Abstract
Background
Activities of hepatic cytochrome P450 enzymes (CYPs) are relevant for hepatic clearance of drugs and known to be decreased in patients with liver cirrhosis. Several studies have reported the effect of liver cirrhosis on CYP activity, but the results are partially conflicting and for some CYPs lacking.
Objective
In this study, we aimed to investigate the CYP activity in patients with liver cirrhosis with different Child stages (A-C) using the Basel phenotyping cocktail approach.
Methods
We assessed the pharmacokinetics of the six compounds and their CYP-specific metabolites of the Basel phenotyping cocktail (CYP1A2: caffeine, CYP2B6: efavirenz, CYP2C9: flurbiprofen, CYP2C19: omeprazole, CYP2D6: metoprolol, CYP3A: midazolam) in patients with liver cirrhosis (n = 16 Child A cirrhosis, n = 15 Child B cirrhosis, n = 5 Child C cirrhosis) and matched control subjects (n = 12).
Results
While liver cirrhosis only marginally affected the pharmacokinetics of the low to moderate extraction drugs efavirenz and flurbiprofen, the elimination rate of caffeine was reduced by 51% in patients with Child C cirrhosis. For the moderate to high extraction drugs omeprazole, metoprolol, and midazolam, liver cirrhosis decreased the elimination rate by 75%, 37%, and 60%, respectively, increased exposure, and decreased the apparent systemic clearance (clearance/bioavailability). In patients with Child C cirrhosis, the metabolic ratio (ratio of the area under the plasma concentration–time curve from 0 to 24 h of the metabolite to the parent compound), a marker for CYP activity, decreased by 66%, 47%, 92%, 73%, and 43% for paraxanthine/caffeine (CYP1A2), 8-hydroxyefavirenz/efavirenz (CYP2B6), 5-hydroxyomeprazole/omeprazole (CYP2C19), α-hydroxymetoprolol/metoprolol (CYP2D6), and 1′-hydroxymidazolam/midazolam (CYP3A), respectively. In comparison, the metabolic ratio 4-hydroxyflurbiprofen/flurbiprofen (CYP2C9) remained unchanged.
Conclusions
Liver cirrhosis affects the activity of CYP isoforms differently. This variability must be considered for dose adjustment of drugs in patients with liver cirrhosis.
Clinical Trial Registration
NCT03337945.
Similar content being viewed by others
Liver cirrhosis had large effects on the pharmacokinetics of the moderate to high extraction drugs omeprazole, metoprolol, and midazolam, but lacked or had less pronounced effects on the low to moderate extraction drugs caffeine, efavirenz, and flurbiprofen. |
Liver cirrhosis did not affect cytochrome P450 enzyme (CYP) 2C9 activity, but decreased the activities of CYP1A2, 2B6, 2C19, 2D6, and 3A. |
The data can be used for dose adjustment of specific drugs in patients with liver cirrhosis and to construct a mathematical model for further improvement and facilitation of dose adjustment in this group of patients. |
1 Introduction
Most patients with liver cirrhosis are treated with multiple drugs not only for liver disease but also for comorbidities [1,2,3]. Because of impaired liver function and portosystemic shunts, the kinetics of drugs used in patients with liver cirrhosis can be altered substantially [4,5,6]. In most cases, drug exposure is increased when the same dose is used as in patients without liver cirrhosis, possibly leading to toxicity. We have previously shown that 336 of 1653 prescriptions (20.3%) in 400 patients with liver cirrhosis were incorrect (drug contraindicated or dosage too high), leading to 210 adverse drug reactions and 24 hospitalizations [7]. Avoiding critical drugs or adjusting their dose is therefore important in this group of patients.
Hepatic drug clearance depends on the liver blood flow, the activity of drug-metabolizing enzymes, and the free drug concentration [4]. For drugs with a high hepatic extraction (e.g., ≥ 70% and a bioavailability ≤ 30%), hepatic clearance is mainly determined by the functional blood flow across the liver, which is dependent on the extent of portosystemic shunting. For drugs with a low hepatic extraction (e.g., ≤ 30% and a bioavailability ≥ 70%), hepatic clearance is mainly determined by the product of the free drug concentration and the activity of metabolizing enzymes. For drugs with a moderate hepatic extraction (30–70%) both hepatic blood flow and activity of metabolizing enzymes determine the hepatic clearance. For drugs with a high protein binding (e.g., > 95%), the fraction of free drug can vary considerably in patients with liver cirrhosis owing to a reduced serum concentration of drug-binding proteins such as albumin and acid α-glycoprotein and displacement from the protein binding [8]. For low and moderate extraction drugs, an increase in the free drug concentration should result in an increase in hepatic drug clearance, which, however, is often overruled by a decrease in the activity of drug-metabolizing enzymes in the cirrhotic liver. Drugs without a functional group that cannot be conjugated directly must first undergo phase I metabolism, which is mainly performed by cytochrome P450 enzymes (CYPs) [9]. Cytochrome P450 activity is therefore an important parameter for estimating the hepatic clearance of low and moderate extraction drugs undergoing phase I metabolism.
