Abstract
Purpose of Review
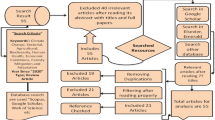
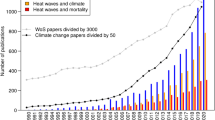
Our goal was to assess current literature and knowledge on associations between characteristics (mean, variability, extremes) of ambient temperatures and human health. We were motivated by concerns that climate change, which operates on a time frame of decades or longer, may influence not only shorter-term associations between weather and health (daily/weekly) but also have enduring implications for population health. We reviewed papers published between 2010 and 2017 on the health effects of longer-term (3 weeks to years) exposures to ambient temperature. We sought to answer: “What health outcomes have been associated with longer-term exposures?” We included studies on a diverse range of health outcomes, with the exception of vector-borne diseases such as malaria. Longer-term exposures were considered to be exposures to annual and seasonal temperatures and temperature variability.
Recent Findings
We found 26 papers meeting inclusion criteria, which addressed mortality, morbidity, respiratory disease, obesity, suicide, infectious diseases, and allergies among various age groups. In general, most studies found associations between longer-term temperature metrics and health outcomes. Effects varied by population subgroup. For example, associations with suicide differed by sex and underlying chronic illness modified effects of heat on mortality among the elderly.
Summary
We found that regional and local temperatures, and changing conditions in weather due to climate change, were associated with a diversity of health outcomes through multiple mechanisms. Future research should focus on evidence for particular mechanistic pathways in order to inform adaptation responses to climate change.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
IPCC 2014 Climate change: impacts, adaptation, and vulnerability. IPCC Working Group II Contribution to AR5 [Internet]. 2014. Available from: http://ipcc-wg2.gov/AR5/.
Meehl GA, Tebaldi C. More intense, more frequent, and longer lasting heat waves in the 21st century. Science (80-. ). [Internet]. 2004;305:994–7. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15310900.
Tebaldi C, Hayhoe K, Arblaster JM, Meehl GA. Going to the extremes. Clim Chang. 2006;79:185–211.
Ganguly AR, Steinhaeuser K, Erickson DJ, Branstetter M, Parish ES, Singh N, et al. Higher trends but larger uncertainty and geographic variability in 21st century temperature and heat waves. Proc Natl Acad Sci U S A [Internet]. 2009 [cited 2012 Mar 21];106:15555–9. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2739867&tool=pmcentrez&rendertype=abstract.
Clark RT, Murphy JM, Brown SJ. Do global warming targets limit heatwave risk? Geophys Res Lett. 2010;37
Barriopedro D, Fischer EM, Luterbacher J, Trigo RM, García-Herrera R. The hot summer of 2010: redrawing the temperature record map of Europe. Science [Internet]. 2011 [cited 2012 Mar 13];332:220–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21415316.
Anderson BT. Intensification of seasonal extremes given a 2°C global warming target. Clim Chang. 2011;112:325–37.
Basu R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Health. [Internet]. 2009 [cited 2017 Dec 20];8:40. Available from: http://ehjournal.biomedcentral.com/articles/10.1186/1476-069X-8-40.
Analitis A, Katsouyanni K, Biggeri A, Baccini M, Forsberg B, Bisanti L, Kirchmayer U., Ballester F., Cadum E., Goodman P.G., Hojs A., Sunyer J., Tiittanen P., Michelozzi P. Effects of cold weather on mortality: results from 15 European cities within the PHEWE project. Am J Epidemiol [Internet] 2008;168:1397–408. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18952849.
Breitner S, Wolf K, Devlin RB, Diaz-Sanchez D, Peters A, Schneider A. Short-term effects of air temperature on mortality and effect modification by air pollution in three cities of Bavaria, Germany: a time-series analysis. Sci Total Environ. [Internet]. 2014 [cited 2014 Jul 9];485–486:49–61. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24704956.
Kaiser R, Le Tertre A, Schwartz J, Gotway CA, Daley WR, Rubin CH. The effect of the 1995 heat wave in Chicago on all-cause and cause-specific mortality. Am J Public Heal. [Internet]. 2007;97 Suppl 1:S158–62. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17413056.
