Abstract
Purpose of the review
The purpose of this review is to critically assess the evidence for exercise as an adjunct intervention for major depressive disorder and bipolar disorder, chronic conditions characterized by frequent comorbid conditions as well as interepisodic symptoms with poor quality of life and impaired functioning. Individuals with these mood disorders are at higher risk of cardiovascular disease and premature death in part because of increased rates of obesity, inactivity, and diabetes mellitus compared to the general population. Exercise may not only mitigate the increased risk of cardiovascular disease, but could also potentially improve the long term outcomes of mood disorders.
Recent findings
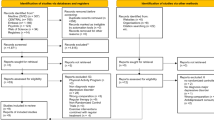
We conducted a literature review on the impact of exercise on mood disorders and associated comorbid conditions as well as possible biological mechanisms. We found that exercise impacts both the physical health parameters of mood disorders as well as mental health outcomes. Exercise also positively impacts conditions frequently comorbid with mood disorders (i.e. anxiety, pain, and insomnia). There are multiple candidate biomarkers for exercise, with brain-derived neurotrophic factor and oxidative stress as two main promising components of exercise’s anti-depressant effect.
Summary
Exercise appears to be a promising adjunct treatment for mood disorders. We conclude with recommendations for future research of exercise as an adjunct intervention for mood disorders.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen H. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012;21(3):169–84.
Merikangas KR, Hagop AS, Angst J, Greenber PE, Hirschfeld RMA, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the national comorbidity survey replication. Arch Gen Psychiatry. 2007;64(5):543–52.
Rapaport MH, Clary C, Fayyad R, Endicott J. Quality-of-life impairment in depressive and anxiety disorders. Am J Psychiatry. 2005;162(6):1171–8.
Zimmerman M, Chelminski I, McDermut W. Major depressive disorder and axis I diagnostic comorbidity. J Clin Psychiatry. 2002;63(3):187–93.
Hirschfeld RMA. The comorbidity of major depression and anxiety disorders-recognition and management in primary care. Prim Care Companion J Clin Psychiatry. 2001;3(6):244–54.
Forty L, Ulanova A, Jones L, Jones I, Gordon-Smith K, Fraser C, et al. Comorbid medical illness in bipolar disorder. Br J Psychiatry. 2014;205:465–72.
Vancampfort D, Vansteelandt K, Correll CU, Mitchell AJ, De Herdt A, Sienaert P, et al. Metabolic syndrome and metabolic abnormalities in bipolar disorder: a meta-analysis of prevalence rates and moderators. Am J Psychiatr. 2013:170(3).
Goldstein BI, Carnethon MR, Matthews KA, McIntyre RS, Miller GE, et al. Major depressive disorder and bipolar disorder predispose youth to accelerated atherosclerosis and early cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132(10):965–86.
Teychenne M, Ball K, Salmon J. Sedentary behavior and depression among adults: a review. Int J Behav Med. 2010;17(4):246–54.
Vancampfort D, Firth J, Schuch F, Rosenbaum S, De Hert M, Mugisha J, et al. Physical activity and sedentary behavior in people with bipolar disorder: a systematic review and meta-analysis. J Affect Disord. 2016;201:145–52.
Fava M. Weight gain and antidepressants. J Clin Psychiatry. 2000;61(suppl 11):1,478-41.
Baptista T, Teneud L, Contreras Q, Alastre T, Burguera JL, De Burguera M, et al. Lithium and body weight gain. Pharmacopsychiatry. 1995;28(2):35–44.
Janney CA, Fagiolini A, Swartz HA, Jakicic JM, Holleman RG, Richardson CR. Are adults with bipolar disorder active? Objectively measured physical activity and sedentary behavior using accelerometry. J Affect Disord. 2014;152-154:498–504.
Elmslie JL, Mann JI, Silverstone JT, Williams SM, Romans SE. Determinants of overweight and obesity in patients with bipolar disorder. J Clin Psychiatry. 2001;62(6):486–91.
Killbourne AM, Rofey DL, McCarthy JF, Post EP, Welsh D, Blow FC. Nutrition and exercise behavior among patients with bipolar disorder. Bipolar Disord. 2007;9(5):443–52.