We have developed and validated a functional test to assess the activity of the six major CYPs simultaneously using a drug phenotyping cocktail approach [10,11,12]. For this test, we administer a single capsule containing compounds specific for six different CYP isoforms in a subtherapeutic dosage (Table 1 of the Electronic Supplementary Material [ESM]) and measure the plasma concentration of the parent compound and of a specific metabolite at different timepoints [13]. The ratio between the area under the plasma concentration–time curve (AUC) or between the plasma concentration at a specific timepoint of the metabolite and the parent compound (called the metabolic ratio, MR) reflects the activity of a specific CYP.
The effect of liver cirrhosis on CYP activity has been investigated in previous studies. In most of them, only one or two CYPs were tested and in only one study the cocktail approach was used to investigate four CYPs simultaneously [14]. However, in their cocktail study, Frye et al. determined the MR only at one timepoint and did not assess a pharmacokinetic profile, which may not be precise enough for the assessment of CYP activity in liver cirrhosis. The currently available studies showed a decrease in the activity of CYP1A2 [14,15,16] and CYP2C19 [14, 17, 18], no change [17] or a decrease in the activity of CYP2D6 [14, 19], a decrease in the MR of CYP2E1 [14], and a decrease in the activity of CYP3A [20,21,22,23]. Regarding CYP2B6, increased efavirenz plasma concentrations have been reported in human immunodeficiency virus-infected patients with liver fibrosis/cirrhosis, but no pharmacokinetic profiles have been obtained [24, 25]. For CYP2C9, to the best of our knowledge, no information is currently available.
Considering the sometimes conflicting or lacking available data, we decided to study the CYP activity in patients with liver cirrhosis with different Child stages using the Basel phenotyping cocktail. The specific aims of the study were to obtain pharmacokinetic profiles for the six substrates and their specific metabolites and to assess the activities of the six major drug metabolizing CYPs involved.
2 Materials and Methods
2.1 Clinical Study
We conducted a single-center clinical study (ClinicalTrials.gov, ID: NCT03337945) in 36 patients with liver cirrhosis and 12 matched control subjects. The study has been approved by the local ethics committee EKNZ (Ethikkommission Nordwestschweiz/Zentralschweiz, BASEC-Nr: 2017-01329) and was conducted in accordance with good clinical practice guidelines and the current version of the Declaration of Helsinki.
The 36 patients with liver cirrhosis were recruited during hospitalization for problems associated with liver disease at the University Hospital of Basel, Switzerland. The study was performed after discharge when the patients were in a stable clinical condition. Liver cirrhosis had been diagnosed histologically in all patients during the current or previous hospitalizations. After explanation of the study aims and study design, patients had a screening visit in the ambulatory study center of the University Hospital of Basel and eligible patients were included into the study after signing the informed consent. Hepatic encephalopathy stage III and IV, tense ascites, continued alcohol consumption, and ingestion of drugs interacting with the substrates of the Basel phenotyping cocktail (moderate and strong CYP inhibitors according to the US Food and Drug Administration) were exclusion criteria. Control subjects were mainly recruited from the hospital staff. They had to have no acute disease, no history of liver disease, normal liver function tests in the screening visit, and no drugs interfering with the metabolism of the six substrates in the Basel phenotyping cocktail. Excessive caffeine ingestion (> 800 mg/day) was an exclusion criterion for both patients and control subjects. One control subject was matched to three patients with liver cirrhosis regarding age (± 10 years), body mass index (± 10%), and sex.