Le Tertre A, Lefranc A, Eilstein D, Declercq C, Medina S, Blanchard M, et al. Impact of the 2003 heatwave on all-cause mortality in 9 French cities. Epidemiology [Internet]. 2006;17:75–9. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16357598.
Ostro BD, Roth LA, Green RS, Basu R. Estimating the mortality effect of the July 2006 California heat wave. Env Res [Internet] 2009;109:614–9. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19394595.
McGeehin MA, Mirabelli M. The potential impacts of climate variability and change on temperature-related morbidity and mortality in the United States. Environ Health Perspect. 2001;109:185–9.
Halonen JII, Zanobetti A, Sparrow D, Vokonas PSS, Schwartz J. Relationship between outdoor temperature and blood pressure. Occup Env Med [Internet] 2011;68:296–301. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=20864465.
Barnett AG. Temperature and cardiovascular deaths in the US elderly: changes over time. Epidemiology [Internet]. 2007 [cited 2012 Apr 26];18:369–72. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17435447.
Alpérovitch A, Lacombe J-M, Hanon O, Dartigues J-F, Ritchie K, Ducimetière P, et al. Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals: the Three-City study. Arch. Intern. Med. [Internet]. 2009 [cited 2012 Apr 26];169:75–80. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19139327.
Halonen JII, Zanobetti A, Sparrow D, Vokonas PSS, Schwartz J. Associations between outdoor temperature and markers of inflammation: a cohort study. Environ. Health [Internet]. 2010/07/27. 2010;9:42. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20653951.
Hampel R, Breitner S, Rückerl R, Frampton MW, Koenig W, Phipps RP, et al. Air temperature and inflammatory and coagulation responses in men with coronary or pulmonary disease during the winter season. Occup Environ Med. [Internet]. 2010 [cited 2012 Apr 26];67:408–16. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19884649.
Donaldson GC, Keatinge WR. Mortality related to cold weather in elderly people in southeast England, 1979-94. BMJ. 1997;315:1055–6.
Neild PJ, Syndercombe-Court D, Keatinge WR, Donaldson GC, Mattock M, Caunce M. Cold-induced increases in erythrocyte count, plasma cholesterol and plasma fibrinogen of elderly people without a comparable rise in protein C or factor X. Clin Sci. 1994;86:43–8.
Yamamoto H, Zheng KC, Ariizumi M. Influence of heat exposure on serum lipid and lipoprotein cholesterol in young male subjects. Ind Health. [Internet] 2003;41:1–7. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12674547.
Halonen JII, Zanobetti A, Sparrow D, Vokonas PSS, Schwartz J. Outdoor temperature is associated with serum HDL and LDL. Environ Res [Internet]. 2011;111:281–7. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=21172696.
Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. Temperature and mortality in 11cities of the eastern United States. Am J Epidemiol. 2002;155:80–7.
O’Neill MS, Zanobetti A, Schwartz J. Modifiers of the temperature and mortality association in seven US cities. Am J Epidemiol [Internet]. 2003;157:1074–82. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12796043.
Braga AL, Zanobetti A, Schwartz J. The time course of weather-related deaths. Epidemiology [Internet]. 2001;12:662–7. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11679794.
Medina-Ramon M, Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatization and effect modification in 50 United States Cities. Occup Env. Med [Internet]. 2007;64:827–833. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17600037.
Medina-Ramon M, Zock JP, Kogevinas M, Sunyer J, Torralba Y, Borrell A, et al. Asthma, chronic bronchitis, and exposure to irritant agents in occupational domestic cleaning: a nested case-control study. Occup Environ Med. [Internet]. 2005;62:598–606. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16109815.
Michelozzi P, De Sario M, Accetta G, de’Donato F, Kirchmayer U, D’Ovidio M, et al. Temperature and summer mortality: geographical and temporal variations in four Italian cities. J. Epidemiol Community Health [Internet]. 2006 [cited 2012 Apr 23];60:417–23. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2563963&tool=pmcentrez&rendertype=abstract.