Fagiolini A, Goracci A. The effects of undertreated chronic medical illnesses in patients with severe mental disorders. J Clin Psychiatry. 2009;70(suppl 3):1,478-29.
Perlis RH, Ostacher MJ, Patel JK, Marangell LB, Zhang H, Wisniewski SR, et al. Predictors of recurrence in bipolar disorder: primary outcomes from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Am J Psychiatr. 2006;163(2):217–24.
Fava M, Davidson KG. Definition and epidemiology of treatment-resistant depression. Psychiatr Clin N Am. 1996;19(2):179–200.
Stathopoulou G, Powers MB, Berry AC, Smits JAJ, Otto MW. Exercise interventions for mental health: a quantitative and qualitative review. Clin Psychol Sci Pract. 2006;13(2):179–93.
Schuch FB, Vancampfort D, Rosenbaum S, Richards J, Ward PB, Stubbs B. Exercise improves physical and psychological quality of life in people with depression: a meta-analysis including the evaluation of control group response. Psychiatry Res. 2016;241:47–54.
Szuhany KL, Smits JAJ, Asmundson GJG, Otto MW. Exercise for mood and anxiety disorders: a review of efficacy, mechanisms, and barriers. New York: Oxford University Press; 2014.
Melo MCA, Daher EDF, Albuquerque SGC, de Bruin VMS. Exercise in bipolar patients: a systematic review. J Affect Disord. 2016;198:32–8.
Blumenthal JA, Babyak MA, Doraiswamy PM, Watkins L, Hoffman BM, Barbour KA, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med. 2007;69(7):587.
Merom D, Phongsavan P, Wagner R, Chey T, Marnane C, Steel Z, et al. Promoting walking as an adjunct intervention to group cognitive behavioral therapy for anxiety disorders: a pilot group randomized trial. J Anxiety Disord. 2008;22(6):959–68.
Kruisdijk FR, Hendriksen IJM, Tak ECPM, Beekman ATF, Hopman-Rock M. Effect of running therapy on depression (EFFORT-D). Design of a randomised controlled trial in adult patients [ISRCTN 1894]. BMC Public Health. 2012;12(1):1–9.
Ng F, Dodd S, Berk M. The effects of physical activity in the acute treatment of bipolar disorder: a pilot study. J Affect Disord. 2007;101(1):259–62. An important study that showed changes in mood, anxiety, and stress after an exercise intervention.
Thomson D, Alyna T, Lauder S, Gigler ME, Berk L, Singh AB, et al. A brief review of exercise, bipolar disorder, and mechanistic pathways. Front Psychol. 2015;6(147):1–10.
Sylvia, LG, Salcedo S, Bernstein EE, Baek JH, Nierenberg AA, Deckersbach T. Nutrition, exercise, and wellness treatment in bipolar disorder: feasibility, acceptability and preliminary efficacy. Int J Bipolar Disord. 2013;1(24):1–7. One of very few studies using a novel exercise intervention in bipolar individuals.
El-Rafie MM, Khafagy GM, Gamal MG. Effect of aerobic exercise during pregnancy on antenatal depression. Int J Women's Health. 2016;8:53.
Siqueira CC, Valiengo LL, Carvalho AF, Santos-Silva PR, Missio G, de Sousa RT, et al. Antidepressant efficacy of adjunctive aerobic activity and associated biomarkers in major depression: a 4-week, randomized, single-blind, controlled clinical trial. PLoS ONE. 2016;11(5):e0154195.
Ellingson LD, Stegner AJ, Schwabacher IJ, Koltyn KF, Cook DB. Exercise strengthens central nervous system modulation of pain in fibromyalgia. Brain Sci. 2016;6(1):8.
Bloomer RJ, Goldfarb AH. Anaerobic exercise and oxidative stress: a review. Can J Appl Physiol. 2004;29(3):245–63.
Fernandes G, Jennings F, Cabral MVN, Buosi ALP, Natour J. Swimming improves pain and functional capacity of patients with fibromyalgia: a randomized controlled trial. Arch Phys Med Rehabil. 2016; p. in press.
