the long-term success of the implant rehabilitation therapy.
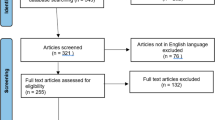
Search Strategy
A literature review focusing on the corrosion process of dental implants was undertaken aiming to answer the following focused question: “What is the current evidence toward the key factors influencing dental implants biocorrosion and driving the anticorrosive effect of implant surface modification techniques and titanium alloys?” For this, as a first step, two reviewers (B.E.N. and J.M.C.) searched for appropriate articles in the Pubmed (Medline) database using the combination of the terms “dental implants” OR “surface treatments” OR “alloys” AND “corrosion” OR “electrochemical” OR “degradation.” This was complemented by manual searches in peer-reviewed journals and snowballing approach to identify additional relevant studies in the reference lists of included articles. Finally, after screening the potential eligible titles and abstracts that addressed the focused question, relevant findings from the included articles were integrated into the following writing topics, as appropriate.
Dental Implants Meet the Challenges of the Reactive Oral Environment
From the moment dental implants are inserted in the oral cavity, the fate of maintaining their physicochemical properties, especially the integrity of the protective TiO2 passive layer against corrosion, is highly dependent on the challenging conditions of the hostile electrolytic oral environment [8]. Usually, the oral fluids (i.e., saliva, blood plasma) are characterized by the presence of organic and inorganic substances in combination with a pH buffering mechanism that regulates the hypotonic and physiological condition of the medium (pH between 6 and 7) [15, 16]; however, some factors such as microbial metabolites and corrosive substances can reduce the pH, turning the environment acidic and highly reactive to chemically attack the metallic surfaces [7, 17, 18].
Corrosive substances, such as Cl−, F−, and H+, can be found in saliva, oral biofilms, prophylactic commercial formulations (e.g., toothpaste, mouth rinses, cariostatic gels), and foods [19–21]. Remarkably, the influence of F− ion concentration in the medium adversely affecting the corrosion resistance of titanium-based materials has been widely studied [20,21,22,23,24]. Beline et al., for example, showed that 0.2% sodium fluoride mouthwash reduced Ti corrosion resistance regardless of the surface treatment (machined, sandblasted, or acid etching) compared to fluoride-free mouthwashes [24]. Similar findings were reported by Chen et al. [25], in which results demonstrated that the Ti corrosion resistance decreased with the increasing concentration of fluoride (0–0.4 ppm F−) in Hanks’ solution. That previous study also demonstrated the increase in surface roughness and acceleration of Ti ion release, which was even more pronounced in an acidic environment (pH 7.3 vs. 5.0) [25]. It is suggested that these corrosion results are mainly due to the formation of hydrofluoric acid (HF) from fluoride ions when the aqueous environment is acidified by eating habits or microbial metabolites (F− + H+ → HF). HF is a well-known weak acid strongly reactive to metals because it has chemical characteristics prone to induce the breakdown of the TiO2 protective layer (TiO2 + 4HF → TiF4 + 2H2O) [26], thus promoting not only the degradation but also the discoloration of the metal surface due to the generated fluoride-titanium compounds (e.g., TiF4(TiF6)3−) [27].
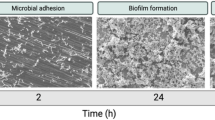
Concurrently, besides the local acidification induced by foods and beverages, oral bacteria’s promotion of acidic environment has been considered one of the major and intriguing causes to decrease the corrosion resistance of Ti [17]. The mechanism from which the microbial corrosion process occurs starts as soon as dental implants are inserted in the oral cavity. From this moment, not only the outer implant surface but also the micro gaps between the implant and abutments are immediately covered by protein-rich fluid pellicle—saliva and blood—that has remarkable specificity to bacterial components, thus promoting the adhesion of bacteria to these surfaces [28, 29]. As the biofilm develops, oxidation reactions due to bacterial acidic metabolites and oxygen level deficiency may occur between the biofilm-covered Ti surface (cathodic area) and the exposed Ti (anodic area), increasing the corrosion rate of the implant material [17]. Additionally, biofilm decontamination by mechanical debridement and chemical methods, such as citric acid rubbing, may also induce Ti release from the implant surface [30, 31].
In a nutshell, it is important to highlight that regardless of the etiologic factor driving the corrosion on Ti, bacterial cells and physicochemical factors act synergically for the implant surface degradation. For example, because biofilm development is influenced by the low pH microenvironment, the promotion of local acidification by modulating factors such as external acidic substances (e.g., foods, caffeine, cotinine, and nicotine) [4, 32, 33] and microbial components such as lipopolysaccharides [34] may accelerate the microbial corrosion process of Ti.
Furthermore, it is important to highlight that the literature has been increasingly reporting other chemical and biological substances to reduce implant corrosion, and it should not be neglected. Notably, Sousa et al. recently demonstrated that hydrogen peroxide (H2O2) concentration in mouthwash was able to reduce the corrosion resistance of Ti6Al4V alloy under dynamic conditions simulating the hygiene protocol usually indicated in post-surgical implant placement [35]. Accordingly, other studies focusing on the role of H2O2 as a by-product of the peri-implant inflammatory process also demonstrated a reduction of implant corrosion stability [21, 36]. Yet, in a most unfavorable environmental condition, combining three oxidative agents (H2O2, lactic acid released from bacteria, and fluoride), the corrosion of the Ti surface considerably increased compared to the results of these substances alone [21]. In the same way, some studies have also assigned the role of albumin, the most abundant protein in blood plasma, to reduce the kinetic of Ti surface passivation and accelerate the dissolution of the material [36, 37].
Altogether, these physical, chemical, microbiological, and inflammatory corrosion processes promote the surface damage of dental implants and the release of corrosion by-products that may adversely alter the microenvironment conditions of peri-implant tissues, leading to cytotoxic and inflammatory reactions. Further, such event compromises the success of dental implant rehabilitation therapy.
Biointerface-Safety of Corrosive Products on Oral/Systemic Health—Should We Care?
With the growing aging world population and its expectation for a predictable long-term dental implant therapy, knowing the factors that contributes to the success/failure of the rehabilitation is of utmost importance. Since one of the main concerns towards implant therapy is the high prevalence of peri-implant disease [14•], unraveling the onset and pattern, as well as the risk factors for disease progression, remains clinically relevant. For instance, because it has been evidenced that metallic corrosive products are not fully bioinert; multiple studies have been raised concerns regarding the potential of wear and corrosion products to induce adverse biological reactions not only locally in the surrounding peri-implant tissues but also systemically throughout the human body [5•, 9•, 18, 33, 38•, 39].
Once corrosion products are released from the implant surface due to mechanical (wear particles/debris), electrochemical (corrosion-related free metal ions, organometallic complexes, and salts), and/or combination of both mechanical and electrochemical processes (i.e., tribocorrosion), a series of biochemical reactions might be triggered at the biointerface microenvironment [4, 38•, 40] (Fig. 1). In this context, several in vitro and pre-clinical experiments have demonstrated the role of Ti ions and particles to present toxic and/or pro-inflammatory effects [33, 41•]. In the case of mechanical wear, for example, Ti particles released by ultrasonic scaling of sandblasted and acid-etched (SLA) surface induced a higher in vitro inflammatory response than the control LPS-treated human macrophages culture. In this case, a higher gene expression level of the pro-inflammatory cytokines IL1β, IL6, and TNFα was noted, probably because macrophages may have phagocytosed Ti particles [30]. Interestingly, such inflammatory response due to Ti phagocytosis is an event that has been reported to occur not only with macrophages but also with neutrophil cells [33]. In addition, it seems that the macrophage-related expression of cytokine level may be directly dependent on the increasing concentration of particles and the type of implant surface treatment (machined, sandblasted, and SLA) [30]. Note that the in vitro cytokine level and in vivo bone resorption (mouse calvariae model) were more pronounced when particles were originated from sandblasted discs than from SLA and machined surfaces, probably due to differences in chemical profile and particle sizes [30].
