Abstract
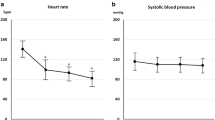
Intravenous landiolol [Rapibloc® (EU)], an ultra short-acting highly cardioselective β1-blocker, is approved in the EU for the rapid short-term control of tachyarrhythmias in the perioperative and intensive care settings. It has long been used in Japan to treat perioperative tachyarrhythmias. The efficacy of landiolol has been demonstrated in a large number of randomized controlled clinical trials. Landiolol significantly reduced heart rate in patients with postoperative or intraoperative supraventricular tachycardia relative to placebo and in those with atrial fibrillation/flutter and left ventricular dysfunction relative to digoxin. It was more effective than diltiazem in converting postoperative atrial fibrillation (POAF) to normal sinus rhythm. Perioperative prophylactic administration of landiolol significantly reduced the incidence of POAF during the first week after cardiac and other surgeries, compared with diltiazem, placebo or no landiolol treatment. Landiolol also attenuated adverse haemodynamic and other responses to invasive procedures such as percutaneous coronary intervention, tracheal intubation, extubation and electroconvulsive therapy. Landiolol was generally well tolerated, with a relatively low risk of hypotension and bradycardia. Landiolol has more favourable pharmacological properties than esmolol, a short-acting β-blocker commonly used for the rapid control of heart rate. Although additional comparative studies are warranted to define the place of landiolol relative to esmolol, current evidence suggest that landiolol is a useful option for the rapid short-term control of tachyarrhythmias. Landiolol offers a simple dosage scheme and is available in two easy-to-use formulations (concentrate and powder).
Similar content being viewed by others
References
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur J Heart Fail. 2016;18(8):891–975.
Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–962.
Blomstrom-Lundqvist C, Scheinman MM, Aliot EM, et al. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the European Society of Cardiology committee for practice guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003;42(18):1493–531.
Rapibloc 20 mg/2 ml concentrate for solution for injection: summary of product characteristics. 2017. http://www.medicinesauthority.gov.mt. Accessed 21 Dec 2017.
Rapibloc 300 mg and 600 mg powder for solution for infusion: summary of product characteristics. 2017. https://mri.cts-mrp.eu. Accessed 24 Jan 2018.
Plosker GL. Landiolol: a review of its use in intraoperative and postoperative tachyarrhythmias. Drugs. 2013;73(9):959–77.
Taenaka N, Kikawa S. The effectiveness and safety of landiolol hydrochloride, an ultra-short-acting β1-blocker, in postoperative patients with supraventricular tachyarrhythmias: a multicenter, randomized, double-blind, placebo-controlled study. Am J Cardiovasc Drugs. 2013;13(5):353–64.
Mori K, Yamada K, Fukuda T, et al. Landiolol hydrochloride for early postoperative tachycardia after transthoracic esophagectomy. Surg Today. 2014;44(5):848–54.
Niwa Y, Koike M, Iwata N, et al. Effect of landiolol hydrochloride on tachyarrhythmia after esophagectomy. Hepatogastroenterology. 2014;61(134):1546–51.
Hamaguchi S, Nagao M, Takahashi Y, et al. Low dose landiolol combined with catecholamine can decrease heart rate without suppression of cardiac contraction after cardiopulmonary bypass. Dokkyo J Med Sci. 2014;41(1):27–33.
Sakamoto A, Kitakaze M, Takamoto S, et al. Landiolol, an ultra-short-acting β1-blocker, more effectively terminates atrial fibrillation than diltiazem after open heart surgery: prospective, multicenter, randomized, open-label study (JL-KNIGHT study). Circ J. 2012;76(5):1097–101.
Nishi H, Sakaguchi T, Miyagawa S, et al. Efficacy of landiolol hydrochloride for atrial fibrillation after open heart surgery. Heart Vessels. 2013;28(4):490–6.
Ojima T, Iwahashi M, Nakamori M, et al. Atrial fibrillation after esophageal cancer surgery: an analysis of 207 consecutive patients. Surg Today. 2014;44(5):839–47.
Nojiri T, Yamamoto K, Maeda H, et al. Efficacy of low-dose landiolol, an ultrashort-acting β-blocker, on postoperative atrial fibrillation in patients undergoing pulmonary resection for lung cancer. Gen Thorac Cardiovasc Surg. 2011;59(12):799–805.
Shibata SC, Uchiyama A, Ohta N, et al. Efficacy and safety of landiolol compared to amiodarone for the management of postoperative atrial fibrillation in intensive care patients. J Cardiothorac Vasc Anesth. 2016;30(2):418–22.
Xiao J, He P, Zou Q, et al. Landiolol in the treatment of the intraoperative supraventricular tachycardia: a multicenter, randomized, double-blind, placebo-controlled study. J Clin Anesth. 2015;27(2):120–8.