Norris R, Carroll D, Cochrane R. The effects of aerobic and anaerobic training on fitness, blood pressure, and psychological stress and well-being. J Psychosom Res. 1990;34(4):367–75.
Mathers C, Fat DM, Boerma JT. The global burden of disease: 2004 Update. 2008: World Health Organization.
Ishak WW, Greenberg JM, Cohen RM. Predicting relapse in major depressive disorder using patient-reported outcomes of depressive symptom severity, functioning, and quality of life in the individual burden of illness index for depression (IBI-D). J Affect Disord. 2013;151(1):59–65.
Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: efficacy and dose response. Am J Prev Med. 2005;28(1):1–8. One of very few randomized clinical trial investigating the optimal dose of exercise.
Daley A. Exercise and depression: a review of reviews. J Clin Psychol Med Settings. 2008;15(2):140–7.
Lawlor DA, Hopker SW. The effectiveness of exercise as an intervention in the management of depression: systematic review and meta-regression analysis of randomised controlled trials. Br Med J. 2001;322(7289):763.
Mota-Pereira J, Carvalho S, Silverio J, Fonte D, Pizarro A, Teixeira J, et al. Moderate physical exercise and quality of life in patients with treatment-resistant major depressive disorder. J Psychiatr Res. 2011;45(12):1657–9.
Herring MP, Puetz TW, O'Connor PJ, Dishman RK. Effect of exercise training on depressive symptoms among patients with a chronic illness: a systematic review and meta-analysis of randomized controlled trials. Arch Intern Med. 2012;172(2):101–11.
Gill A, Womack R, Safranek S. Does exercise alleviate symptoms of depression? Clinical Inquiries, 2010 (MU). 2010.
Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiatry Med. 2011;41(1):15–28.
Rethorst CD, Trivedi MH. Evidence-based recommendations for the prescription of exercise for major depressive disorder. J Psychiatr Pract. 2013;19(3):204–12.
Seime RJ, Vickers KS. The challenges of treating depression with exercise: from evidence to practice. Clin Psychol Sci Pract. 2006;13(2):194–7.
Vancampfort D, Sienaert P, Wyckaert S, De Hert M, Stubbs B, Soundy A, et al. Health-related physical fitness in patients with bipolar disorder vs. healthy controls: an exploratory study. J Affect Disord. 2015;177:22–7.
Proudfoot J, Whitton A, Parker G, Doran J, Manicavasagar V, Delmas K. Triggers of mania and depression in young adults with bipolar disorder. J Affect Disord. 2012;143(1):196–202.
Amati F, Dubé JJ, Coen PM, Stefanovic-Racic M, Toledo FG, Goodpaster BH. Physical inactivity and obesity underlie the insulin resistance of aging. Diabetes Care, 2009. in press.
Wright KA, Everson-Hock ES, Taylor AH. The effects of physical activity on physical and mental health among individuals with bipolar disorder: a systematic review. Ment Health and Phys Act. 2009;2(2):86–94.
Ströhle A, Höfler M, Pfister H, Muller A, Hoyer J, Wittchen H, et al. Physical activity and prevalence and incidence of mental disorders in adolescents and young adults. Psychol Med. 2007;37(11):1657–66.
Hays AE. Effect of an acute bout of aerobic exercise on dehydroepiandrosterone sulphate (DHEAS) in clinically diagnosed bipolar subjects. 2007. University of Pittsburgh.
Edenfield TM. Exercise and mood: exploring the role of exercise in regulating stress reactivity in bipolar disorder. Dissertation Abstracts International: Section B: The Sciences and Engineering. 2008. 68(8-B): p. 5566.
Sylvia LG, Salcedo S, Berinstein EE, Baek JH, Nierenberg AA, Deckersbach T. Nutrition, exercise, and wellness treatment in bipolar disorder: proof of concept for a consolidated intervention. Int J Bipolar Disord. 2013;1(1):1–7.
Harvey AG. Sleep and circadian rhythms in bipolar disorder: seeking synchrony, harmony, and regulation. Am J Psychiatr. 2008;165(7):820–9.
Grandin LD, Alloy LB, Abramson LY. The social zeitgeber theory, circadian rhythms, and mood disorders: review and evaluation. Clin Psychol Rev. 2006;26(6):679–94.