Schematic depiction of hypothesized biochemical mechanisms for corrosion-related titanium-tissue interaction of dental implants. Corrosion process of dental implants leading to Ti particle/ion release arises from the electrochemical attack of the reactive oral environment to the implant surface by disrupting the protective oxide passive layer (TiO2). As a consequence, there is an induction of inflammatory process in the soft tissue cells (e.g., fibroblasts) and bone cells, which is mainly led by signaling factors promoting the differentiation and recruitment of osteoclast cells responsible for peri-implant bone resorption (left panel). In a close look, there are several potential biochemical routes for the occurrence of these peri-implant inflammatory processes (right side). For instance, when dental implants are subjected to physical, chemical, and bacterial factors present in the reactive oral environment, it can be supposed that there is a multidirectional pathway loop for the Ti-tissue interaction. For example, once metallic particles/ions are released, the peri-implant inflammatory process may occur by activating the function of phagocytic cells such as (1) neutrophils and (2) macrophages, (3) stimulating some communication pathways of osteoblastic cells, or even promoting (4) microbial accumulation in the degraded rougher surface region. In particular, the phagocytosis of Ti ions may lead to a (5) higher expression level of pro-inflammatory cytokines (e.g., IL1β, IL6, and TNFα), and all of these mentioned processes (3 to 5) may induce (6) RANKL expression within osteogenic cells, thus indirectly promoting RANKL-induced osteoclast differentiation and consequent (7) tissue inflammation and bone resorption. Once inflammation occurs, the pH level of the region is reduced with concurrent microbial dysbiosis, favoring the generation of bacterial acid products that, in the end, also negatively affect the corrosion resistance of Ti. Created and adapted from “Anti-neutrophil Cytoplasmic Antibody (ANCA)-associated Vasculitis” and “Proposed Therapeutic Treatments for COVID-19 Targeting Viral Entry Mechanism,” using BioRender.com (2021)
Choi et al. [42] reported that the larger the particle size, the more the expression of receptor activator of nuclear factor κB ligand (RANKL), a dominant signal for osteoclast recruitment, and the proteolytic activities of matrix metalloproteinases (MMP) 2 and 9, involved in the degradation of bone matrix and mineralization. The authors also demonstrated that although all particle sizes were able to induce the loss of implant integration with bone tissue in vivo (rat tibia model), large particle sizes (≥10.0 μm and <15 μm) were shown to maintain osteoblast in vitro viability whereas a reduction was observed for smaller particle sizes, indicating that different functional responses may be generated depending on the particle size present in the surrounding tissues, which is reported to vary from 100 nm to 54 μm [41•].
The cytotoxic effect of Ti products on the inflammatory response of human cells has been demonstrated for particles and Ti ions. Mine et al. showed that the concentration of Ti ions might have an impact on the bone remodeling of dental implants as 20 ppm Ti ions reduced cell viability of murine pre-osteoblastic MC3T3-E1, osteoclast-like RAW264.7, and epithelial cell-like GE-1 cells, and 9 ppm Ti ions increased the expression of RANKL and osteoprotegerin (OPG) in MC3T3-E1 cells [43]. In accordance, Wachi et al. [44] also demonstrated in vitro and in vivo (rat model) that, in the presence of bacterial LPS, 9 ppm Ti ions (limited concentration to induce a cytotoxic effect in vitro) can synergistically increase the ratio of RANKL to OPG and the level of CCL2, a chemokine related to activation of monocyte infiltration. Additionally, gingival epithelium loaded with Ti ions enhanced the localization of bacterial LPS endotoxin toll-like receptor 4, suggesting that Ti ions may play an important role in peri-implantitis onset by altering osteoclast differentiation due to changes in the sensitivity of the epithelium around microorganisms. In fact, in a previous study of our research group, Ti particles and ions demonstrated a striking influence on microbial growth in a dose-response manner, and Ti ions had the capacity to cause a dysbiotic change in the microbial community toward a profile similar to pathogenic biofilm-related to peri-implant infections [6].
Accordingly, evidence for Ti degradation in diseased peri-implant tissues has been demonstrated in human studies. As such, levels of released Ti were detected via ICP-MS (inductively coupled plasma mass spectrometry) in submucosal plaque [45•], soft-tissue biopsies [46], and exfoliative cytologic samples [47•, 48] in greater amount in diseased peri-implant mucosa than in healthy sites. Nevertheless, for both healthy and inflamed tissue biopsies, the Ti concentration found (7.3 to 38.9 μM) were reported to be within the levels needed to activate the IL-1β secretion from human macrophage in vitro, which is a phenomenon closely related to stimulating an in vivo proinflammatory reaction [46]. Thus, these findings suggest poor specificity between the biological impact of Ti concentration and the pathological process of peri-implant diseases.
Indeed, there is some biological plausibility of the relationship between the origin of Ti ions/particles in the peri-implant tissue and the onset of biofilm-related peri-implant diseases. For instance, it can be supposed that there is a multidirectional pathway loop for the degradation of Ti surface in the oral environment: (i) wear, acidic substances, and metabolites released from bacteria (e.g., lactic acid) promote the degradation and acidification of the peri-implant microenvironment, thus allowing the passive oxide layer breakdown with consequent pitting and galvanic attacks; (ii) corroded Ti surface presenting increased roughness provides additional niches for bacterial recolonization; (iii) microbial accumulation promotes oxygen level deficiency that jeopardizes the reformation of the passive oxide layer, thus promoting crevice corrosion on Ti surface; (iv) corrosion products induce microbial dysbiosis favoring the occurrence of inflammatory reaction and the consequent generation of acid products (hydrogen peroxide and H+) that in the end also negatively affect the corrosion resistance of Ti. Nevertheless, it is of utmost importance to emphasize that among biofilm models used to assess microbial corrosion on Ti, only a few studies available in the literature considered the polymicrobial diversity of oral environment resembling the clinical situation [17], emphasizing the need for further in vitro and in vivo investigations on the cause-effect pattern between microbial accumulation and Ti surface degradation.
In addition, considering that all these corrosion processes occur in a complex biological environment, the transportation of corrosion by-products to remote organs is inherent. Ti ions have been related to ionically bind to blood proteins and be transported throughout the human body to distant organs such as kidneys, liver, and lung, thus extending toxicity concerns from local to a general health scope [39]. Therefore, as it is well known that corrosion and Ti release indeed occur and are correlated with inflammatory reaction induction and potential systemic cytotoxic effects, strategies to avoid the corrosion of dental implants are necessary and have been extensively studied.
Strategies to Avoid/Reduce the Corrosion of Dental Implants
Given what was mentioned in the above topics, some strategies have been drawn to avoid/reduce the corrosion of dental implants and the consequent undesired effects. Inhibiting corrosion of metals is an interdisciplinary approach in which engineering solutions are applied to the biomedical field to improve their applicability under a complex biological environment. Nevertheless, the race for novel approaches has led to numerous technologies that do not reach an endpoint consensus on the ideal strategy that could provide real progress for clinical application. In this way, knowing the key factors driving the corrosion resistance of current technologies is of great relevance for the guidance of future studies. Herein, we will review two main methods: the design of corrosion-resistant Ti alloys and the development of protective surface treatments.
The Search for Corrosion-Resistant Alloys for Dental Implants
When designing experimental alloys for dental implants to resist corrosion, the most straightforward strategy is altering their composition. Several alloying elements are known to inhibit the degradation process by driving the growth of highly stable passive oxide films and microstructures [49]. From designing a new experimental alloy to improving already existing ones, the final goal is to create a material that can achieve passivity [50], regulate the hydrogen evolution reaction [51, 52], and reduce the anodic/cathodic activity directly [22, 53].
