Abstract
Background and Purpose
Selective serotonin reuptake inhibitors (SSRIs) are frequently prescribed in the elderly due to a more favorable risk profile than other antidepressants (ADs). However, SSRIs are associated with an increased risk of gastrointestinal bleeding, while evidence on the risk of hemorrhagic stroke (HS) is limited. Therefore, we compared the risk of HS associated with the use of ADs in the elderly.
Methods
Based on data from the German Pharmacoepidemiological Research Database (GePaRD), a case–control study matched on age, sex, and health insurance provider, nested in a cohort of incident users of ADs ≥ 65 years of age was performed. Cases were identified from hospital discharge diagnoses, and exposure was identified from outpatient prescriptions. Multivariable conditional logistic regression was used to estimate adjusted odds ratios (ORs) with 95% confidence intervals (CIs).
Results
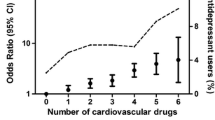
Based on 4059 cases and 40,590 controls, an increased risk of HS was found in current use of SSRIs (OR 1.39, 95% CI 1.22–1.58), selective serotonin and noradrenaline reuptake inhibitors (1.69, 1.35–2.11), noradrenergic and specific serotonergic ADs (1.44, 1.22–1.69), and noradrenaline reuptake inhibitors (3.81, 1.54–9.43) compared with tri- and tetracyclic antidepressants. An increased risk of HS was seen in patients with a high baseline risk of bleeding and in patients with depression. The risk of HS varied between individual ADs.
Conclusion
Our study shows that the use of medications inhibiting serotonin and/or noradrenaline reuptake increases the risk of HS in patients aged 65 years and older and that the risk varies across individual ADs.

Similar content being viewed by others
References
Cecilio Á, Francisco LM, Pilar GG, Silvia GR. Risk–benefit analysis of antidepressant drug treatment in the elderly. Psychogeriatrics. 2014;14(4):261–8.
American Geriatrics Society Beers Criteria Update Expert Panel. American geriatrics society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227–46.
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. Stopp/start criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–8.
de Abajo FJ, Alberto L, Rodríguez G, Montero D. Association between selective serotonin reuptake inhibitors and upper gastrointestinal bleeding: population based case-control study. BMJ. 1999;319(7217):1106–9.
de Abajo FJ, Montero D, Rodriguez LA, Madurga M. Antidepressants and risk of upper gastrointestinal bleeding. Basic Clin Pharmacol Toxicol. 2006;98(3):304–10.
Meijer WE, Heerdink ER, Nolen WA, Herings RM, Leufkens HG, Egberts AC. Association of risk of abnormal bleeding with degree of serotonin reuptake inhibition by antidepressants. Arch Intern Med. 2004;164(21):2367–70.
Eschenfelder CC, Zeller JA, Stingele R. Schlaganfall—ursachen und klassifikation. Hämostaseologie. 2006;26(4):298–308.
Zahuranec DB, Lisabeth LD, Sanchez BN, Smith MA, Brown DL, Garcia NM, et al. Intracerebral hemorrhage mortality is not changing despite declining incidence. Neurology. 2014;82(24):2180–6.
Lekander I, Willers C, von Euler M, Lilja M, Sunnerhagen KS, Pessah-Rasmussen H, et al. Relationship between functional disability and costs one and two years post stroke. PLoS One. 2017;12(4):e0174861.
Douglas I, Smeeth L, Irvine D. The use of antidepressants and the risk of haemorrhagic stroke: a nested case control study. Br J Clin Pharmacol. 2010;71:115–20.
Kharofa J, Sekar P, Haverbusch M, Moomaw C, Flaherty M, Kissela B, et al. Selective serotonin reuptake inhibitors and risk of hemorrhagic stroke. Stroke. 2007;38:3049–51.