Edgar DM, Dement WC. Regularly scheduled voluntary exercise synchronizes the mouse circadian clock. Am J Phys Regul Integr Comp Phys. 1991;261(4):R928–33.
Escames G, Ozturk G, Bano Otalora B, Pozo MJ, Madrid JA, Reiter RJ, et al. Exercise and melatonin in humans: reciprocal benefits. J Pineal Res. 2012;52(1):1–11.
Solberg LC, Horton TH, Turek FW. Circadian rhythms and depression: effects of exercise in an animal model. Am J Phys Regul Integr Comp Phys. 1999;276(1):R152–61.
King AC, Pruitt LA, Woo S, Castro CM, Ahn DK, Vitiello MV, et al. Effects of moderate-intensity exercise on polysomnographic and subjective sleep quality in older adults with mild to moderate sleep complaints. J Gerontol Ser A Biol Med Sci. 2008;63(9):997–1004.
McGlinchey EL, Gershon A, Eidelman P, Kaplan KA, Harvey AG. Physical activity and sleep: day-to-day associations among individuals with and without bipolar disorder. Ment Health and Phys Act. 2014;7(3):183–90.
Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: a meta-analytic review. J Behav Med. 2015;38(I):427–49.
Herring MP, Kline CE, O'Connor PJ. Effects of exercise on sleep among young women with Generalized Anxiety Disorder. Ment Health and Phys Act. 2015;9:59–66.
Simon NM, Otto MW, Wisniewski SR, Fossey M, Sagduyu K, Frank E, et al. Anxiety disorder comorbidity in bipolar disorder patients: data from the first 500 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Am J Psychiatr. 2004;161(12):2222–9.
Fava M, Rankin MA, Wright EC, Alpert JE, Nierenberg AA, Pava J, et al. Anxiety disorders in major depression. Compr Psychiatry. 2000;41(2):97–102.
McElroy SL, Altshuler LL, Suppes T, Keck PE, Frye MA, Denicoff KD, et al. Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. Am J Psychiatr. 2001;158(3):420–6.
Bakish D. The patient with comorbid depression and anxiety: the unmet need. J Clin Psychiatr. 1999;60(6):20–4.
Coryell W, Noyes R, House JD. Mortality among outpatients with anxiety disorders. Am J Psychiatr. 1986;143(4):508–10.
Physical activity reduces stress. 6/24/2016]; Available from: http://www.adaa.org/understanding-anxiety/related-illnesses/other-related-conditions/stress/physical-activity-reduces-st.
Asmundson GJG, Fetzner MG, DeBoer LB, Powers MB, Otto MW, Smits JAJ. Let's get physical: a contemporary review of the anxiolytic effects of exercise for anxiety and its disorders. Depression Anxiety. 2013;30(4):362–73.
DeBoer LB, Powers MB, Utschig AC, Otto MW, Smits JAJ. Exploring exercise as an avenue for the treatment of anxiety disorders. Expert Rev Neurother. 2012;12(8):1011–22.
Broocks A, Bandelow B, Pekrun G, George A, Meyer T, Bartmann U, et al. Comparison of aerobic exercise, clomipramine, and placebo in the treatment of panic disorder. Am J Psychiatry, 1998.
Szuhany KL, Smits JAJ, Asmundson GJG, Otto MW. Exercise for mood and anxiety disorders: a review of efficacy, mechanisms, and barriers. Oxford Handbooks Online; 2014. pp. 1–22.
Wipfli BM, Rethorst CD, Landers DM. The anxiolytic effects of exercise: a meta-analysis of randomized trials and dose-response analysis. J Sport Exerc Psychol. 2008;30(4):392.
Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163(20):2433–45.
Stubbs B, Eggermont L, Mitchell AJ, De Hert M, Correll CU, Soundy A, et al. The prevalence of pain in bipolar disorder: a systematic review and large-scale meta-analysis. Acta Psychiatr Scand. 2015;131(2):75–88.
Bernstein EE, Rabideau DJ, Gigler ME, Nierenberg AA, Deckersbach T, Sylvia LG. Patient perceptions of physical health and bipolar symptoms: the intersection of mental and physical health. J Affect Disord. 2016;189:203–6.