Stainless steel, cobalt-based alloys, magnesium (Mg), and its alloys have proven their applicability as bone implants [11]. However, Ti is the most popular material used for dental implant manufacturing, and its alloys have been widely applied clinically. Table 1 sums up the main alloying elements added to Ti and their role in improving the electrochemical properties of experimental metallic alloys proposed for dental implants. Herein, only studies investigating binary alloys with high potential as implant materials were selected. In this way, it was possible to clearly state the effects of the alloying elements on Ti corrosion kinetics and microstructure.
Zirconium (Zr), tantalum (Ta), niobium (Nb), chromium (Cr), and molybdenum (Mo) are some of the elements normally added to Ti to form a stable and resistant oxide film when in contact with the environment. For example, Ta oxides (mainly Ta2O5) are known to be very stable, and their association with TiO2 improved the structural integrity of the passive film leading to superior resistance to pitting corrosion [55]. Similarly, Mo showed concentration-dependent protection, in which higher concentrations arise the formation of a more compact inner oxide layer at the metal-oxide interface [67]. On the other hand, some elements such as Fe form oxides less stable than TiO2, impairing its protective behavior if added in high concentrations [68].
As seen in Table 1, not only the oxide film is changed when an alloying element is added to Ti. The alloy may go through a variety of phase transformation reactions, which can result in three microstructure phases (α, α+β, and β) with intermetallic variants [69•, 70]. There is no consensus in the literature regarding the best crystalline phase to prevent corrosion. While β crystalline phase is expected to be more resistant to dissolution and stabler than the α-phase [71, 72], the solid solution strengthening effect of the single α-phase in Ti alloys has revealed a better electrochemical behavior than α+β and β alloys [53, 73].
Regarding intermetallic phases, it tends to precipitate by incorporating high concentrations of alloying elements to Ti. Generally, intermetallic compounds will dissolve preferentially on the surface by developing a galvanic cell with the matrix [73,74,75,76,77], which impairs the alloy’s electrochemical stability. In fact, the possible formation of a galvanic couple between Ti and Mg because of their dissimilar potential may accelerate the corrosion processes of Ti–Mg alloys [64]. Thus, single-phase alloys are likely to exhibit better electrochemical properties [78], but when more than one phase and/or diverse crystallographic orientations are present, it is indispensable to achieve grain refinement and an even distribution of the elements [49]. A fine microstructure provides an “enveloping effect” by modifying the cathode/anode area ratio between the intermetallic and the matrix to minimize the galvanic effects and provide corrosion protection of the less noble phase [57, 79]. Also, homogeneous microstructures and greater elemental distributions may result in better corrosion resistance due to the improved stability and durability of the passivation films formed on the matrices in these cases [50, 58, 74, 76, 77, 80]. For instance, the inhomogeneous distribution of the Ti2Ag phase in Ti-Ag alloys resulted in more pores (e.g., imperfections) on the surfaces, favoring crevice corrosion attacks owing to localized disruption of the passive film [59].
The grain refinement of an alloy can be achieved from different approaches. Firstly, alloying elements such as Fe [68], In [60], and Sn [81] have shown a strong role in refining the grain size of the alloy, increasing its corrosion resistance. Another well-known approach to inhibit corrosion on alloy materials by microstructure refinement and homogeneous element distribution is applying alternative manufacturing techniques and thermomechanical/finishing processes [49]. Additive manufacturing or 3D printing (e.g., selective laser melting (SLM), electron beam melting (EBM), laser metal deposition (LMD), selective laser sintering (SLS), binder jetting (BJ), laser engineered net shaping (LENS), and wire arc additive manufacturing (WAAM)) [55, 82,83,84,85,86], as well as finishing (e.g., burnishing, laser surface treatments, and shot penning) [87,88,89], and thermomechanical processing (e.g., aging and annealing) [90, 91] are a set of techniques that have been used to fabricate new alloys with protective properties against corrosion by (i) complete oxidation of alloying elements and growth of a uniform surface film, (ii) formation of defect-free microstructures with refined grain structures, and (iii) homogeneous distribution of alloying elements without solute segregation.
Although only binary Ti alloys are reviewed in Table 1, several other elements have been used to develop corrosion-resistant alloys. Some alloying elements (e.g., V, Al, and Sn) are more commonly associated in ternary, high entropy alloys (HEAs), or compositionally complex alloys (CCAs). The range of elements and combinations is wide. For this reason, researchers are first modeling a well-defined combination of elements and their concentrations by computational tools that consider first-principles calculations (e.g., ab initio, density functional theory) to predict material properties and electrochemical mechanisms before testing it by in vitro and in vivo studies [51, 92, 93]. Although this approach may increase the chance of success of metallic alloys, essentially, studies may have tested the progressive incorporation of an element to alloys empirically [53,54,55, 94,95,96].
Improving the Electrochemical Stability of Dental Implants by Surface Treatments
While the design of new alloys seeks to create a corrosion-resistant dental implant by improving the electrochemical properties of the bulk material, surface treatments are applied to the implant substrate after its manufacturing, aiming to minimize the corrosion damages by avoiding the penetration of corrodents on metal underneath and preventing the electrochemical reactions. Table 2 summarizes the treatment details and outcomes of the main technologies proposed to create a protective behavior against corrosion of dental implants surfaces.
Similar to the corrosive behavior of alloys, the electrochemical stability of coatings is also influenced by their elemental and crystalline composition. For instance, the growth of a TiO2 rutile phase by surface treatments applied to Ti substrate has triggered superior electrochemical stability of the material [104, 111]. In addition, the reinforcement of the oxide layer with homogeneously distributed functional and stable compounds and crystal phases (e.g., TiN, TiH TiO2, Al2O3, SiC) by coating/film deposition technologies has proved to enhance the corrosion performance of the implant material [54, 99, 110, 113]. In this context, Safavi et al. [113] and Ling et al. [119] listed a series of mechanism and ideal criteria that coatings and films deposited by magnetron sputtered and hydrothermal methods need to meet for corrosion inhibition, which may be considered regardless of the surface treatment technology: (i) the formation of stabler oxide films containing TiO2, ZrO2, Nb2O5, Ta2O5, etc. and certain crystallinity potentially contribute to prevent the internal dissolution of the coating due to corrosive attacks; (ii) dense, compact, and defect-free layers can successfully fill the existing porosities of the substrate, preventing the corrosive fluid to reach the surface of the implant; (iii) thick layers may decrease and even mitigate the dissolution of the coatings in the immersion medium; (iv) an improved ability of substrates to form passive layers after coating/film deposition leads to better protective behavior; and (v) a strong bond strength between the coating and the substrate might avoid the coating cracking and peeling off in the body fluid, avoiding local corrosion.
Besides the intrinsic characteristics of the film/coating, it is important to consider the final alterations that the surface treatment will result in the physical-chemical properties of the dental implant that may hinder or improve the material’s electrochemical stability. For example, some researchers have focused on creating a surface with hydrophobic nature to restrict or repeal the electrolyte solution at the surface, preventing liquid penetration through the coating and protecting the underlying substrate from corrosion [114, 117]. On the other hand, a detrimental behavior from the physicochemical alterations provoked by treatment techniques is also possible. For instance, increased surface roughness and surface area may impair the passive film formation and facilitate its damage, favoring pitting corrosion initiation [97,98,99]. Besides, increased electrochemical activity of treated surfaces may be incited by greater wettability, which results in lower contact resistance between the electrode and electrolyte that can have an even more negative outcome if a higher surface area is available for ion transportation [54, 128].