Hansen AL, Bi P, Ryan P, Nitschke M, Pisaniello D, Tucker G. The effect of heat waves on hospital admissions for renal disease in a temperate city of Australia. Int J Epidemiol [Internet]. 2008;37:1359–65. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18710886
Knowlton K, Rotkin-Ellman M, King G, Margolis HG, Smith D, Solomon G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect [Internet]. 2009;117:61–7. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19165388
Michelozzi P, Accetta G, De Sario M, D’Ippoliti D, Marino C, Baccini M, et al. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Accetta G, De Sario M, D’Ippoliti D, Marino C, Baccini M, Biggeri A, et al., editors. Am J Respir Crit Care Med [Internet]. 2009;179:383–9. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19060232.
Schwartz J, Samet JM, Patz JA. Hospital admissions for heart disease: the effects of temperature and humidity. Epidemiology [Internet]. 2004;15:755–61. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15475726
Hajat S, Kovats RS, Atkinson RW, Haines A. Impact of hot temperatures on death in London: a time series approach. J Epidemiol Community Health. 2002;56:367–72.
Medina-Ramon M, Zanobetti A, Cavanagh DP, Schwartz J. Extreme temperatures and mortality: assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ Health Perspect [Internet]. 2006;114:1331–6. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16966084
Armstrong B. Models for the relationship between ambient temperature and daily mortality. Epidemiology [Internet]. 2006;17:624–31. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17028505
Schwartz J. Who is sensitive to extremes of temperature?: a case-only analysis. Epidemiology [Internet]. 2005;16:67–72. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15613947
Diaz J, Jordan A, Garcia R, Lopez C, Alberdi JC, Hernandez E, et al. Heat waves in Madrid 1986-1997: effects on the health of the elderly. Int Arch Occup Environ Health. 2002;75:163–70.
O’Neill MS. Air conditioning and heat-related health effects. Appl Environ Sci Public Health. 2003;1:9–12.
Balbus JM, Malina C. Identifying vulnerable subpopulations for climate change health effects in the United States. J Occup Environ Med [Internet]. 2009;51:33–7. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19136871
Harlan SL, Brazel AJ, Prashad L, Stefanov WL, Larsen L. Neighborhood microclimates and vulnerability to heat stress. Soc Sci Med [Internet]. 2006;63:2847–63. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16996668
O’Neill MS, Zanobetti A, Schwartz J. Disparities by race in heat-related mortality in four US Cities: the role of air conditioning prevalence. J Urban Health [Internet]. 2005;82:191–7. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15888640
Conlon KC, Rajkovich NB, White-Newsome JL, Larsen L, O’Neill MS. Preventing cold-related morbidity and mortality in a changing climate. Maturitas [Internet]. 2011;69:197–202. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21592693
Ye X, Wolff R, Yu W, Vaneckova P, Pan X, Tong S. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect. [Internet]. 2012 [cited 2014 May 5];120:19–28. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3261930&tool=pmcentrez&rendertype=abstract
Claeys MJ, Rajagopalan S, Nawrot TS, Brook RD. Climate and environmental triggers of acute myocardial infarction. Eur Heart J. [Internet]. Oxford University Press; 2016 [cited 2017 Dec 20];38:ehw151. Available from: http://eurheartj.oxfordjournals.org/lookup/doi/10.1093/eurheartj/ehw151.
•• Zhang Y, Yu C, Wang L. Temperature exposure during pregnancy and birth outcomes: An updated systematic review of epidemiological evidence. Environ Pollut. [Internet]. 2017 [cited 2017 Dec 20];225:700–12. Available from: http://linkinghub.elsevier.com/retrieve/pii/S026974911730074X. This review indicates that high temperatures are a risk factor for preterm birth, low birth weight, and stillbirth, while less evidence was reported for cold-related effects. Given the projected changes in the global climate, these findings may have great implications in public decision-making regarding maternal and child health to reduce temperature-related adverse birth outcomes. Due to inconsistencies among temperature indicators used in different studies, the authors recommend that more well-designed studies are needed in more diversified climate zones, to ascertain the association between temperature and birth outcomes.