Thieme K, Turk DC, Flor H. Comorbid depression and anxiety in fibromyalgia syndrome: relationship to somatic and psychosocial variables. Psychosom Med. 2004;66(6):837–44.
Cohen H, Neumann L, Haiman Y, Matar MA, Press J, Buskila D. Prevalence of post-traumatic stress disorder in fibromyalgia patients: overlapping syndromes or post-traumatic fibromyalgia syndrome? Semin Arthritis Rheum. 2002;32(1):38–50.
Carta MG, Hardoy MC, Pilu A, Sorba M, Floris AL, Mannu FA, et al. Improving physical quality of life with group physical activity in the adjunctive treatment of major depressive disorder. Clin Pract Epidemiol Mental Health. 2008;4(1):1–6.
Annesi JJ, Unruh JL. Relations of exercise, self-appraisal, mood changes and weight loss in obese women: testing propositions based on Baker and Brownell's (2000) model. Am J Med Sci. 2008;335(3):198–204.
Duman RS. Neurotrophic factors and regulation of mood: role of exercise, diet and metabolism. Neurobiol Aging. 2005;26(Suppl 1):S88–93.
Ernst C, Olson AK, Pinel JP, Lam RW, Christie BR. Antidepressant effects of exercise: evidence for an adult-neurogenesis hypothesis? J Psychiatry Neurosci. 2006;31(2):84–91.
Cataldo AM, McPhie DL, Lange NT, Punzell S, Elmiligy S, Ye NZ, et al. Abnormalities in mitochondrial structure in cells from patients with bipolar disorder. Am J Pathol. 2010;177(2):575–85.
Dinas PC, Koutedakis Y, Flouris AD. Effects of exercise and physical activity on depression. Ir J Med Sci. 2011;180(2):319–25.
Benes FM, Matzilevich D, Burke RE, Walsh J. The expression of proapoptosis genes is increased in bipolar disorder, but not in schizophrenia. Mol Psychiatry. 2006;11(3):241–51.
Clay HB, Sillivan S, Konradi C. Mitochondrial dysfunction and pathology in bipolar disorder and schizophrenia. Int J Dev Neurosci. 2011;29(3):311–24.
Gomez-Pinilla F, Zhuang Y, Feng J, Ying Z, Fan G. Exercise impacts brain-derived neurotrophic factor plasticity by engaging mechanisms of epigenetic regulation. Eur J Neurosci. 2011;33(3):383–90.
Cotman CW, Berchtold NC, Christie L. Exercise builds brain health: key roles of growth factor cascades and inflammation. Trends Neurosci. 2007;30(9):464–72.
Schuch FB, Vasconcelos-Moreno MP, Borowsky C, Zimmermann AB, Wollenhaupt-Aguiar B, et al. The effects of exercise on oxidative stress (TBARS) and BDNF in severely depressed inpatients. Eur Arch Psychiatry Clin Neurosci. 2014;264(7):605–13.
Marais L, Stein DJ, Daniels WMU. Exercise increases BDNF levels in the striatum and decreases depressive-like behavior in chronically stressed rats. Metab Brain Dis. 2009;24(4):587–97.
Schinder AF, Poo M. The neurotrophin hypothesis for synaptic plasticity. Trends Neurosci. 2000;23(12):639–45.
Binder DK, Scharfman HE. Brain-derived neurotrophic factor. Growth Factors. 2004;22(3):123–31.
Bearden CE, Thompson PM, Dalwani M, Hayashi KM, Lee AD, Nicoletti M, et al. Greater corticol grey matter density in lithium-treated patients with bipolar disorder. Biol Psychiatry. 2007;62(1):7–16.
Bearden CE, Thompson PM, Dutton RA, Frey BN, Peluso MA, Nicoletti M, et al. Three-dimensional mapping of hippocampal anatomy in unmedicated and lithium-treated patients with bipolar disorder. Neuropsychopharmacology. 2008;33(6):1229–38.
Duman CH, Schlesinger L, Russell DS, Duman RS. Voluntary exercise produces antidepressant and anxiolytic behavioral effects in mice. Brain Res. 2008;1199:148–58.