Nagai R, Kinugawa K, Inoue H, et al. Urgent management of rapid heart rate in patients with atrial fibrillation/flutter and left ventricular dysfunction: comparison of the ultra-short-acting β1-selective blocker landiolol with digoxin (J-Land Study). Circ J. 2013;77(4):908–16.
Kinugawa K, Nagai R, Inoue H, et al. Impacts of patient characteristics on the effectiveness of landiolol in AF/AFL patients complicated with LV dysfunction: subgroup analysis of the J-Land study. Adv Ther. 2014;31(4):426–39.
Kobayashi S, Murakami W, Myoren T, et al. A low-dose β1-blocker effectively and safely slows the heart rate in patients with acute decompensated heart failure and rapid atrial fibrillation. Cardiology. 2014;127(2):105–13.
Ozaki T, Yamada T, Morita T, et al. Urgent control of rapid atrial fibrillation using landiolol in patients with acute decompensated heart failure with reduced or preserved left ventricular ejection fraction [abstract no. P6352]. Eur Heart J. 2016;37(Suppl.):1319.
Kobayashi S, Susa T, Tanaka T, et al. Low-dose beta-blocker in combination with milrinone safely improves cardiac function and eliminates pulsus alternans in patients with acute decompensated heart failure. Circ J Off J Jpn Circ Soc. 2012;76(7):1646–53.
Adachi T, Sato A, Baba M, et al. Novel use of the ultra-short-acting intravenous beta1-selective blocker landiolol for supraventricular tachyarrhythmias in patients with congestive heart failure. Heart Vessels. 2014;29(4):464–9.
Kobayashi S, Susa T, Ishiguchi H, et al. A low-dose β1-blocker in combination with milrinone improves intracellular Ca2+ handling in failing cardiomyocytes by inhibition of milrinone-induced diastolic Ca2+ leakage from the sarcoplasmic reticulum. PLoS One. 2015. https://doi.org/10.1371/journal.pone.0114314.
Kimura Y, Aga C, Hayashi H, et al. Efficacy and safety of landiolol in heart failure patients with supraventricular tachycardia compared to diltiazem [abstract no. O01-3]. J Card Fail. 2016;22(9 Suppl. 1):167.
Kiuchi S, Aikawa H, Hisatake S, et al. Efficacy of intravenous administration of landiolol in patients with acute heart failure and supraventricular tachyarrhythmia. J Clin Med Res. 2017;9(5):426–32.
Wada Y, Aiba T, Tsujita Y, et al. Practical applicability of landiolol, an ultra-short-acting beta1-selective blocker, for rapid atrial and ventricular tachyarrhythmias with left ventricular dysfunction. J Arrhythm. 2016;32(2):82–8.
Oka E, Iwasaki Y, Fujimoto Y. Differential effectiveness of landiolol among atrial fibrillation and atrial flutter/tachycardia in the patients with left ventricular dysfunction [abstract no. PE-776]. In: In: 81st Annual Scientific Meeting of the Japanese Circulation Society. 2017.
Yoshima S. Concomitant administration of landiolol and dobutamine in acute heart failure syndrome with atrial tachyarrhythmia [abstract no. P2699]. Eur Heart J. 2017; 38(Suppl).
Okajima M, Takamura M, Taniguchi T. Landiolol, an ultra-short-acting beta1-blocker, is useful for managing supraventricular tachyarrhythmias in sepsis. World J Crit Care Med. 2015;4(3):251–7.
Sezai A, Osaka S, Yaoita H, et al. Safety and efficacy of landiolol hydrochloride for prevention of atrial fibrillation after cardiac surgery in patients with left ventricular dysfunction: Prevention of Atrial Fibrillation After Cardiac Surgery With Landiolol Hydrochloride for Left Ventricular Dysfunction (PLATON) trial. J Thorac Cardiovasc Surg. 2015;150(4):957–64.
Nagaoka E, Arai H, Tamura K, et al. Prevention of atrial fibrillation with ultra-low dose landiolol after off-pump coronary artery bypass grafting. Ann Thorac Cardiovasc Surg. 2014;20(2):129–34.
Ogawa S, Okawa Y, Goto Y, et al. Perioperative use of a beta blocker in coronary artery bypass grafting. Asian Cardiovasc Thorac Ann. 2013;21(3):265–9.
Fujii M, Bessho R, Ochi M, et al. Effect of postoperative landiolol administration for atrial fibrillation after off pump coronary artery bypass surgery. J Cardiovasc Surg. 2012;53(3):369–74.