Wang X, Cao Y, Hong D, Zheng D, Richtering S, Sandset EC, et al. Ambient temperature and stroke occurrence: a systematic review and meta-analysis. Int J Environ Res Public Health [Internet]. 2016 [cited 2017 Dec 20];13:698. Available from: http://www.mdpi.com/1660-4601/13/7/698.
Bunker A, Wildenhain J, Vandenbergh A, Henschke N, Rocklöv J, Hajat S, et al. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly: a systematic review and meta-analysis of epidemiological evidence. EBioMedicine [Internet]. 2016 [cited 2017 Dec 20];6:258–68. Available from: http://linkinghub.elsevier.com/retrieve/pii/S2352396416300731.
Carlton EJ, Woster AP, DeWitt P, Goldstein RS, Levy K. A systematic review and meta-analysis of ambient temperature and diarrhoeal diseases. Int J Epidemiol. [Internet]. 2016 [cited 2017 Dec 20];45:117–30. Available from: https://academic.oup.com/ije/article-lookup/doi/10.1093/ije/dyv296.
Benmarhnia T, Deguen S, Kaufman JS, Smargiassi A. Review article: vulnerability to heat-related mortality: a systematic review, meta-analysis, and meta-regression analysis. Epidemiology [Internet]. 2015 [cited 2017 Dec 20];26:781–93. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00001648-201511000-00002.
Hess JJ, Saha S, Luber G. Summertime acute heat illness in U.S. emergency departments from 2006 through 2010: analysis of a nationally representative sample. Environ Health Perspect. [Internet]. 2014 [cited 2018 Jan 17];122:1209–15. Available from: http://ehp.niehs.nih.gov/1306796.
Michal Freedman D, Kitahara CM, Linet MS, Alexander BH, Neta G, Little MP, et al. Ambient temperature and risk of first primary basal cell carcinoma: a nationwide United States cohort study. J Photochem Photobiol B. [Internet]. 2015 [cited 2018 Jan 30];148:284–9. Available from: http://linkinghub.elsevier.com/retrieve/pii/S101113441500148759.
• Sharma A, Sharma T, Panwar MS, Sharma D, Bundel R, Hamilton RT, et al. Colder environments are associated with a greater cancer incidence in the female population of the United States. Tumour Biol. [Internet]. 2017 [cited 2018 Jan 17];39:1010428317724784. Available from: http://journals.sagepub.com/doi/10.1177/1010428317724784 This is an important study as it is one of the few to examine the effect of temperature on site-specific cancer, and suggests that cold environment could be an independent risk factor for cancer especially in the female population.
•• Molina O, Saldarriaga V. The perils of climate change: In utero exposure to temperature variability and birth outcomes in the Andean region. Econ Hum Biol. [Internet]. 2017 [cited 2018 Jan 17];24:111–24. Available from: http://linkinghub.elsevier.com/retrieve/pii/S1570677X1630212X This study is one of the first to examine the adverse effects of temperature variability on health conditions of newborns by investigating how in utero exposure to temperature variability, measured as the fluctuations relative to the historical local temperature mean, affects birth outcomes in the Andean region. The finding that temperature variability is associated with decreased birth weight is important, and sheds light on the adverse effects of temperature variability on health conditions of newborns. Moreover, the authors find some evidence that these results can be explained by food insecurity and health care during pregnancy that arise due to increased temperature variability.
Ogata S, Yorioka N. Environmental factors influencing the survival of chronic dialysis patients. Clin Exp Nephrol. [Internet]. 2011 [cited 2018 Jan 30];15:405–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21249416.
•• Azage M, Kumie A, Worku A, C. Bagtzoglou A, Anagnostou E. Effect of climatic variability on childhood diarrhea and its high risk periods in northwestern parts of Ethiopia. Shaman J, editor. PLoS One [Internet]. 2017 [cited 2018 Jan 30];12:e0186933. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29073259. In Ethiopia, the burden of childhood diarrhea is high and diarrhea is the second leading cause of childhood deaths in the country. This study found an association between climatic factors and the occurrence of childhood diarrhea, and recommend that local health departments should develop appropriate climate-change adaptation and preparedness for diarrhea prevention and control strategies.