Russo-Neustadt A, Ha T, Ramirez R, Kesslak JP. Physical activity-antidepressant treatment combination: impact on brain-derived neurotrophic factor and behavior in an animal model. Behav Brain Res. 2001;120(1):87–95.
Guillin O, Demily C, Thibaut F. Brain-derived neurotrophic factor in schizophrenia and its relation with dopamine. Int Rev Neurobiol. 2007;78:377–95.
Brunoni AR, Lopes M, Fregni F. A systematic review and meta-analysis of clinical studies on major depression and BDNF levels: implications for the role of neuroplasticity in depression. Int J Neuropsychopharmacol. 2008;11(8):1169–80.
Lee B, Kim H, Park S, Kim Y. Decreased plasma BDNF level in depressive patients. J Affect Disord. 2007;101(1):239–44.
Cirulli F, Berry A, Chiarotti F, Alleva E. Intrahippocampal administration of BDNF in adult rats affects short-term behavioral plasticity in the Morris water maze and performance in the elevated plus-maze. Hippocampus. 2004;14(7):802–7.
Gustafsson G, Lira CM, Johansson J, Wisén A, Wohlfart B, Ekman R, et al. The acute response of plasma brain-derived neurotrophic factor as a result of exercise in major depressive disorder. Psychiatry Res. 2009;169(3):244–8.
Erickson KI, Voss MW, Prakash RS, Basak C, Szabo A, Chaddock L, et al. Exercise training increases size of hippocampus and improves memory. Proc Natl Acad Sci. 2011;108(7):3017–22.
Toups MSP, Greer TL, Kurian BT, Grannemann BD, Carmody TJ, Huebinger R, et al. Effects of serum brain derived neurotrophic factor on exercise augmentation treatment of depression. J Psychiatr Res. 2011;45(10):1301–6.
Szuhany KL, Bugatti M, Otto MW. A meta-analytic review of the effects of exercise on brain-derived neurotrophic factor. J Psychiatr Res. 2015;60:56–64.
Russo-Neustadt AA, Beard RC, Huang YM, Cotman CW. Physical activity and antidepressant treatment potentiate the expression of specific brain-derived neurotrophic factor transcripts in the rat hippocampus. Neuroscience. 2000;101(2):305–12.
Ma Q. Beneficial effects of moderate voluntary physical exercise and its biological mechanisms on brain health. Neurosci Bull. 2008;24(4):265–7.
Andreazza AC, Wang JF, Salmasi F, Shao L, Young LT. Specific subcellular changes in oxidative stress in prefrontal cortex from patients with bipolar disorder. J Neurochem. 2013;127(4):552–61.
Berk M, Kapczinski F, Andreazza AC, Dean OM, Giorlando F, Maes M, et al. Pathways underlying neuroprogression in bipolar disorder: focus on inflammation, oxidative stress and neurotrophic factors. Neurosci Biobehav Rev. 2011;35(3):804–17.
Steckert AV, Valvassori SS, Moretti M, Dal-Pizzol F, Quevedo J. Role of oxidative stress in pathophysiology of bipolar disorder. Neurochem Res. 2010;35(3):1295–301.
Konradi C, Eaton M, MacDonald ML, Walsh J, Benes FM, Heckers S. Molecular evidence for mitochondrial dysfunction in bipolar disorder. Arch Gen Psychiatry. 2004;61(3):301–8.
Munakata K, Tanaka M, Mori K, Washizuka S, Yoneda M, Tajima O, et al. Mitochondrial DNA 3644T→C mutation associated with bipolar disorder. Genomics. 2004;84(6):1041–50.
Naydenov AV, MacDonald ML, Ongur D, Konradi C. Differences in lymphocyte electron transport gene expression levels between subjects with bipolar disorder and normal controls in response to glucose deprivation stress. Arch Gen Psychiatry. 2007;64(5):555–64.
Stork C, Renshaw PF. Mitochondrial dysfunction in bipolar disorder: evidence from magnetic resonance spectroscopy research. Mol Psychiatry. 2005;10(10):900–19.