Conclusions and Remarks
Despite the need for further in vitro and in vivo in-depth elucidation regarding the effect and mechanisms of dental implant corrosion products on peri-implant tissue inflammation and systemic health, current evidence displays that there is room for the development of improved strategies toward the reduction of implant corrosion rate targeting real progress from the bench to the clinic. Regardless of the strategy, either designing experimental Ti alloys or developing new treatment surfaces, the aim converts to the same spotlight: to reduce the degradation level of the implants and prevent metal release in the tissue surrounding them to prolong their lifetime. It is evident that the chemical and physical properties are crucial for the electrochemical behavior of the implant material. Thus, developing an alloy or coating/layer for corrosion inhibition is mandatory to investigate these features and consider biological applicability. For instance, incorporating some functional compounds into the substrate may improve the corrosion resistance of the implant material, but it can also be cytotoxic for tissues. On the other hand, although hierarchal structure topography with a greater surface area might improve the biological response of the implant, it may exhibit unwanted effects on the growth and stability of the oxide film, impairing its corrosion properties. The ultimate goal is to find reliable routes to conjugate in the same implant both characteristics, adequate stimulation of the biological tissues without weakening its protective behavior against corrosion. Therefore, based on the data discussed in this review, it can be suggested that an extensive understanding of the involved corrosion mechanism should be the basis for the design of dental implant devices. Full knowledge of the role of corrosion products and better methods to improve the corrosion resistance of dental implants can illuminate how to control peri-implant diseases and achieve safe and long-term implant rehabilitation therapy.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Branemark PI. Osseointegration and its experimental background. J Prosthet Dent. 1983;50:399–410. https://doi.org/10.1016/S0022-3913(83)80101-2.
•Howe M-S, Keys W, Richards D. Long-term (10-year) dental implant survival: a systematic review and sensitivity meta-analysis. J Dent 2019;84:9–21. https://doi.org/10.1016/j.jdent.2019.03.008. (High-level evidence on the long-term survival rate of dental implants.)
Gautam G, Kumar S, Kumar K. Processing of biomaterials for bone tissue engineering: state of the art. Mater Today Proc. 2021. https://doi.org/10.1016/j.matpr.2021.09.459.
Dini C, Costa RC, Sukotjo C, Takoudis CG, Mathew MT, Barão VAR. Progression of bio-tribocorrosion in implant dentistry. Front Mech Eng 2020;6. https://doi.org/10.3389/fmech.2020.00001.
•Revathi A, Borrás AD, Muñoz AI, Richard C, Manivasagam G. Degradation mechanisms and future challenges of titanium and its alloys for dental implant applications in oral environment. Mater Sci Eng C 2017;76:1354–68. https://doi.org/10.1016/j.msec.2017.02.159. (Critical review highlighting current evidence on degradation mechanisms and future prospects for dental implants.)
Souza JGS, Costa Oliveira BE, Bertolini M, Lima CV, Retamal-Valdes B, Faveri M, et al. Titanium particles and ions favor dysbiosis in oral biofilms. J Periodontal Res. 2020;55:258–66. https://doi.org/10.1111/jre.12711.
Barão VAR, Mathew MT, Assunção WG, Yuan JC-C, Wimmer MA, Sukotjo C. Stability of cp-Ti and Ti-6Al-4V alloy for dental implants as a function of saliva pH-an electrochemical study. Clin Oral Implants Res 2012;23:1055–62. https://doi.org/10.1111/j.1600-0501.2011.02265.x.
Chaturvedi TP. Corrosive behaviour of implant biomaterials in oral environment. Mater Technol. 2016;31:689–95. https://doi.org/10.1080/10667857.2016.1213527.
•Mombelli A, Hashim D, Cionca N. What is the impact of titanium particles and biocorrosion on implant survival and complications? A critical review. Clin Oral Implants Res 2018;29:37–53. https://doi.org/10.1111/clr.13305. (Critical review highlighting current evidence on the association between corrosion and biological complications related to dental implants.)
Lugowski SJ, Smith DC, McHugh AD, Van Loon JC. Release of metal ions from dental implant materialsin vivo: determination of Al Co, Cr, Mo, Ni, V, and Ti in organ tissue. J Biomed Mater Res. 1991;25:1443–58. https://doi.org/10.1002/jbm.820251204.
Asri RIM, Harun WSW, Samykano M, Lah NAC, Ghani SAC, Tarlochan F, et al. Corrosion and surface modification on biocompatible metals: a review. Mater Sci Eng C. 2017;77:1261–74. https://doi.org/10.1016/j.msec.2017.04.102.
Pettersson M, Pettersson J, Johansson A, Molin Thorén M. Titanium release in peri-implantitis. J Oral Rehabil. 2019;46:179–88. https://doi.org/10.1111/joor.12735.
•Schwarz F, Derks J, Monje A, Wang H-L. Peri-implantitis. J Clin Periodontol 2018;45:S246–66. https://doi.org/10.1111/jcpe.12954. (Latest consensus report on peri-implant diseases.)
•Romandini M, Lima C, Pedrinaci I, Araoz A, Soldini MC, Sanz M. Prevalence and risk/protective indicators of peri-implant diseases: a university-representative cross-sectional study. Clin Oral Implants Res 2021;32:112–22. https://doi.org/10.1111/clr.13684.(High-level evidence on the prevalence of peri-implant diseases.)
Fisher DS, van Schalkwyk GI, Seedat S, Curran SR, Flanagan RJ. Plasma, oral fluid, and whole-blood distribution of antipsychotics and metabolites in clinical samples. Ther Drug Monit. 2013;35:345–51. https://doi.org/10.1097/FTD.0b013e318283eaf2.
Lehnfeld J, Dukashin Y, Mark J, White GD, Wu S, Katzur V, et al. Saliva and serum protein adsorption on chemically modified silica surfaces. J Dent Res. 2021;100:1047–54. https://doi.org/10.1177/00220345211022273.
Costa RC, Abdo VL, Mendes PHC, Mota-Veloso I, Bertolini M, Mathew MT, et al. Microbial corrosion in titanium-based dental implants: how tiny bacteria can create a big problem? J Bio- Tribo-Corrosion. 2021;7:136. https://doi.org/10.1007/s40735-021-00575-8.
Souza JCM, Apaza-Bedoya K, Benfatti CAM, Silva FS, Henriques B. A comprehensive review on the corrosion pathways of titanium dental implants and their biological adverse effects. Metals (Basel). 2020;10:1272. https://doi.org/10.3390/met10091272.
Virtanen S, Milošev I, Gomez-Barrena E, Trebše R, Salo J, Konttinen YT. Special modes of corrosion under physiological and simulated physiological conditions. Acta Biomater. 2008;4:468–76. https://doi.org/10.1016/j.actbio.2007.12.003.
Fraser BM. Does fluoride cause corrosion of titanium dental implants? Int J Oral Implantol Clin Res. 2018;9:7–10. https://doi.org/10.5005/jp-journals-10012-1179.
Mabilleau G, Bourdon S, Joly-Guillou ML, Filmon R, Baslé MF, Chappard D. Influence of fluoride, hydrogen peroxide and lactic acid on the corrosion resistance of commercially pure titanium. Acta Biomater. 2006;2:121–9. https://doi.org/10.1016/j.actbio.2005.09.004.
Wang ZB, Hu HX, Zheng YG, Ke W, Qiao YX. Comparison of the corrosion behavior of pure titanium and its alloys in fluoride-containing sulfuric acid. Corros Sci. 2016;103:50–65. https://doi.org/10.1016/j.corsci.2015.11.003.
Noguti J, de Oliveira F, Peres RC, Renno ACM, Ribeiro DA. The role of fluoride on the process of titanium corrosion in oral cavity. BioMetals. 2012;25:859–62. https://doi.org/10.1007/s10534-012-9570-6.
Beline T, Garcia CS, Ogawa ES, Marques ISV, Matos AO, Sukotjo C, et al. Surface treatment influences electrochemical stability of cpTi exposed to mouthwashes. Mater Sci Eng C. 2016;59:1079–88. https://doi.org/10.1016/j.msec.2015.11.045.
Chen W-Q, Zhang S-M, Qiu J. Surface analysis and corrosion behavior of pure titanium under fluoride exposure. J Prosthet Dent. 2020;124:239.e1-239.e8. https://doi.org/10.1016/j.prosdent.2020.02.022.