The study subjects had to stop consuming caffeine containing nutrients 24 h prior to the phenotyping cocktail administration. They were not allowed to eat overnight before they arrived at the study center the next morning. A venous catheter was placed in the non-dominant forearm and a blood sample was withdrawn to determine the baseline caffeine and paraxanthine concentrations. The patients had to void their bladder before a 40% galactose infusion (0.5 g galactose per kg) was administered over 5 min. Venous blood samples were obtained 20, 35, and 50 min after start of the infusion into ethylenediaminetetraacetic acid-coated tubes and the urine was collected over 45 min. Blood samples were centrifuged at 1500g for 10 min at 4 °C and the plasma stored at − 80 °C until analysis. The urine volume was measured and an aliquot frozen at − 80 °C until analysis. 30 min after start of the galactose infusion, the Basel phenotyping cocktail capsule containing 10 mg of caffeine (CYP1A2 substrate), 50 mg of efavirenz (CYP2B6 substrate), 12.5 mg of flurbiprofen (CYP2C9 substrate), 10 mg of omeprazole (CYP2C19 substrate), 12.5 mg of metoprolol tartrate (CYP2D6 substrate), and 2 mg of midazolam (CYP3A substrate) was administered orally. Venous blood samples were obtained 5 min, 15 min, 30 min, 45 min, 1 h, 2 h, 3 h, 4 h, 6 h, 8 h, 12 h, and 24 h after cocktail administration into ethylenediaminetetraacetic acid-coated tubes. Samples were centrifuged at 1500g for 10 min at 4 °C and the plasma stored at − 80 °C until analysis. We have shown previously that there are no significant pharmacokinetic interactions between the compounds administered in the Basel phenotyping cocktail at these dosages [11].
2.2 Characterization of the Study Subjects
All study subjects were investigated clinically and biochemically to assess the functions of the liver and other organs as shown in Table 1, and in Table 2 of the ESM. This allowed the calculation of the Child score [26], which was used to categorize the patients with liver cirrhosis. Furthermore, the galactose elimination capacity [27, 28] and the plasma concentrations of unconjugated cholic acid and chenodeoxycholic acid were determined in all subjects to assess the metabolic function of the liver and the extent of portosystemic shunting [29], respectively.
2.3 Study Drugs
The Basel phenotyping cocktail capsules were prepared under good manufacturing practice conditions by Dr. Hysek Apotheke (Biel, Switzerland) as described previously [13]. The 40% galactose infusion (40 g/100 mL) was prepared under good manufacturing practice conditions by the Hospital Pharmacy of the University Hospital of Basel.
2.4 Bioanalysis
The substrates of the Basel phenotyping cocktail were quantified in plasma via high-performance liquid chromatography tandem mass spectrometry as described previously [30]. The plasma concentrations of caffeine, efavirenz, flurbiprofen, omeprazole, and metoprolol and their metabolites were determined without prior deglucuronidation, whereas for midazolam and 1′-OH-midazolam, the samples were first treated with β-glucuronidase (from Helix pomatia, ≥ 100,000 units/mL; Sigma-Aldrich, Buchs, Switzerland) [31]. Analyte extraction was performed by the addition of 150 µL of methanol to 50 µL of plasma. After vortex mixing for 1 min, the samples were centrifuged, and aliquots of the clear supernatant injected into the high-performance liquid chromatography tandem mass spectrometry system. The analyses were conducted on a Shimadzu (Kyoto, Japan) ultra-high pressure liquid chromatography system, which was connected to an API 5500 QTRAP mass spectrometer (Sciex, Concord, ON, Canada).
2.5 Measurement of Galactose Concentrations in Plasma and Urine
The galactose concentrations in plasma and urine samples were measured using the fluorometric assay kit ab83382 from Abcam (Lucerna-Chem AG; Luzern, Switzerland) following the instructions of the supplier.
2.6 Determination of the Galactose Elimination Capacity
In the concentration range assessed in the current study, galactose is eliminated by zero order kinetics [27]. The three plasma concentrations determined were plotted against time and the slope (ke) was determined by linear regression. C0 was determined as the intersection of the regression line with the y-axis and used to calculate the volume of distribution Vd:
where dose represents the dose of galactose administered. The amount of galactose metabolized and excreted over 50 min (A50min) was calculated as:
After subtraction of the amount eliminated by the urine over 50 min (U50min), the galactose elimination capacity (GEC) could be calculated as g galactose metabolized per min:
2.7 Measurement of Cholic Acid and Chenodeoxycholic Acid Concentrations
Cholic acid (Toronto Research Chemicals, Toronto, ON, Canada) and chenodeoxycholic acid (Merck, Schaffhausen, Switzerland) plasma concentrations were determined by high-performance liquid chromatography tandem mass spectrometry (API 5000; Sciex). An aliquot of 50 µL of plasma was extracted with 150 µL of acetonitrile, which contained 25 ng/mL of the internal standards, cholic acid-d4 (Toronto Research Chemicals), and chenodeoxycholic acid-d4 (Cerilliant, Round Rock, TX, USA). The samples were agitated for 30 min and afterwards centrifuged at 10 °C and 3220g for 30 min. An aliquot of 5 µL was injected into the liquid chromatography tandem mass spectrometry system.