Smoller JW, Allison M, Cochrane BB, Curb JD, Perlis RH, Robinson JG, et al. Antidepressant use and risk of incident cardiovascular morbidity and mortality among postmenopausal women in the women’s health initiative study. Arch Intern Med. 2009;169(22):2128–39.
Bak S, Tsiropoulos I, Kjærsgaard JO, Andersen M, Mellerup E, Hallas J, et al. Selective serotonin reuptake inhibitors and the risk of stroke a population-based case-control study. Stroke. 2002;33:1465–73.
Chen Y, Guo JJ, Li H, Wulsin L, Patel NC. Risk of cerebrovascular events associated with antidepressant use in patients with depression: a population-based, nested case-control study. Ann Pharmacother. 2008;42(2):177–84.
de Abajo FJ, Jick H, Derby L, Jick S, Schmitz S. Intracranial haemorrhage and use of selective serotonin reuptake inhibitors. Br J Clin Pharmacol. 2000;50:43–7.
Renoux C, Vahey S, Dell’Aniello S, Boivin J. Association of selective serotonin reuptake inhibitors with the risk for spontaneous intracranial hemorrhage. JAMA Neurol. 2017;74(2):173–80.
Douros A, Ades M, Renoux C. Risk of intracranial hemorrhage associated with the use of antidepressants inhibiting serotonin reuptake: a systematic review. CNS Drugs. 2018;32(4):321–34.
Verdel BM, Souverein PC, Meenks SD, Heerdink ER, Leufkens HG, Egberts TC. Use of serotonergic drugs and the risk of bleeding. Clin Pharmacol Ther. 2011;89(1):89–96.
Wu CS, Wang SC, Cheng YC, Gau SS. Association of cerebrovascular events with antidepressant use: a case-crossover study. The American journal of psychiatry. 2011;168(5):511–21.
Ohlmeier C, Langner I, Garbe E, Riedel O. Validating mortality in the german pharmacoepidemiological research database (gepard) against a mortality registry. Pharmacoepidemiol Drug Saf. 2016;25(7):778–84.
Jobski K, Kollhorst B, Garbe E, Schink T. The risk of ischemic cardio- and cerebrovascular events associated with oxycodone–naloxone and other extended-release high-potency opioids: a nested case–control study. Drug Saf. 2017;40(6):505–15.
Jobski K, Schmedt N, Kollhorst B, Krappweis J, Schink T, Garbe E. Characteristics and drug use patterns of older antidepressant initiators in germany. Eur J Clin Pharmacol. 2017;73(1):105–13.
Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158(9):915–20.
Rothman KJ, Greenland S, Lash TL. Case-control studies. In: Rothman KJ, Greenland S, Lash TL, editors. Modern epidemiology. Philadelphia: Lippincott Williams & Wilkens; 2008. p. 111–27.
Schmedt N, Jobski K, Kollhorst B, Krappweis J, Ruther E, Schink T, et al. Treatment patterns and characteristics of older antipsychotic users in germany. Int Clin Psychopharmacol. 2016;31(3):159–69.
Gardarsdottir H, Souverein PC, Egberts TC, Heerdink ER. Construction of drug treatment episodes from drug-dispensing histories is influenced by the gap length. J Clin Epidemiol. 2010;63(4):422–7.
Schneeweiss S, Avorn J. A review of uses of health care utilization databases for epidemiologic research on therapeutics. J Clin Epidemiol. 2005;58(4):323–37.
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (has-bled) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093–100.
Mutschler E, Geisslinger G, Kroemer HK, Menzel S, Ruth P. Mutschler arzneimittelwirkungen. Lehrbuch der pharmakologie, der klinischen pharmakologie und toxikologie. [Mutschler Drug Reactions. Textbook of Pharmacology, Clinical Pharmacology and Toxicology]. Stuttgart: Wissenschaftliche verlagsgesellschaft mbH; 2013.