Boere G. Influence of fluoride on titanium in an acidic environment measured by polarization resistance technique. J Appl Biomater. 1995;6:283–8. https://doi.org/10.1002/jab.770060409.
Souza JCM, Barbosa SL, Ariza EA, Henriques M, Teughels W, Ponthiaux P, et al. How do titanium and Ti6Al4V corrode in fluoridated medium as found in the oral cavity? An in vitro study. Mater Sci Eng C. 2015;47:384–93. https://doi.org/10.1016/j.msec.2014.11.055.
Bowen WH, Burne RA, Wu H, Koo H. Oral biofilms: pathogens, matrix, and polymicrobial interactions in microenvironments. Trends Microbiol. 2018;26:229–42. https://doi.org/10.1016/j.tim.2017.09.008.
Souza JGS, Bertolini MM, Costa RC, Nagay BE, Dongari-Bagtzoglou A, Barão VAR. Targeting implant-associated infections: titanium surface loaded with antimicrobial. IScience. 2021;24:102008. https://doi.org/10.1016/j.isci.2020.102008.
Eger M, Sterer N, Liron T, Kohavi D, Gabet Y. Scaling of titanium implants entrains inflammation-induced osteolysis. Sci Rep. 2017;7:39612. https://doi.org/10.1038/srep39612.
Cordeiro JM, Pires JM, Souza JGS, Lima CV, Bertolini MM, Rangel EC, et al. Optimizing citric acid protocol to control implant-related infections: an in vitro and in situ study. J Periodontal Res. 2021;56:558–68. https://doi.org/10.1111/jre.12855.
Barão VAR, Ricomini-Filho AP, Faverani LP, Del Bel Cury AA, Sukotjo C, Monteiro DR, et al. The role of nicotine, cotinine and caffeine on the electrochemical behavior and bacterial colonization to cp-Ti. Mater Sci Eng C. 2015;56:114–24. https://doi.org/10.1016/j.msec.2015.06.026.
Noronha Oliveira M, Schunemann WVH, Mathew MT, Henriques B, Magini RS, Teughels W, et al. Can degradation products released from dental implants affect peri-implant tissues? J Periodontal Res. 2018;53:1–11. https://doi.org/10.1111/jre.12479.
Barão VA, Mathew MT, Assunção WG, Yuan JC, Wimmer MA, Sukotjo C. The role of lipopolysaccharide on the electrochemical behavior of titanium. J Dent Res. 2011;90:613–8. https://doi.org/10.1177/0022034510396880.
Sousa CA, Cordeiro JM, Silva AO, Barão VAR, Faverani LP, Assunção WG. Dynamic action of mouthwashes affects the electrochemical behavior of Ti6Al4V alloy. J Bio Tribo Corros. 2021;7:158. https://doi.org/10.1007/s40735-021-00591-8.
Dragus L, Benea L, Simionescu N, Ravoiu A, Neaga V. Effect of the inflammatory conditions and albumin presence on the corrosion behavior of grade 5 titanium alloy in saliva biological solution. IOP Conf Ser Mater Sci Eng. 2019;572:012005. https://doi.org/10.1088/1757-899X/572/1/012005.
Talha M, Ma Y, Kumar P, Lin Y, Singh A. Role of protein adsorption in the bio corrosion of metallic implants–a review. Colloids Surfaces B Biointerfaces. 2019;176:494–506. https://doi.org/10.1016/j.colsurfb.2019.01.038.
•Kunrath MF, Muradás TC, Penha N, Campos MM. Innovative surfaces and alloys for dental implants: what about biointerface-safety concerns? Dent Mater 2021;37:1447–62. https://doi.org/10.1016/j.dental.2021.08.008. (Critical review highlighting current evidences on the biotribocorrosion performance of alloys and surface treatments for dental implants.)
Kim KT, Eo MY, Nguyen TTH, Kim SM. General review of titanium toxicity. Int J Implant Dent. 2019;5:10. https://doi.org/10.1186/s40729-019-0162-x.
Prestat M, Thierry D. Corrosion of titanium under simulated inflammation conditions: clinical context and in vitro investigations. Acta Biomater. 2021. https://doi.org/10.1016/j.actbio.2021.10.002.
•Suárez-López del Amo F, Garaicoa-Pazmiño C, Fretwurst T, Castilho RM, Squarize CH. Dental implants-associated release of titanium particles: a systematic review. Clin Oral Implants Res 2018;29:1085–100. https://doi.org/10.1111/clr.13372. (Systematic review highlighting in vitro, pre-clinical, and clinical evidences of titanium particles release associated to dental implants.)
Choi MG, Koh HS, Kluess D, O’Connor D, Mathur A, Truskey GA, et al. Effects of titanium particle size on osteoblast functions in vitro and in vivo. Proc Natl Acad Sci. 2005;102:4578–83. https://doi.org/10.1073/pnas.0500693102.
Mine Y, Makihira S, Nikawa H, Murata H, osokawa R, Hiyama A, et al. Impact of titanium ions on osteoblast-, osteoclast- and gingival epithelial-like cells. J Prosthodont Res 2010;54:1–6. https://doi.org/10.1016/j.jpor.2009.07.003.
Wachi T, Shuto T, Shinohara Y, Matono Y, Makihira S. Release of titanium ions from an implant surface and their effect on cytokine production related to alveolar bone resorption. Toxicology. 2015;327:1–9. https://doi.org/10.1016/j.tox.2014.10.016.
•Safioti LM, Kotsakis GA, Pozhitkov AE, Chung WO, Daubert DM. Increased levels of dissolved titanium are associated with peri-implantitis–a cross-sectional study. J Periodontol 2017;88:436–42. https://doi.org/10.1902/jop.2016.160524. (Clinical evidence of possible association between released titanium and peri-implantitis.)
Pettersson M, Kelk P, Belibasakis GN, Bylund D, Molin Thorén M, Johansson A. Titanium ions form particles that activate and execute interleukin-1β release from lipopolysaccharide-primed macrophages. J Periodontal Res. 2017;52:21–32. https://doi.org/10.1111/jre.12364.
•Olmedo DG, Nalli G, Verdú S, Paparella ML, Cabrini RL. Exfoliative cytology and titanium dental implants: a pilot study. J Periodontol 2013;84:78–83. https://doi.org/10.1902/jop.2012.110757. (Clinical evidence of possible association between metal-like particles and peri-implantitis.)
Wylie AH, Kerr JF, Currie AR: Cell death: the significance of apoptosis. In: Bourne GH, Field JM, Jeon KW, editors. International review of cytology. Oxford: Blackwell Science; 2012.
Cordeiro JM, Nagay BE, Mathew MT, Barão VAR: Designing corrosion-resistant alloys. In: Inamuddin RB, Ahamed MI, Asiri AM, editors. Alloy materials and their allied applications. Wiley; 2020. https://doi.org/10.1002/9781119654919.ch2.
Shi Y, Yang B, Liaw PK. Corrosion-resistant high-entropy alloys: a review. Metals. 2017;7:43. https://doi.org/10.3390/met7020043.
Zhang M, Hector LG, Guo Y, Liu M, Qi L. First-principles search for alloying elements that increase corrosion resistance of Mg with second-phase particles of transition metal impurities. Comput Mater Sci. 2019;165:154–66. https://doi.org/10.1016/j.commatsci.2019.04.018.
Henderson JD, Ebrahimi N, Dehnavi V, Guo M, Shoesmith DW, Noël JJ. The role of internal cathodic support during the crevice corrosion of Ni-Cr-Mo alloys. Electrochim Acta. 2018;283:1600–8. https://doi.org/10.1016/j.electacta.2018.07.048.
Cordeiro JM, Beline T, Ribeiro ALR, Rangel EC, da Cruz NC, Landers R, et al. Development of binary and ternary titanium alloys for dental implants. Dent Mater. 2017;33:1244–57. https://doi.org/10.1016/j.dental.2017.07.013.