Calibrators and quality control samples were prepared in charcoal-stripped plasma, which was extracted similarly as unknown samples. The calibration range covered 0.5–500 ng/mL and 0.5–1000 ng/mL for cholic acid and chenodeoxycholic acid, respectively. Samples with concentrations above the upper limit of quantification were diluted into the calibration range using charcoal-stripped plasma. Triplicates of six quality control levels (1, 2.5, 5, 50, 250, and 500 ng/mL) were included in each analytical run.
Water plus 0.1% formic acid and acetonitrile served as mobile phase A and B, respectively. Samples were on-line diluted with mobile phase A via a t-union, which was installed in front of the analytical column (Kinetex C18, 50 × 2.1 mm, 2.6 µm; Phenomenex, Torrance, CA, USA). The following gradient profile was used to separate the analytes: 0–0.5 min; 2% mobile B, 0.5–1 min; 2–30% mobile B, 1–7 min; 30–45% mobile B, 7–7.5 min; 45–95% mobile B, 7.5–8.5 min; 95% mobile B, 8.5–9 min; 2% mobile B. The flow rate was set a 0.5 mL/min and the column oven temperature at 35 °C. Cholic acid and chenodeoxycholic acid eluted after 3.8 min and 5.92 min, respectively. The analytes were detected by negative electrospray ionization and multiple reaction monitoring. The following mass transitions were used: cholic acid; m/z 407.3 → 407.3 (collision energy [CE]: − 40 V), cholic acid-d4; m/z 411.3 → 411.3 (CE: − 40 V), chenodeoxycholic acid: m/z 391.3 → 391.3 (CE: − 50 V), and chenodeoxycholic acid-d4: m/z 395.3 → 395.3 (CE: − 50 V).
The bioanalytical method was qualified considering method linearity, accuracy and precision, and selectivity. The method was linear over the applied calibration range (R ≥ 0.998), endogenous interferences were separated by the applied high-performance liquid chromatography gradient program, and the intra-assay accuracy was between 89.5 and 109.1% and the intra-assay precision was ≤ 6.4%.
2.8 Pharmacokinetic Analysis and Statistics
A primary endpoint of the study was the effect of liver cirrhosis on the metabolic activity of CYP1A2, 2B6, 2C9, 2C19, 2D6, and 3A. Cytochrome P450 activities were determined as the terminal elimination rate constant (ke) and as the MR of the six substrates used in the Basel phenotyping cocktail. We quantified the following reactions: caffeine to paraxanthine (CYP1A2), efavirenz to 8-hydroxyefavirenz (CYP2B6), flurbiprofen to 4-hydroxyflurbiprofen (CYP2C9), omeprazole to 5-hydroxyomeprazole (CYP2C19), metoprolol to α-hydroxymetoprolol (CYP2D6), and midazolam to 1′-hydroxymidazolam (CYP3A). The MR was calculated by dividing the AUC from 0 to 24 h (AUC0–24h) of the metabolite by the AUC0–24h of the respective parent drug. We performed non-compartmental pharmacokinetic analyses of plasma concentration–time curves of the study drugs and their metabolites using PKanalix (version 2019R1; Lixoft SAS, Antony, France). Values below the lower limit of quantification were put to zero. The number of values lower than the lower limit of quantification per analyte and timepoint are shown in Table 3 of the ESM. Maximum plasma concentration was obtained directly from the plotted plasma concentration–time profiles and the ke from the terminal linear part of the semilogarithmic plasma concentration–time plots (Table 1). The elimination half-lives (t½) were calculated as ln2/ke. Area under the plasma concentration–time curves were calculated using the linear trapezoidal method. Clearance divided by bioavailability (Cl/F) of the parent compounds was calculated by dividing the dose (Table 1 of the ESM) by the AUC from 0 to infinity, and the volume of distribution of the elimination phase (Vz/F) by dividing Cl/F by ke.