Lee YC, Lin CH, Lin MS, Lu Y, Chang CH, Lin JW. Comparison of the effects of serotonin-norepinephrine reuptake inhibitors versus selective serotonin reuptake inhibitors on cerebrovascular events. J Clin Psychiatry. 2016;77(1):e1–7.
Chen Y, Guo JJ, Li H, Wulsin L, Patel NC. Risk of cerebrovascular events associated with antidepressant use in patients with depression: a population-based, nested case–control study. Neurology. 2008;42:177–84.
Coupland C, Dhiman P, Morriss R, Arthur A, Barton G, Hippisley-Cox J. Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ. 2011;343:d4551.
Eguale T, Buckeridge DL, Winslade NE, Benedetti A, Hanley JA, Tamblyn R. Drug, patient, and physician characteristics associated with off-label prescribing in primary care. Arch Intern Med. 2012;172(10):781–8.
Knoll J, Bernheim MLC. Analysis of the pharmacological effects of selective monoamine oxidase inhibitors. Ciba foundation symposium 39—monoamine oxidase and its inhibition. John Wiley & Sons, Ltd; 2008. Pp 135–61.
Sandler M. Monoamine oxidase inhibitor efficacy in depression and the “cheese effect”. Psychol Med. 1981;11(3):455–8.
Halperin D, Reber G. Influence of antidepressants on hemostasis. Dialogues Clin Neurosci. 2007;9(1):47–59.
Garbe E, Kreisel SH, Behr S. Risk of subarachnoid hemorrhage and early case fatality associated with outpatient antithrombotic drug use. Stroke. 2013;44(9):2422–6.
Feigin V, Lawes C, Bennett D, Anderson C. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2:43–53.
Feigin VL, Krishnamurthi RV, Parmar P, Norrving B, Mensah GA, Bennett DA, et al. Update on the global burden of ischemic and hemorrhagic stroke in 1990–2013: the gbd 2013 study. Neuroepidemiology. 2015;45(3):161–76.
Martini SR, Flaherty ML, Brown WM, Haverbusch M, Comeau ME, Sauerbeck LR, et al. Risk factors for intracerebral hemorrhage differ according to hemorrhage location. Neurology. 2012;79(23):2275–82.
Acknowledgements
The authors would like to thank all SHIs who provided data for this study, namely AOK Bremen/Bremerhaven, DAK-Gesundheit, hkk Krankenkasse, and Die Techniker (TK). The authors would further would like to thank Franziska von Mandelsloh and Nadine Schlie for their help in developing the outcome definitions and defining potential confounding factors, as well as Marieke Niemeyer and Inga Schaffer for statistical programming of the matched cohort.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
Wiebke Schäfer, Bianca Kollhorst, and Tania Schink are employees of the Leibniz Institute for Prevention Research and Epidemiology – BIPS. Unrelated to this study, BIPS occasionally conducts studies financed by the pharmaceutical industry. Almost exclusively, these are post-authorization safety studies (PASS) requested by health authorities. The studies and the resulting publications are not influenced by the pharmaceutical industry. Christina Princk is currently an employee at the Governmental Institute of Public Health of Lower Saxony, Hanover, Germany, and has no conflicts of interest that are directly relevant to the content of this study.
Ethical Approval
In Germany, the utilization of health insurance data for scientific research is regulated by the Code of Social Law. All involved SHIs, the German Federal (Social) Insurance, and the Senator for Science, Health and Consumer Protection in Bremen as their responsible authorities approved the use of the data for this study. Informed consent for studies based on the GePaRD is not required by law, and, according to the Ethics Committee of the University of Bremen, these studies are exempt from Institutional Review Board review.
Funding
No sources of funding were used to assist in the preparation of this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schäfer, W., Princk, C., Kollhorst, B. et al. Antidepressants and the Risk of Hemorrhagic Stroke in the Elderly: a Nested Case–Control Study. Drug Saf 42, 1081–1089 (2019). https://doi.org/10.1007/s40264-019-00837-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-019-00837-y