Liao J, Qin Z, Zuo Z, Yu S, Zhang J. Spatial-temporal mapping of hand foot and mouth disease and the long-term effects associated with climate and socio-economic variables in Sichuan Province, China from 2009 to 2013. Sci. Total Environ. [Internet]. 2016 [cited 2018 Jan 17];563–564:152–9. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0048969716305836.
Bind AM, Zanobetti A, Gasparrini A, Peters A, Coull B, Baccarelli A, et al. Effects of temperature and relative humidity on DNA methylation. Epidemiology [Internet]. 2014 [cited 2014 May 12];25:561–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24809956.
• Wallwork RS, Colicino E, Zhong J, Kloog I, Coull BA, Vokonas P, et al. Ambient fine particulate matter, outdoor temperature, and risk of metabolic syndrome. Am J Epidemiol. [Internet]. 2017 [cited 2017 Dec 16];185:30–9. Available from: https://academic.oup.com/aje/article-lookup/doi/10.1093/aje/kww157. Metabolic syndrome is an urgent public health concern that affects 10–25% of the global population and is associated with increased risk of cardiovascular disease, asthma, sleep apnea, and selected malignancies and with higher total and cause-specific mortality. This is the first study to examine and find an association between long-term exposures to outdoor temperatures with increased risk of developing elevated fasting blood glucose. The authors suggest that this could be due to the role of adipose tissue in adaptation to temperature differences. Specifically, people exposed to comparatively higher temperatures burn fewer calories to maintain body temperature, have less brown adipose tissue, and therefore may be more prone to developing insulin resistance.
Valdés S, Maldonado-Araque C, García-Torres F, Goday A, Bosch-Comas A, Bordiú E, et al. Ambient temperature and prevalence of obesity in the Spanish population: the Diabet.es study. Obesity (Silver Spring). [Internet]. 2014 [cited 2018 Jan 17];22:2328–32. Available from: http://doi.wiley.com/10.1002/oby.20866
Voss JD, Masuoka P, Webber BJ, Scher AI, Atkinson RL. Association of elevation, urbanization and ambient temperature with obesity prevalence in the United States. Int J Obes (Lond). [Internet]. 2013 [cited 2018 Jan 17];37:1407–12. Available from: http://www.nature.com/articles/ijo20135
• Yang HK, Han K, Cho J-H, Yoon K-H, Cha B-Y, Lee S-H. Ambient temperature and prevalence of obesity: a nationwide population-based study in Korea. Meyre D, editor. PLoS One [Internet]. 2015 [cited 2018 Jan 17];10:e0141724. Available from: http://dx.plos.org/10.1371/journal.pone.0141724 Excess body weight is an important risk factor for mortality and morbidity. It is known that unhealthy diets and sedentary lifestyle are major contributors to the increasing prevalence of obesity. But few studies examined other conditions such as genetic, biological, and environmental factors. This study demonstrates a significant association between ambient temperature and prevalence of obesity among the Korean population and suggests that a possible explanation could be cold-induced thermogenesis.
Metintas S, Kurt E, PARFAIT Study Group. Geo-climate effects on asthma and allergic diseases in adults in Turkey: results of PARFAIT study. Int J Environ Health Res. [Internet]. 2010 [cited 2018 Jan 17];20:189–99. Available from: http://www.tandfonline.com/doi/full/10.1080/09603120903456828
Miller ME, Shapiro NL, Bhattacharyya N. Annual temperature and the prevalence of frequent ear infections in childhood. Am J Otolaryngol. [Internet]. 2012 [cited 2018 Jan 17];33:51–5. Available from: http://linkinghub.elsevier.com/retrieve/pii/S019607091100024X.