Considering the explorative nature of the study, we did not perform a formal power analysis. Differences between the study groups (controls and patients with Child A, Child B, and Child C liver cirrhosis) were analyzed by a one-way analysis of variance followed by the Holm–Sidak method for comparisons vs the control values. In the case of non-normally distributed values, an analysis of variance on ranks (Kruskal–Wallis) followed by Dunn’s method was performed. All analyses were conducted with GraphPad Prism 8 (Graphpad Software, La Jolla, CA, USA). Statistical significance was defined as p < 0.05.
3 Results
We investigated the pharmacokinetics of the six substrates in the Basel phenotyping cocktail in 16, 15, and 5 patients with Child A, Child B, and Child C liver cirrhosis, respectively, and in 12 matched control subjects. Compared with control subjects, patients with liver cirrhosis tended to be older but had similar body weights and body mass indexes (Table 1, and in Table 2 of the ESM). Patients with liver cirrhosis had higher activities of serum transaminases and alkaline phosphatase as well as higher serum bilirubin levels, but lower serum albumin levels. The galactose elimination capacity, a marker of the metabolic capacity of the liver [27, 28], decreased with increasing severity of liver cirrhosis, dropping to 18% in patients with Child C cirrhosis compared with controls. The prothrombin ratio and the factor V concentrations were reduced in patients with liver cirrhosis and, accordingly, the international normalized ratio was increased. The plasma concentrations of chenodeoxycholic acid and cholic acid were increased in patients with liver cirrhosis, reaching statistical significance compared to controls only for chenodeoxycholic acid because of a high variability.
The impact of liver cirrhosis on the pharmacokinetics of the low to moderate extraction drugs was limited for efavirenz and flurbiprofen but distinct for caffeine. Despite abstinence from caffeine ingestion during the 24 h before treatment with the Basel phenotyping cocktail, all subjects had residual plasma caffeine and paraxanthine concentrations, whereby the residual plasma caffeine concentration was higher in patients with liver cirrhosis compared with controls (control subjects 1.19 ± 0.24 µg/mL [n = 12; mean ± standard error of the mean], Child A: 1.44 ± 0.34 µg/mL [n = 16], Child B: 2.04 ± 0.49 µg/mL [n = 15], Child C: 7.49 ± 3.68 µg/mL [n = 5; p < 0.05 vs control]) (Fig. 1 and Table 2). Because of this high residual plasma caffeine concentration, the increment resulting from the exogenous caffeine (10 mg) could not be determined with certainty, precluding the calculation of Vz/F and Cl/F for caffeine. The caffeine elimination rate was numerically lower in patients with cirrhosis compared with controls but without reaching statistical significance because of a high variability. The caffeine MR0–24h decreased with the severity of liver cirrhosis, dropping to 12% in patients with Child C cirrhosis compared with controls. Similar to caffeine, the elimination rate of paraxanthine was decreased in patients with liver cirrhosis compared with control subjects (Fig. 1 and Table 3).
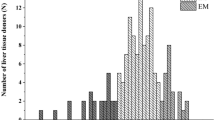
Pharmacokinetics of substrates with a low to moderate hepatic extraction. Plasma concentration–time profiles were assessed in n = 16 patients with Child A cirrhosis, n = 15 patients with Child B cirrhosis, n = 5 patients with Child C cirrhosis, and in 12 matched control subjects. The insert displays the semi-logarithmical presentation of the data. The calculated pharmacokinetic variables are displayed in Table 2. Data are presented as mean ± standard error of the mean
In comparison to caffeine, liver cirrhosis affected the metabolism of efavirenz less strongly (Fig. 1 and Table 2). Liver cirrhosis did not significantly affect efavirenz elimination, exposure, Vz/F, or Cl/F. Regarding the elimination rate constant ke and half-life of efavirenz, the short sampling time (24 h) of the current study must be taken into account. The half-life was clearly shorter in the current study (17.4 h in control subjects) than the 52–74 h reported in studies with longer sampling times [32]. The short sampling time may have mitigated the effect of liver cirrhosis on efavirenz elimination. The MR0–24h of efavirenz decreased significantly with the severity of liver cirrhosis, dropping to 58% in patients with Child C cirrhosis compared with control subjects. In comparison, liver cirrhosis did not significantly affect the pharmacokinetics of 8-hydroxyefavirenz (Table 3). As shown in Fig. 1 and Table 2, the pharmacokinetics and MR0–24h of flurbiprofen were not significantly affected by liver cirrhosis. Accordingly, the effect of liver cirrhosis on the pharmacokinetics of 4-hydroxyflurbiprofen was minimal with a 58% increase in the AUC0–24h, which reached statistical significance (Fig. 1 and Table 3).