Wang J-F. Defects of mitochondrial electron transport chain in bipolar disorder: implications for mood-stabilizing treatment. Can J Psychiatry-Rev Can Psychiatr. 2007;52(12):753–62.
Erkan OM, Gulec M, Ozerol E, Polat R, Akyol O. Antioxidant enzyme activities and oxidative stress in affective disorders. Int J Clin Psychopharmacol. 2004;19(2):89–95.
Michel TM, Pülschen D, Thome J. The role of oxidative stress in depressive disorders. Curr Pharm Des. 2012;22(46):5890–9.
Tobe EH. Mitochondrial dysfunction, oxidative stress, and major depressive disorder. Neuropsychiatr Dis Treat. 2013;9:567–73.
Ng F, Berk M, Dean O, Bush AI. Oxidative stress in psychiatric disorders: evidence base and therapeutic interventions. Int J Neuropsychopharmacol. 2008;11(6):851–76.
Ng F, Berk M, Dean O, Busch AI. Oxidative stress in psychiatric disorders: evidence base and therapeutic implications. Int J Neuropsychopharmacol. 2008;22(6):851–76.
Handschin C, Spiegelman BM. The role of exercise and PGC1α in inflammation and chronic disease. Nature. 2008;454(7203):463–9.
Agarwal D, Haque M, Sriramula S, Mariappan N, Pariaut R, Francis J. Role of proinflammatory cytokines and redox homeostasis in exercise-induced delayed progression of hypertension in spontaneously hypertensive rats. Hypertension. 2009;54(6):1393–400.
Urso ML, Clarkson PM. Oxidative stress, exercise, and antioxidant supplementation. Toxicology. 2003;189(1):41–54.
Gleeson M. Immune function in sport and exercise. J Appl Physiol. 2007;103(2):693–9.
Alsuwaidan MT, Kucyi A, Law CWY, McIntyre RS. Exercise and bipolar disorder: a review of neurobiological mediators. Neruomol Med. 2009;11(4):328–36.
Moore DS. The developing Genome: an introduction to behavioral epigenetics. New York, NY: Oxford University Press; 2015. pp. 1–309.
Bird A. Perceptions of epigenetics. Nature. 2007;447(7143):396–8.
Massart R, Mongeau R, Lanfumey L. Beyond the monoaminergic hypothesis: Philos Trans R Soc B: Biol Sci neuroplasticity and epigenetic changes in a transgenic mouse model of depression. 2012;367(1601):2485–94.
Sanchis-Gomar F, Garcia-Gimenez JL, Perez-Quilis C, Gomez-Cabrera MC, Pallardo FV, Lippi G. Physical exercise as an epigenetic modulator: eustress, the “positive stress” as an effector of gene expression. J Strength Cond Res. 2012;26(12):3469–72.
Mersy DJ. Health benefits of aerobic exercise. Postgrad Med. 1991;90(1):103–12.
Garber CE, Blissmer B, Deschenes MR, Franklin B, Lamonte MJ, Lee I, et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–59.
Sylvia LG, Friedman ES, Kocsis JH, Bernstein EE, Brody BD, Kinrys G, et al. Association of exercise with quality of life and mood symptoms in a comparative effectiveness study of bipolar disorder. J Affect Disord. 2013;151(2):722–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Ms. Hearing has no competing interests to report.
Ms. Chang has no competing interests to report.
Dr. Deckersbach’s research has been funded by NIH, NIMH, NARSAD, TSA, IOCDF, Tufts University, DBDAT and Otsuka Pharmaceuticals. He has received honoraria, consultation fees and/or royalties from the MGH Psychiatry Academy, BrainCells Inc., Clintara, LLC., Systems Research and Applications Corporation, Boston University, the Catalan Agency for Health Technology Assessment and Research, the National Association of Social Workers Massachusetts, the Massachusetts Medical Society, Tufts University, NIDA, NIMH, Oxford University Press, Guilford Press, and Rutledge. He has also participated in research funded by DARPA, NIH, NIMH, NIA, AHRQ, PCORI, Janssen Pharmaceuticals, The Forest Research Institute, Shire Development Inc., Medtronic, Cyberonics, Northstar, and Takeda.