• Silverberg JI, Braunstein M, Lee-Wong M. Association between climate factors, pollen counts, and childhood hay fever prevalence in the United States. Mosby. 2015 [cited 2017 Dec 18];135. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0091674914011154. This study used the National Survey of Children’s Health to examine the impact of specific climate factors and pollen counts on the US prevalence of hay fever and statewide variation in prevalence. This study provides evidence of the influences of climate on the prevalence of HF, suggesting that climate factors and pollen counts likely aggravate HF, resulting in chronic disease.
•• Armstrong B, Bell ML, de Sousa Zanotti Stagliorio Coelho M, Leon Guo Y-L, Guo Y, Goodman P, et al. Longer-term impact of high and low temperature on mortality: an international study to clarify length of mortality displacement. Environ Health Perspect. [Internet]. 2017 [cited 2018 Jan 17];125:107009. Available from: http://ehp.niehs.nih.gov/EHP1756 This is the largest study estimating the association between annual mortality and annual summaries of heat and cold, with 278 locations from 12 countries around the world. This study not only found strong evidence that annual mortality was associated with the extent to which years experienced long or severe hot or cold weather, but also that most lives were shortened by at least a year, and these associations are confirmed as important public health concerns.
• Goggins WB, Yang C, Hokama T, Law LSK, Chan EYY. Using annual data to estimate the public health impact of extreme temperatures. Am J Epidemiol. [Internet]. 2015 [cited 2018 Jan 17];182:80–7. Available from: https://academic.oup.com/aje/article-lookup/doi/10.1093/aje/kwv013. This study used the annual cold-degrees days and heat-degrees days in an annual time series analysis. The results indicate that annual time periods with a greater frequency and severity of both hot and cold weather tend to have higher mortality rates than years with more moderate daily temperature; moreover the results imply that the excess mortality observed during periods of hot or cold weather is not simply due to short- or medium-term forward mortality displacement, and that a substantial proportion of these deaths occurred in people who would have been expected to live at least several more months in the absence of these exposures.
•• Rehill N, Armstrong B, Wilkinson P. Clarifying life lost due to cold and heat: a new approach using annual time series. BMJ Open [Internet]. 2015 [cited 2018 Jan 17];5:e005640. Available from: http://bmjopen.bmj.com/cgi/doi/10.1136/bmjopen-2014-005640. This was the first study to apply an annual time series analysis to examine the association between long-term mortality and long-term temperature, and to use the “heat-degrees” and “cold-degrees” derived as the number of degrees above a threshold to summarize heat and cold day across the year.
• Lim Y-H, Bell ML, Kan H, Honda Y, Guo Y-LL, Kim H. Economic status and temperature-related mortality in Asia. Int. J. Biometeorol. [Internet]. 2015 [cited 2018 Jan 17];59:1405–12. Available from: http://link.springer.com/10.1007/s00484-014-0950-1. This study found that in cities with low GDP per capita, heat risk increases with higher summer temperature but not in cities with high GDP per capita. These findings may indicate a greater heat-related risk in hotter cities if economic resources are insufficient, possibly due to poor individual- or city-level adaptation or mitigation efforts.
Schumann B, Edvinsson S, Evengård B, Rocklöv J. The influence of seasonal climate variability on mortality in pre-industrial Sweden. Glob Health Action [Internet]. 2013 [cited 2018 Jan 17];6:20153. Available from: https://www.tandfonline.com/doi/full/10.3402/gha.v6i0.20153.
Zanobetti A, O’Neill MSMSS, Gronlund CJJCJ, Schwartz JDJDD. Summer temperature variability and long-term survival among elderly people with chronic disease. Proc. Natl. Acad. Sci. [Internet]. 2012 [cited 2012 Apr 11];109:6608–13. Available from: http://www.pnas.org/cgi/doi/10.1073/pnas.1113070109.
•• Shi L, Kloog I, Zanobetti A, Liu P, Schwartz JD. Impacts of temperature and its variability on mortality in New England. Nat Clim Chang. [Internet]. 2015 [cited 2016 Mar 18];5:988–91. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26640524 This study, by estimating impacts of both mean temperature and temperature variability in summer and winter simultaneously, adds considerable strength to the evidence of a significant association between mortality and prolonged exposures to temperatures, especially temperature variability. Moreover, this study shows that increases in temperature variability can have similar estimated effects on mortality as increases in mean temperature. Therefore, the variability of atmospheric temperature emerges as a key factor for potential health impacts of climate change.