In contrast to the low to moderate extraction drugs, liver cirrhosis had a large impact on the pharmacokinetics of moderate to high extraction drugs (Fig. 2, Tables 3 and 4). Regarding omeprazole, patients with liver cirrhosis had a large decrease in the elimination rate and an increase in exposure, resulting in a decrease in the omeprazole Cl/F by 91% in Child C cirrhosis compared with control subjects. Because of the increase in omeprazole exposure, the MR0–24h showed a marked drop in patients with liver cirrhosis; this drop reached 92% in Child C cirrhosis compared with control subjects. Similarly, patients with liver cirrhosis had a reduced elimination rate and Vz/F of metoprolol, resulting in a reduction in Cl/F, which dropped to 22% in patients with Child C cirrhosis compared with control subjects. With increasing severity of liver cirrhosis, the MR0–24h of metoprolol decreased, amounting to 21% in patients with Child C cirrhosis compared with control subjects.
Pharmacokinetics of substrates with a moderate to high hepatic extraction. Plasma concentration–time profiles were assessed in n = 16 patients with Child A cirrhosis, n = 15 patients with Child B cirrhosis, n = 5 patients with Child C cirrhosis, and in 12 matched control subjects. The insert displays the semi-logarithmical presentation of the data. The calculated pharmacokinetic variables are displayed in Table 4. Data are presented as mean ± standard error of the mean
For midazolam, we deglucuronidated the plasma samples before quantification because 1′-hydroxymidazolam is rapidly and almost completely glucuronidated [33] and the MR0–24h provides more reliable results when the total (glucuronidated and non-glucuronidated) 1′-hydroxymidazolam is used for the calculation [31]. Similar to omeprazole and metoprolol, the elimination rate of midazolam decreased with increasing severity of liver cirrhosis, resulting in a higher exposure and lower Cl/F (drop by 84% in patients with Child C cirrhosis compared with control subjects). The MR0–24h was decreased in severe liver cirrhosis, dropping to 33% in patients with Child C cirrhosis compared with control subjects.
As shown in Table 4 of the ESM, we found significant linear correlations between liver function tests and pharmacokinetic parameters. As expected, such correlations were mainly present for the moderate to high extraction drugs omeprazole, metoprolol, and midazolam, whose pharmacokinetics were predominantly affected by liver cirrhosis. The galactose elimination capacity, serum bilirubin, markers of protein synthesis (serum albumin, prothrombin ratio, and factor V activity), and the bile acids (chenodeoxycholic acid and cholic acid) showed the best correlations with the pharmacokinetic variables. The correlations of the prothrombin ratio with the elimination rate constant and the MR0–24h for the substrates used are shown in Figs. 3 and 4, respectively. The figures show that the prothrombin ratio has tighter correlations with the elimination rate constant than with the MR0–24h and that significant correlations between the prothrombin ratio and the two pharmacokinetic variables mainly exist for omeprazole, metoprolol, and midazolam.
Linear correlation of the prothrombin ratio with the terminal elimination rate constant (ke) for the substrates used in the Basel phenotyping cocktail. The population studied included n = 16 patients with Child A cirrhosis, n = 15 patients with Child B cirrhosis, n = 5 patients with Child C cirrhosis, and in 12 matched control subjects. ke terminal elimination rate constant
Linear correlation of the prothrombin ratio with the metabolic ratio for the substrates used in the Basel phenotyping cocktail. The population studied included n = 16 patients with Child A cirrhosis, n = 15 patients with Child B cirrhosis, n = 5 patients with Child C cirrhosis, and in 12 matched control subjects. The metabolic ratio was calculated as the ratio of area under the plasma concentration–time curve from 0 to 24 h for the specific metabolite and area under the plasma concentration–time curve from 0 to 24 h for the parent drug
Next, we estimated the effect of liver cirrhosis on the activity of the CYPs involved in the metabolism of the six substrates of the Basel phenotyping cocktail using the elimination rate constant and MR0–24h as markers for CYP activity. The main reason to use these two parameters is the fact that they are independent of bioavailability. This is important because the presence of portosystemic shunts in patients with liver cirrhosis leads to an increase of the bioavailability of drugs with a moderate to high hepatic extraction [6, 22]. As shown in Fig. 5, the results obtained with the elimination rate constant and MR0–24h were similar, showing a decrease in CYP activity depending on the CYP assessed and on the severity of liver cirrhosis. The only exception was CYP2C9 (flurbiprofen), for which we had not observed a significant effect of liver cirrhosis on the elimination rate constant or MR0–24h (Table 2). The mean reductions in CYP activity in patients with Child C cirrhosis were 72% for CYP1A2, 36% for CYP2B6, 84% for CYP2C19, 58% for CYP2D6, and 70% for CYP3A.