Sezai A, Minami K, Nakai T, et al. Landiolol hydrochloride for prevention of atrial fibrillation after coronary artery bypass grafting: new evidence from the PASCAL trial. J Thorac Cardiovasc Surg. 2011;141(6):1478–87.
Sezai A, Nakai T, Hata M, et al. Feasibility of landiolol and bisoprolol for prevention of atrial fibrillation after coronary artery bypass grafting: a pilot study. J Thorac Cardiovasc Surg. 2012;144(5):1241–8.
Sakaguchi M, Sasaki Y, Hirai H, et al. Efficacy of landiolol hydrochloride for prevention of atrial fibrillation after heart valve surgery. Int Heart J. 2012;53(6):359–63.
Tamura T, Yatabe T, Yokoyama M. Prevention of atrial fibrillation after cardiac surgery using low-dose landiolol: a systematic review and meta-analysis. J Clin Anesth. 2017;42:1–6.
Ji T, Feng C, Sun L, et al. Are beta-blockers effective for preventing post-coronary artery bypass grafting atrial fibrillation? Direct and network meta-analyses. Ir J Med Sci. 2016;185(2):503–11.
Yoshida T, Furukita Y, Yamamoto Y, et al. A randomized, open label study of the efficacy of prophylactic 24-h low-dose landiolol for atrial fibrillation in transthoracic esophagectomy. Esophagus. 2017;14(1):97–103.
Ojima T, Nakamori M, Nakamura M, et al. Randomized clinical trial of landiolol hydrochloride for the prevention of atrial fibrillation and postoperative complications after oesophagectomy for cancer. Br J Surg. 2017;104(8):1003–9.
Horikoshi Y, Goyagi T, Kudo R, et al. The suppressive effects of landiolol administration on the occurrence of postoperative atrial fibrillation and tachycardia, and plasma IL-6 elevation in patients undergoing esophageal surgery: a randomized controlled clinical trial. J Clin Anesth. 2017;38:111–6.
Yagi K, Usuda J, Sakamoto A. Perioperative landiolol infusion reduces the incidence of atrial fibrillation after pulmonary lobectomy: postoperative randomized controlled study. Open J Anesthesiol. 2016;6:119–23.
Suzuki K, Numaguchi A, Adachi YU, et al. Continuous administration of landiolol reduced QT dispersion in postoperative patients. J Clin Anesth. 2014;26(6):438–42.
Kiyokuni M, Konishi M, Sakamaki K, et al. Beneficial effect of early infusion of landiolol, a very short-acting beta-1 adrenergic receptor blocker, on reperfusion status in acute myocardial infarction. Int J Cardiol. 2016;221:321–6.
Park H, Otani H, Noda T, et al. Intracoronary followed by intravenous administration of the short-acting β-blocker landiolol prevents myocardial injury in the face of elective percutaneous coronary intervention. Int J Cardiol. 2013;167(4):1547–51.
Hanada K, Higuma T, Nishizaki F, et al. Randomized study on the efficacy and safety of landiolol, an ultra-short-acting β1-adrenergic blocker, in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention. Circ J. 2012;76(2):439–45.
Hoshi T, Sato A, Nishina H, et al. Acute hemodynamic effects of landiolol, an ultra-short-acting beta-blocker, in patients with acute coronary syndrome: preliminary study. J Cardiol. 2012;60(4):252–6.
Kawaguchi M, Kawaraguchi Y, Yamamoto Y, et al. Effects of landiolol on systemic and cerebral hemodynamics and recovery from anesthesia in patients undergoing craniotomy. J Anesth. 2010;24(4):503–10.
Miyazaki M, Kadoi Y, Takashi S, et al. Comparative effects of propofol, landiolol, and nicardipine on hemodynamic and bispectral index responses to endotracheal intubation: a prospective, randomized, double-blinded study. J Clin Anesth. 2008;24(4):257–62.
Kawaguchi M, Takamatsu I, Masui K, et al. Effect of landiolol on bispectral index and spectral entropy responses to tracheal intubation during propofol anaesthesia. Br J Anaesth. 2008;101(2):273–8.
Goyagi T, Tanaka M, Nishikawa T. Landiolol attenuates the cardiovascular response to tracheal intubation. J Anesth. 2005;19(4):282–6.
Oda Y, Nishikawa K, Hase I, et al. The short-acting β1-adrenoceptor antagonists esmolol and landiolol suppress the bispectral index response to tracheal intubation during sevoflurane anesthesia. Anesth Analg. 2005;100(3):733–7.
Wajima Z, Shiga T, Imanaga K, et al. Prophylactic continuous administration of landiolol, a novel β1 blocker, blunts hyperdynamic responses during electroconvulsive therapy without altering seizure activity. Int J Psychiatry Clin Pract. 2010;14(2):132–6.