•• Shi L, Liu P, Wang Y, Zanobetti A, Kosheleva A, Koutrakis P, et al. Chronic effects of temperature on mortality in the Southeastern USA using satellite-based exposure metrics. Sci Rep. [Internet]. 2016 [cited 2018 Jan 17];6:30161. Available from: http://www.nature.com/articles/srep30161. This study adds more evidence on the chronic effect of temperature on mortality. Moreover, it suggests that even in regions with hot summers and high prevalence of air conditioning like the Southeastern USA, areas with higher summer temperature or temperature variability had higher death rates. This suggests that temperature related mortality is already present at non-trivial levels, and adaptation ability is limited and therefore these locations may be particularly sensitive to rising summer temperatures in the future.
Fountoulakis KN, Savopoulos C, Zannis P, Apostolopoulou M, Fountoukidis I, Kakaletsis N, et al. Climate change but not unemployment explains the changing suicidality in Thessaloniki Greece (2000–2012). J. Affect. Disord. [Internet]. 2016 [cited 2018 Jan 17];193:331–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26796233.
Helama S, Holopainen J, Partonen T. Temperature-associated suicide mortality: contrasting roles of climatic warming and the suicide prevention program in Finland. Environ Health Prev Med. [Internet]. 2013 [cited 2018 Jan 17];18:349–55. Available from: http://link.springer.com/10.1007/s12199-013-0329-7.
Fukuda M, Fukuda K, Shimizu T, Nobunaga M, Mamsen LS, Yding Andersen C. Climate change is associated with male:female ratios of fetal deaths and newborn infants in Japan. Fertil Steril. [Internet]. 2014;102:1364–1370.e2. Available from: doi:https://doi.org/10.1016/j.fertnstert.2014.07.1213.
Fukuda M, Fukuda K, Shimizu T, Nobunaga M, Mamsen LS, Yding Andersen C. Climate change is associated with male:female ratios of fetal deaths and newborn infants in Japan. Fertil Steril [Internet]. Elsevier; 2014 [cited 2017 Dec 13];102:1364–1370.e2. Available from: http://www.sciencedirect.com.ezp-prod1.hul.harvard.edu/science/article/pii/S0015028214018408?via%3Dihub.
Nordio F, Zanobetti A, Colicino E, Kloog I, Schwartz J. Changing patterns of the temperature-mortality association by time and location in the US, and implications for climate change. Environ Int. [Internet]. 2015 [cited 2015 Jun 18];81:80–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25965185.
Gronlund CJ. Racial and socioeconomic disparities in heat-related health effects and their mechanisms: a review. Curr Epidemiol. reports [Internet]. 2014 [cited 2018 Jan 27];1:165–73. Available from: http://link.springer.com/10.1007/s40471-014-0014-4.
Funding
National Institutes of Health NIH/NIEHS grants P30 ES000002, P30 ES017885, R21 ES020156, and RO1 ES024332; EPA grants RD83615601 and RD 83587201; National Science Foundation grant 1520803; and National Institute for Occupational Safety and Health grant T42 OH008455. Its contents are solely the responsibility of the grantee and do not necessarily represent the official views of the US EPA. Further, US EPA does not endorse the purchase of any commercial products or services mentioned in the publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Antonella Zanobetti reports grants from National Institutes of Health NIH/NIEHS and grants from US EPA, during the conduct of the study. Marie S. O’Neill report grants from National Science Foundation, and grants from National Institute of Occupational Safety and Health, during the conduct of the study.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Environmental Epidemiology
Rights and permissions
About this article
Cite this article
Zanobetti, A., O’Neill, M.S. Longer-Term Outdoor Temperatures and Health Effects: a Review. Curr Epidemiol Rep 5, 125–139 (2018). https://doi.org/10.1007/s40471-018-0150-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40471-018-0150-3