Effect of liver cirrhosis on cytochrome P450 enzyme (CYP) activity. The population studied included n = 16 patients with Child A cirrhosis, n = 15 patients with Child B cirrhosis, n = 5 patients with Child C cirrhosis, and in 12 matched control subjects. Cytochrome P450 enzyme activity was estimated based on the elimination rate constant (ke) or on the metabolic ratio (MR0–24h) of the substrates used in the Basel phenotyping cocktail. The substrates included caffeine (CYP1A2), efavirenz (CYP2B6), flurbiprofen (CYP2C9), omeprazole (CYP2C19), metoprolol (CYP2D6), and midazolam (CYP3A). The MR was calculated as the ratio of area under the plasma concentration–time curve from 0 to 24 h for the specific metabolite and area under the plasma concentration–time curve from 0 to 24 h for the parent drug. Data are displayed as individual values and mean ± standard error of the mean. ke terminal elimination rate constant, *p < 0.05 between patients with liver cirrhosis according to Child class vs control subjects
4 Discussion and Conclusions
The principal aims of the current study were to assess the pharmacokinetics of the six substrates and their specific metabolites of the Basel phenotyping cocktail and to determine the activity of the CYPs that metabolize these substrates in patients with liver cirrhosis. We included 48 subjects into the study, yielding 576 individual pharmacokinetic profiles.
The substrates in the Basel phenotyping cocktail comprise two low to moderate (caffeine and flurbiprofen) and three moderate to high extraction drugs (omeprazole, metoprolol, and midazolam) (Table 1). The classification of efavirenz is unclear as the absolute bioavailability and hepatic extraction in humans is not known. Assuming the same bioavailability in humans as in monkeys (42%) [32], efavirenz would be classified as a moderate extraction drug. However, the bioavailability of efavirenz is primarily limited by its low water solubility and not by hepatic extraction [32], which could shift it into the category of the low extraction drugs. As expected, the effect of liver cirrhosis was clearly evident for the moderate to high extraction substrates, with a reduction in Cl/F and in the elimination rate for omeprazole, metoprolol, and midazolam. In theory, liver blood flow, and not CYP activity, should limit the hepatic metabolism of high-extraction compounds [34], rendering midazolam potentially useless as a marker for CYP activity. In three publications where midazolam was administered intravenously, the volume of distribution was not different between patients with liver cirrhosis and control subjects [20,21,22]. Assuming that the same is true for the subjects of the current study, the ratio of the bioavailabilities Fcirrhosis Child C/Fcontrols equals 1.73. Assuming a bioavailability of 30% in healthy persons [35, 36], this would result in a bioavailability of 50–60% in patients with Child C cirrhosis, matching well with reported data [36]. Using these values for bioavailability, the corresponding clearances can be calculated as approximately 80 L/h in controls and 35 L/h in patients with Child C cirrhosis, showing the clearance of midazolam is impaired in patients with liver cirrhosis also after correction for bioavailability. This indicates that portosystemic shunts, which are mainly responsible for the increase in bioavailability, cannot entirely explain the decrease in Cl/F of midazolam in patients with liver cirrhosis, suggesting that a reduced function of CYP3A at least contributes to the impaired metabolism of midazolam in this group of patients. This is supported by the decreases in the elimination rate constant and in MR0–24h, which we consider to be independent of bioavailability. Similarly, for omeprazole and metoprolol, two moderate extraction drugs, the effect of liver cirrhosis on Cl/F was more accentuated than on Vz/F, suggesting a negative effect of liver cirrhosis on the activity of CYP2C19 and CYP2D6, respectively. In addition for these substrates, the impact of liver cirrhosis on their pharmacokinetics is evidenced by the decrease in the respective elimination rate constant and MR0–24h.