Cordeiro JM, Faverani LP, Grandini CR, Rangel EC, da Cruz NC, Nociti Junior FH, et al. Characterization of chemically treated Ti-Zr system alloys for dental implant application. Mater Sci Eng C. 2018;92:849–61. https://doi.org/10.1016/j.msec.2018.07.046.
Zhao D, Han C, Li Y, Li J, Zhou K, Wei Q, et al. Improvement on mechanical properties and corrosion resistance of titanium-tantalum alloys in-situ fabricated via selective laser melting. J Alloys Compd. 2019;804:288–98. https://doi.org/10.1016/j.jallcom.2019.06.307.
Han M-K, Kim J-Y, Hwang M-J, Song H-J, Park Y-J. Effect of Nb on the microstructure, mechanical properties, corrosion behavior, and cytotoxicity of Ti-Nb alloys. Materials (Basel). 2015;8:5986–6003. https://doi.org/10.3390/ma8095287.
Zhang E, Ren J, Li S, Yang L, Qin G. Optimization of mechanical properties, biocorrosion properties and antibacterial properties of as-cast Ti–Cu alloys. Biomed Mater. 2016;11:065001. https://doi.org/10.1088/1748-6041/11/6/065001.
Takada Y, Nakajima H, Okuno O, Okabe T. Microstructure and corrosion behavior of binary titanium alloys with beta-stabilizing elements. Dent Mater J. 2001;20:34–52. https://doi.org/10.4012/dmj.20.34.
Chen M, Zhang E, Zhang L. Microstructure, mechanical properties, bio-corrosion properties and antibacterial properties of Ti–Ag sintered alloys. Mater Sci Eng C. 2016;62:350–60. https://doi.org/10.1016/j.msec.2016.01.081.
Romero-Resendiz L, Gómez-Sáez P, Vicente-Escuder A, Amigó-Borrás V. Development of Ti–In alloys by powder metallurgy for application as dental biomaterial. J Mater Res Technol. 2021;11:1719–29. https://doi.org/10.1016/j.jmrt.2021.02.014.
Song H-J, Lee H, Lee J-Y, Moon W-J, Lee W-Y, Park Y-J. Characteristics and oxidation mechanism of thermal oxide on Ti-xCr and Ti-xV (x = 5, 10, 15) alloys. J Alloys Compd. 2020;815:152390. https://doi.org/10.1016/j.jallcom.2019.152390.
Takemoto S, Hattori M, Yoshinari M, Kawada E, Asami K, Oda Y. Corrosion behavior and surface characterization of Ti-20Cr alloy in a solution containing fluoride. Dent Mater J. 2004;23:379–86. https://doi.org/10.4012/dmj.23.379.
Kim J-W, Hwang M-J, Han M-K, Kim Y-G, Song H-J, Park Y-J. Effect of manganese on the microstructure, mechanical properties and corrosion behavior of titanium alloys. Mater Chem Phys. 2016;180:341–8. https://doi.org/10.1016/j.matchemphys.2016.06.016.
Liu Y, Li K, Luo T, Song M, Wu H, Xiao J, et al. Powder metallurgical low-modulus Ti–Mg alloys for biomedical applications. Mater Sci Eng C. 2015;56:241–50. https://doi.org/10.1016/j.msec.2015.06.010.
Qiu KJ, Liu Y, Zhou FY, Wang BL, Li L, Zheng YF, et al. Microstructure, mechanical properties, castability and in vitro biocompatibility of Ti–Bi alloys developed for dental applications. Acta Biomater. 2015;15:254–65. https://doi.org/10.1016/j.actbio.2015.01.009.
Oliveira NTC, Guastaldi AC. Electrochemical behavior of Ti–Mo alloys applied as biomaterial. Corros Sci. 2008;50:938–45. https://doi.org/10.1016/j.corsci.2007.09.009.
Bolat G, Mareci D, Chelariu R, Izquierdo J, González S, Souto RM. Investigation of the electrochemical behaviour of TiMo alloys in simulated physiological solutions. Electrochim Acta. 2013;113:470–80. https://doi.org/10.1016/j.electacta.2013.09.116.
Niu J, Guo Y, Li K, Liu W, Dan Z, Sun Z, et al. Improved mechanical, bio-corrosion properties and in vitro cell responses of Ti-Fe alloys as candidate dental implants. Mater Sci Eng C. 2021;122:111917. https://doi.org/10.1016/j.msec.2021.111917.
•Cordeiro JM, Barão VAR. Is there scientific evidence favoring the substitution of commercially pure titanium with titanium alloys for the manufacture of dental implants? Mater Sci Eng C 2017;71:1201–15. https://doi.org/10.1016/j.msec.2016.10.025. (Critical review highlighting the current evidence on overall properties of titanium and its alloys for the manufacturing of dental implants.)
Liu X, Chen S, Tsoi JKH, Matinlinna JP. Binary titanium alloys as dental implant materials-a review. Regen Biomater. 2017;4:315–23. https://doi.org/10.1093/rb/rbx027.
Chen J-R, Tsai W-T. In situ corrosion monitoring of Ti–6Al–4V alloy in H2SO4/HCl mixed solution using electrochemical AFM. Electrochim Acta. 2011;56:1746–51. https://doi.org/10.1016/j.electacta.2010.10.024.
Dai N, Zhang L-C, Zhang J, Chen Q, Wu M. Corrosion behavior of selective laser melted Ti-6Al-4 V alloy in NaCl solution. Corros Sci. 2016;102:484–9. https://doi.org/10.1016/j.corsci.2015.10.041.
Cordeiro JM, Nagay BE, Ribeiro ALR, da Cruz NC, Rangel EC, Fais LMG, et al. Functionalization of an experimental Ti-Nb-Zr-Ta alloy with a biomimetic coating produced by plasma electrolytic oxidation. J Alloys Compd. 2019;770:1038–48. https://doi.org/10.1016/j.jallcom.2018.08.154.
Atapour M, Pilchak AL, Frankel GS, Williams JC. Corrosion behavior of β titanium alloys for biomedical applications. Mater Sci Eng C. 2011;31:885–91. https://doi.org/10.1016/j.msec.2011.02.005.
Zeng R, Kainer KU, Blawert C, Dietzel W. Corrosion of an extruded magnesium alloy ZK60 component—The role of microstructural features. J Alloys Compd. 2011;509:4462–9. https://doi.org/10.1016/j.jallcom.2011.01.116.
Jia H, Feng X, Yang Y. Microstructure and corrosion resistance of directionally solidified Mg-2 wt.% Zn alloy. Corros Sci 2017;120:75–81. https://doi.org/10.1016/j.corsci.2017.02.023.
Guo Y, Bataev I, Georgarakis K, Jorge AM, Nogueira RP, Pons M, et al. Ni- and Cu-free Ti-based metallic glasses with potential biomedical application. Intermetallics. 2015;63:86–96. https://doi.org/10.1016/j.intermet.2015.04.004.
Sefer B, Virtanen S. Electrochemical and corrosion study of as-cast NixAly intermetallic alloys: influence of alloy composition and electrolyte pH. Corros Sci. 2019;150:127–35. https://doi.org/10.1016/j.corsci.2019.01.031.
Osório WR, Cremasco A, Andrade PN, Garcia A, Caram R. Electrochemical behavior of centrifuged cast and heat treated Ti–Cu alloys for medical applications. Electrochim Acta. 2010;55:759–70. https://doi.org/10.1016/j.electacta.2009.09.016.
Zhao Y, Xing S, Wang L, Sun Y, Liu H, Zhan K, et al. Roles of growth mechanisms of Ni deposits on corrosion behaviors of NixAlyTi composite coatings. Appl Surf Sci. 2019;492:177–88. https://doi.org/10.1016/j.apsusc.2019.06.188.