Dr. Nierenberg serves as a consultant for Abbott Laboratories, Alkermes, American Psychiatric Association, Appliance Computing Inc. (Mindsite), Basliea, Brain Cells, Inc., Brandeis University, Bristol Myers Squibb, Clintara, Corcept, Dey Pharmaceuticals, Dainippon Sumitomo (now Sunovion), Eli Lilly and Company, EpiQ, L.P./Mylan Inc., Forest, Genaissance, Genentech, GlaxoSmithKline, Healthcare Global Village, Hoffman LaRoche, Infomedic, Intra-cellular Therapies, Lundbeck, Janssen Pharmaceutica, Jazz Pharmaceuticals, Medavante, Merck, Methylation Sciences, NeuroRx, Naurex, Novartis, PamLabs, Parexel, Pfizer, PGx, Health, Otsuka, Ridge Diagnostics Shire, Schering-Plough, Somerset, Sunovion, Takeda Pharmaceuticals, Targacept, and Teva; He has also consulted through the MGH Clinical Trials Network and Institute (CTNI) for Astra Zeneca, Brain Cells, Inc., Dianippon Sumitomo/Sepracor, Johnson and Johnson, Labopharm, Merck, Methylation Science, Novartis, PGx Health, Shire, Schering-Plough, Targacept and Takeda/Lundbeck Pharmaceuticals. He has received grants/research support from American Foundation for Suicide Prevention, AHRQ, Brain and Behavior Research Foundation, Bristol-Myers Squibb, Cederroth, Cephalon, Cyberonics, Elan, Eli Lilly, Forest, GlaxoSmithKline, Intra-Cellular Therapies, Janssen Pharmaceutica, Lichtwer Pharma, Marriott Foundation, Mylan, NIMH, PamLabs, PCORI, Pfizer Pharmaceuticals, Shire, Stanley Foundation, Takeda, and Wyeth-Ayerst and honoraria from Belvoir Publishing, University of Texas Southwestern Dallas, Brandeis University, Bristol-Myers Squibb, Hillside Hospital, American Drug Utilization Review, American Society for Clinical Psychopharmacology, Baystate Medical Center, Columbia University, CRICO, Dartmouth Medical School, Health New England, Harold Grinspoon Charitable Foundation, IMEDEX, International Society for Bipolar Disorder, Israel Society for Biological Psychiatry, Johns Hopkins University, MJ Consulting, New York State, Medscape, MBL Publishing, MGH Psychiatry Academy, National Association of Continuing Education, Physicians Postgraduate Press, SUNY Buffalo, University of Wisconsin, University of Pisa, University of Michigan, University of Miami, University of Wisconsin at Madison, APSARD, ISBD, SciMed, Slack Publishing and Wolters Klower Publishing, ASCP, NCDEU, Rush Medical College, Yale University School of Medicine, NNDC, Nova Southeastern University, NAMI, Institute of Medicine, CME Institute, ISCTM, World Congress on Brain Behavior and Emotion, Congress of the Hellenic Society for Basic and Clinical Pharmacology, and ADAA. Dr. Nierenberg has stock in Appliance Computing, Inc. (MindSite), Brain Cells, Inc., and Medavante. He holds copyrights for Clinical Positive Affect Scale and the MGH Structured Clinical Interview for the Montgomery Asberg Depression Scale exclusively licensed to the MGH Clinical Trials Network and Institute (CTNI).
Dr. Sylvia was a shareholder in Concordant Rater Systems and has served in the past year as a consultant for United Biosource Corporation, Clintara, Bracket, and Clinical Trials Network and Institute. Dr. Sylvia receives royalties from New Harbinger. She has received grant/research support from NIMH, PCORI, AFSP, and Takeda.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Additional information
This article is part of the Topical Collection on Mood and Anxiety Disorders
Rights and permissions
About this article
Cite this article
Hearing, C.M., Chang, W.C., Szuhany, K.L. et al. Physical Exercise for Treatment of Mood Disorders: A Critical Review. Curr Behav Neurosci Rep 3, 350–359 (2016). https://doi.org/10.1007/s40473-016-0089-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40473-016-0089-y