Kitamura A, Sakamoto A, Inoue T, et al. Efficacy of an ultrashort-acting β-adrenoceptor blocker (ONO-1101) in attenuating cardiovascular responses to endotracheal intubation. Eur J Clin Pharmacol. 1997;51(6):467–71.
Inoue S, Tanaka Y, Kawaguchi M, et al. The efficacy of landiolol for suppressing the hyperdynamic response following laryngoscopy and tracheal intubation: a systematic review. Anaesth Intensive Care. 2009;37(6):893–902.
Kaneko M, Yamaguchi S, Hamaguchi S, et al. Effects of landiolol on QT interval and QT dispersion during induction of anesthesia using computerized measurement. J Clin Anesth. 2009;21(8):555–61.
Yang X, Li S. Analysis of esmolol and landiolol on elderly patients in the perioperative period with gastric surgery. Int J Clin Exp Pathol. 2016;9(12):12755–60.
Tochikubo J, Adachi YU, Ejima T, et al. Landiolol reduces hemodynamic responses to bronchoscopy-assisted suctioning in intubated ICU patients. J Intensive Care. 2014;2(6):1–4.
Hirota K, Baba S, Fukushi S, et al. Efficacy of landiolol in attenuating hemodynamic responses to local epinephrine infiltration in patients undergoing vaginal total hysterectomy. J Anesth. 2005;19(1):17–20.
Saito S, Nishihara F, Akihiro T, et al. Landiolol and esmolol prevent tachycardia without altering cerebral blood flow. Can J Anaesth. 2005;52(10):1027–34.
Krumpl G, Ulc I, Trebs M, et al. Bolus application of landiolol and esmolol: comparison of the pharmacokinetic and pharmacodynamic profiles in a healthy Caucasian group. Eur J Clin Pharmacol. 2017;73(4):417–28.
Krumpl G, Ulc I, Trebs M, et al. Pharmacokinetics and -dynamics of low, intermediate and high dose landiolol and esmolol during long term infusion in healthy Caucasians. J Cardiovasc Pharmacol. 2017. https://doi.org/10.1097/FJC.0000000000000554.
Walter E, Schalle K. Cost-effectiveness of landiolol, an ultra-short-acting beta-blocker, for prevention of postoperative atrial fibrillation in Germany [abstract no. PCV84]. Value Heath. 2017;20(9).
Nasrollahi-Shirazi S, Sucic S, Yang Q, et al. A comparison of the β-adrenergic receptor antagonists landiolol and esmolol: receptor selectivity, partial agonism and pharmacochaperoning actions. J Pharmacol Exp Ther. 2016;359(1):73–81.
Ikeshita K, Nishikawa K, Toriyama S, et al. Landiolol has a less potent negative inotropic effect than esmolol in isolated rabbit hearts. J Anesth. 2008;22(4):361–6.
Shibata S, Okamoto Y, Endo S, et al. Direct effects of esmolol and landiolol on cardiac function, coronary vasoactivity, and ventricular electrophysiology in guinea-pig hearts. J Pharmacol Sci. 2012;118(2):255–65.
Sasao J, Tarver SD, Kindscher JD, et al. In rabbits, landiolol, a new ultra-short-acting beta-blocker, exerts a more potent negative chronotropic effect and less effect on blood pressure than esmolol. Can J Anesth. 2001;48(10):985–9.
Krumpl G, Ulc I, Trebs M, et al. Pharmacodynamic and -kinetic behavior of low-, intermediate-, and high-dose landiolol during long-term infusion in Whites. J Cardiovasc Pharmacol. 2017;70(1):42–51.
Krumpl G, Ulc I, Trebs M, et al. Pharmacokinetics and pharmacodynamics of two different landiolol formulations in a healthy Caucasian group. Eur J Pharm Sci. 2016;92:64–73.
Acknowledgments
During the peer review process, the manufacturer of landiolol was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Funding
The preparation of this review was not supported by any external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yahiya Y. Syed is a salaried employee of Adis/Springer, is responsible for the article content and declares no relevant conflicts of interest.
Additional information about this Adis Drug Review can be found at http://www.medengine.com/Redeem/8F1DF0605D713619.
Additional information
The manuscript was reviewed by: T. Hoshi, Department of Cardiology, Faculty of Medicine, University of Tsukuba, Tsukuba, Japan; G. Krumpl, MRN Medical Research Network GmbH, Vienna, Austria; Z. Wajima, Department of Anesthesiology, Tokyo Medical University Hachioji Medical Center, Tokyo, Japan
Rights and permissions
About this article
Cite this article
Syed, Y.Y. Landiolol: A Review in Tachyarrhythmias. Drugs 78, 377–388 (2018). https://doi.org/10.1007/s40265-018-0883-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-018-0883-9