Tsao LC. Effect of Sn addition on the corrosion behavior of Ti–7Cu–Sn cast alloys for biomedical applications. Mater Sci Eng C. 2015;46:246–52. https://doi.org/10.1016/j.msec.2014.10.037.
Sander G, Tan J, Balan P, Gharbi O, Feenstra DR, Singer L, et al. Corrosion of additively manufactured alloys: a review. Corrosion. 2018;74:1318–50. https://doi.org/10.5006/2926.
Singh N, Hameed P, Ummethala R, Manivasagam G, Prashanth KG, Eckert J. Selective laser manufacturing of Ti-based alloys and composites: impact of process parameters, application trends, and future prospects. Mater Today Adv. 2020;8:100097. https://doi.org/10.1016/j.mtadv.2020.100097.
Lee WJ, Kim J, Park HW. Improved corrosion resistance of Mg alloy AZ31B induced by selective evaporation of Mg using large pulsed electron beam irradiation. J Mater Sci Technol. 2019;35:891–901. https://doi.org/10.1016/j.jmst.2018.12.004.
Wang JC, Liu YJ, Qin P, Liang SX, Sercombe TB, Zhang LC. Selective laser melting of Ti–35Nb composite from elemental powder mixture: microstructure, mechanical behavior and corrosion behavior. Mater Sci Eng A. 2019;760:214–24. https://doi.org/10.1016/j.msea.2019.06.001.
Marattukalam JJ, Singh AK, Datta S, Das M, Balla VK, Bontha S, et al. Microstructure and corrosion behavior of laser processed NiTi alloy. Mater Sci Eng C Mater Biol Appl. 2015;57:309–13. https://doi.org/10.1016/j.msec.2015.07.067.
Wu S, Wang S, Wang G, Yu X, Liu W, Chang Z, et al. Microstructure, mechanical and corrosion properties of magnesium alloy bone plate treated by high-energy shot peening. Trans Nonferrous Met Soc China. 2019;29:1641–52. https://doi.org/10.1016/S1003-6326(19)65071-5.
Salahshoor M, Li C, Liu ZY, Fang XY, Guo YB. Surface integrity and corrosion performance of biomedical magnesium-calcium alloy processed by hybrid dry cutting-finish burnishing. J Mech Behav Biomed Mater. 2018;78:246–53. https://doi.org/10.1016/j.jmbbm.2017.11.026.
Vasilescu C, Drob SI, Calderon Moreno JM, Osiceanu P, Popa M, Vasilescu E, et al. Long-term corrosion resistance of new Ti–Ta–Zr alloy in simulated physiological fluids by electrochemical and surface analysis methods. Corros Sci. 2015;93:310–23. https://doi.org/10.1016/j.corsci.2015.01.038.
Panigrahi P, Liao Y, Mathew MT, Fischer A, Wimmer MA, Jacobs JJ, et al. Intergranular pitting corrosion of CoCrMo biomedical implant alloy. J Biomed Mater Res B Appl Biomater. 2014;102:850–9. https://doi.org/10.1002/jbm.b.33067.
Janbozorgi M, Karimi Taheri K, Karimi Taheri A. Microstructural evolution, mechanical properties, and corrosion resistance of a heat-treated Mg alloy for the bio-medical application. J Magnes Alloy. 2019;7:80–9. https://doi.org/10.1016/j.jma.2018.11.002.
Ma H, Chen X-Q, Li R, Wang S, Dong J, Ke W. First-principles modeling of anisotropic anodic dissolution of metals and alloys in corrosive environments. Acta Mater. 2017;130:137–46. https://doi.org/10.1016/j.actamat.2017.03.027.
Gutiérrez Moreno JJ, Bönisch M, Panagiotopoulos NT, Calin M, Papageorgiou DG, Gebert A, et al. Ab-initio and experimental study of phase stability of Ti-Nb alloys. J Alloys Compd. 2017;696:481–9. https://doi.org/10.1016/j.jallcom.2016.11.231.
Feng Z, Dong H, Kang J, Li J, Zhang X, Ma M, et al. Study on the correlation between microstructures and corrosion properties of novel ZrTiAlV alloys. Mater Sci Eng C. 2019;101:92–102. https://doi.org/10.1016/j.msec.2019.03.076.
Grimm M, Lohmüller A, Singer RF, Virtanen S. Influence of the microstructure on the corrosion behaviour of cast Mg-Al alloys. Corros Sci. 2019;155:195–208. https://doi.org/10.1016/j.corsci.2019.04.024.
Guo S, Lu Y, Wu S, Liu L, He M, Zhao C, et al. Preliminary study on the corrosion resistance, antibacterial activity and cytotoxicity of selective-laser-melted Ti6Al4V-xCu alloys. Mater Sci Eng C Mater Biol Appl. 2017;72:631–40. https://doi.org/10.1016/j.msec.2016.11.126.
Ogawa ES, Matos AO, Beline T, Marques ISV, Sukotjo C, Mathew MT, et al. Surface-treated commercially pure titanium for biomedical applications: electrochemical, structural, mechanical and chemical characterizations. Mater Sci Eng C. 2016;65:251–61. https://doi.org/10.1016/j.msec.2016.04.036.
Barranco V, Escudero ML, García-Alonso MC. 3D, chemical and electrochemical characterization of blasted TI6Al4V surfaces: its influence on the corrosion behaviour. Electrochim Acta. 2007;52:4374–84. https://doi.org/10.1016/j.electacta.2006.12.031.
Cordeiro JM, Pantaroto HN, Paschoaleto EM, Rangel EC, da Cruz NC, Sukotjo C, et al. Synthesis of biofunctional coating for a TiZr alloy: surface, electrochemical, and biological characterizations. Appl Surf Sci. 2018;452:268–78. https://doi.org/10.1016/j.apsusc.2018.05.044.
Mohammad NF, Ahmad RN, Mohd Rosli NL, Abdul Manan MS, Marzuki M, Wahi A. Sol gel deposited hydroxyapatite-based coating technique on porous titanium niobium for biomedical applications: a mini review. Mater Today Proc. 2021;41:127–35. https://doi.org/10.1016/j.matpr.2020.11.1023.
Ansari Z, Kalantar M, Kharaziha M, Ambrosio L, Raucci MG. Polycaprolactone/fluoride substituted-hydroxyapatite (PCL/FHA) nanocomposite coatings prepared by in-situ sol-gel process for dental implant applications. Prog Org Coatings. 2020;147:105873. https://doi.org/10.1016/j.porgcoat.2020.105873.
El hadad AA, García-Galván FR, Mezour MA, Hickman GJ, Soliman IE, Jiménez-Morales A, et al. Organic-inorganic hybrid coatings containing phosphorus precursors prepared by sol–gel on Ti6Al4V alloy: electrochemical and in-vitro biocompatibility evaluation. Prog Org Coatings 2020;148:105834. https://doi.org/10.1016/j.porgcoat.2020.105834.
Chen S, Zhang C, Xiao D, Shi F, Liu K, Wan Y, et al. Magnesium-incorporated sol-gel Ta2O5 coating on Ti6Al4V and in vitro biocompatibility. Surf Coatings Technol. 2021;426:127769. https://doi.org/10.1016/j.surfcoat.2021.127769.
Marques I da SV, Barão VAR, Cruz NC da, Yuan JC-C, Mesquita MF, Ricomini-Filho AP, et al. Electrochemical behavior of bioactive coatings on cp-Ti surface for dental application. Corros Sci 2015;100:133–46. https://doi.org/10.1016/j.corsci.2015.07.019.
Beline T, Marques I da SV, Matos AO, Ogawa ES, Ricomini-Filho AP, Rangel EC, et al. Production of a biofunctional titanium surface using plasma electrolytic oxidation and glow-discharge plasma for biomedical applications. Biointerphases 2016;11:011013. https://doi.org/10.1116/1.4944061.
Kaluđerović MR, Schreckenbach JP, Graf H-L. Titanium dental implant surfaces obtained by anodic spark deposition-from the past to the future. Mater Sci Eng C Mater Biol Appl. 2016;69:1429–41. https://doi.org/10.1016/j.msec.2016.07.068.
Höhlinger M, Heise S, Wagener V, Boccaccini AR, Virtanen S. Developing surface pre-treatments for electrophoretic deposition of biofunctional chitosan-bioactive glass coatings on a WE43 magnesium alloy. Appl Surf Sci. 2017;405:441–8. https://doi.org/10.1016/j.apsusc.2017.02.049.
Tabesh E, Salimijazi HR, Kharaziha M, Mahmoudi M, Hejazi M. Development of an in-situ chitosan-copper nanoparticle coating by electrophoretic deposition. Surf Coatings Technol. 2019;364:239–47. https://doi.org/10.1016/j.surfcoat.2019.02.040.
Fardi SR, Khorsand H, Askarnia R, Pardehkhorram R, Adabifiroozjaei E. Improvement of biomedical functionality of titanium by ultrasound-assisted electrophoretic deposition of hydroxyapatite-graphene oxide nanocomposites. Ceram Int. 2020;46:18297–307. https://doi.org/10.1016/j.ceramint.2020.05.049.
Beline T, de Almeida AB, Azevedo Neto NF, Matos AO, Ricomini-Filho AP, Sukotjo C, et al. β-Ta2O5 thin film for implant surface modification triggers superior anti-corrosion performance and cytocompatibility of titanium. Appl Surf Sci. 2020;520:146326. https://doi.org/10.1016/j.apsusc.2020.146326.
Pantaroto HN, Cordeiro JM, Pereira LT, de Almeida AB, Nociti Junior FH, Rangel EC, et al. Sputtered crystalline TiO2 film drives improved surface properties of titanium-based biomedical implants. Mater Sci Eng C. 2021;119: 111638. https://doi.org/10.1016/j.msec.2020.111638.
Bao Y, Wang W, Cui W, Qin G. Corrosion resistance and antibacterial activity of Ti-N-O coatings deposited on dental titanium alloy. Surf Coatings Technol. 2021;419:127296. https://doi.org/10.1016/j.surfcoat.2021.127296.
Safavi MS, Surmeneva MA, Surmenev RA, Khalil-Allafi J. RF-magnetron sputter deposited hydroxyapatite-based composite & multilayer coatings: a systematic review from mechanical, corrosion, and biological points of view. Ceram Int. 2021;47:3031–53. https://doi.org/10.1016/j.ceramint.2020.09.274.
Souza JGS, Bertolini M, Costa RC, Cordeiro JM, Nagay BE, de Almeida AB, et al. Targeting pathogenic biofilms: newly developed superhydrophobic coating favors a host-compatible microbial profile on the titanium surface. ACS Appl Mater Interfaces. 2020;12:10118–29. https://doi.org/10.1021/acsami.9b22741.
Tyczkowski J, Kierzkowska-Pawlak H, Kapica R, Balcerzak J, Sielski J. Cold plasma−a promising tool for the production of thin-film nanocatalysts. Catal Today. 2019;337:44–54. https://doi.org/10.1016/j.cattod.2019.03.037.
Ting W-T, Chen K-S, Wang M-J. Dense and anti-corrosion thin films prepared by plasma polymerization of hexamethyldisilazane for applications in metallic implants. Surf Coatings Technol. 2021;410:126932. https://doi.org/10.1016/j.surfcoat.2021.126932.
Singh S, Pandey KK, Islam A, Keshri AK. Corrosion behaviour of plasma sprayed graphene nanoplatelets reinforced hydroxyapatite composite coatings in simulated body fluid. Ceram Int. 2020;46:13539–48. https://doi.org/10.1016/j.ceramint.2020.02.139.
Bansal P, Singh G, Sidhu HS. Investigation of corrosion behavior and surface properties of plasma sprayed HA/Sr reinforced coatings on CoCr alloys. Mater Chem Phys. 2020;253:123330. https://doi.org/10.1016/j.matchemphys.2020.123330.
Ling L, Cai S, Li Q, Sun J, Bao X, Xu G. Recent advances in hydrothermal modification of calcium phosphorus coating on magnesium alloy. J Magnes Alloy. 2021. https://doi.org/10.1016/j.jma.2021.05.014.
Xi Z, Wu Y, Xiang S, Sun C, Wang Y, Yu H, et al. Corrosion resistance and biocompatibility assessment of a biodegradable hydrothermal-coated Mg–Zn–Ca alloy: an in vitro and in vivo study. ACS Omega. 2020;5:4548–57. https://doi.org/10.1021/acsomega.9b03889.
Wu H, Xi K, Xiao S, Qasim AM, Fu RKY, Shi K, et al. Formation of self-layered hydrothermal coating on magnesium aided by titanium ion implantation: synergistic control of corrosion resistance and cytocompatibility. Surf Coatings Technol. 2020;401:126251. https://doi.org/10.1016/j.surfcoat.2020.126251.
Guo Z, Pang X, Yan Y, Gao K, Volinsky AA, Zhang T-Y. CoCrMo alloy for orthopedic implant application enhanced corrosion and tribocorrosion properties by nitrogen ion implantation. Appl Surf Sci. 2015;347:23–34. https://doi.org/10.1016/j.apsusc.2015.04.054.
Luiz LA, Kurelo BCES, de Souza GB, de Andrade J, Marino CEB. Effect of nitrogen plasma immersion ion implantation on the corrosion protection mechanisms of different stainless steels. Mater Today Commun. 2021;28:102655. https://doi.org/10.1016/j.mtcomm.2021.102655.
Huang H-H, Shiau D-K, Chen C-S, Chang J-H, Wang S, Pan H, et al. Nitrogen plasma immersion ion implantation treatment to enhance corrosion resistance, bone cell growth, and antibacterial adhesion of Ti-6Al-4V alloy in dental applications. Surf Coatings Technol. 2019;365:179–88. https://doi.org/10.1016/j.surfcoat.2018.06.023.
Guzmán E, Rubio RG, Ortega F. A closer physico-chemical look to the layer-by-layer electrostatic self-assembly of polyelectrolyte multilayers. Adv Colloid Interface Sci. 2020;282:102197. https://doi.org/10.1016/j.cis.2020.102197.
Mott R, Priefer R. Multilayering as a solution to medical device failure. Colloids Surfaces B Biointerfaces. 2020;193:111154. https://doi.org/10.1016/j.colsurfb.2020.111154.
Farhat TR, Schlenoff JB. Corrosion control using polyelectrolyte multilayers. Electrochem Solid-State Lett. 2002;5:B13. https://doi.org/10.1149/1.1452484.
Costa RC, Souza JGS, Cordeiro JM, Bertolini M, de Avila ED, Landers R, et al. Synthesis of bioactive glass-based coating by plasma electrolytic oxidation: untangling a new deposition pathway toward titanium implant surfaces. J Colloid Interface Sci. 2020;579:680–98. https://doi.org/10.1016/j.jcis.2020.06.102.
Funding
This study is partially supported by the São Paulo Research Foundation (FAPESP) (#2017/01320-0 to J.M.C, 2019/17238-6 to B.E.N., and 2020/05231-4 to V.A.R.B) and the Conselho Nacional de Desenvolvimento Científico e Tecnológico – Brazil (CNPq) (#304853/2018-60 to V.A.R.B).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Dental Restorative Materials
Bruna E. Nagay and Jairo M. Cordeiro share the position of the first authors.
Rights and permissions
About this article
Cite this article
Nagay, B.E., Cordeiro, J.M. & Barao, V.A.R. Insight Into Corrosion of Dental Implants: From Biochemical Mechanisms to Designing Corrosion-Resistant Materials. Curr Oral Health Rep 9, 7–21 (2022). https://doi.org/10.1007/s40496-022-00306-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40496-022-00306-z