The effects of liver cirrhosis observed in the current study match well with data reported in the literature for omeprazole [37, 38], metoprolol [39], and midazolam [20,21,22,23]. This demonstrates that the cocktail approach cannot only be used to obtain MRs but can provide also entire plasma concentration–time profiles for pharmacokinetic calculations. Similar to the findings in the current study, these earlier publications showed that liver cirrhosis decreases the elimination rate with a corresponding increase in the terminal half-life and decreases the clearance of moderate to high extraction drugs, whereas the volume of distribution remains unchanged. In the studies, where the absolute bioavailability was measured, the expected increase in patients with liver cirrhosis was demonstrated [22, 37, 39].
In comparison to the moderate to high extraction drugs, the effect of liver cirrhosis on the pharmacokinetics of the low to moderate extraction drugs caffeine, efavirenz, and flurbiprofen was much less accentuated. In contrast to caffeine, efavirenz and flurbiprofen have a high protein binding (Table 1 of the ESM), which is usually associated with an increase in the free fraction (and possibly free concentration) of such drugs in patients with liver cirrhosis [8, 20, 22], potentially overriding a negative effect of liver cirrhosis on drug clearance. As shown in Table 2, this appears to be the case for efavirenz and flurbiprofen. As the MR0–24h may be influenced by protein binding (protein binding between the parent drug and the metabolite may be different), the elimination rate constant, which is independent of protein binding [8, 20], may represent the best marker for CYP activity for such compounds. The results of the current study show a significant decrease in the MR0–24h for caffeine and efavirenz but no significant effect on elimination rate constant or MR0–24h of flurbiprofen. The effect of liver cirrhosis on the metabolism of caffeine has been reported earlier [15, 16], and caffeine has been proposed as a marker of the metabolic capacity of the liver [27]. Because caffeine has a low protein binding (Table 1 of the ESM), protein binding does not influence its hepatic clearance, which therefore mainly depends on the activity of CYP1A2. This dependence on only one CYP must be taken into account when caffeine is used as a marker of liver function.
In contrast to caffeine, the pharmacokinetics of efavirenz and flurbiprofen have so far not been reported in patients with liver cirrhosis. Both drugs are highly protein bound, which must be taken into account for the interpretation of their pharmacokinetic data. Considering flurbiprofen, liver cirrhosis did not significantly affect its pharmacokinetic properties. In comparison, regarding efavirenz, liver cirrhosis was associated with a 30% numerical decrease and a significant 42% decrease in the MR0–24h in patients with Child C cirrhosis, suggesting a decrease in the activity of CYP2B6.
A second aim of the study was to determine the activity of the CYPs involved in the metabolism of the substrates of the Basel phenotyping cocktail. The markers used for CYP activity should be independent of protein binding and bioavailability, which can change substantially in patients with liver cirrhosis [4]. An ideal candidate is the elimination rate constant, which is independent of both protein binding and bioavailability if protein binding of the drug considered is not saturable [8]. The MR can be considered to be independent of bioavailability but may not be independent of protein binding, which may differ between parent compound and metabolite. This is almost certainly the case for midazolam, where we used the total 1′-hydroxymidazolam concentration (mainly consisting of the 1′-O-glucuronide metabolite, which is more polar than midazolam and therefore has most probably a lower protein binding than midazolam) for the calculation of the MR0–24h. However, the results regarding the effect on CYP3A activity were similar for the elimination rate constant and MR0–24h as markers (Fig. 5), suggesting that protein binding had no relevant impact on the MR0–24h of midazolam. As shown in Fig. 5, the effect of liver cirrhosis on CYP activity depends on both the severity of cirrhosis and on the CYP considered. Whereas CYP2C9 was not significantly affected by liver cirrhosis, the activities of CYP1A2, 2B6, 2C19, 2D6, and 3A were reduced in patients with Child C cirrhosis, with CYP2C19 activity being reduced already in patients with Child A cirrhosis. Activities of CYP1A2 and CYP3A4 in liver microsomes or liver biopsies from patients with liver cirrhosis were in the range of 20–30% and 30–70% of control activities [40,41,42], respectively, which is similar to the findings in the current study. Protein expression data showed a drop to 20–29% for CYP1A2, 44–57% for 2C9, 68% for CYP2D6, and 11–25% for CYP3A4 in liver microsomes from patients with liver cirrhosis compared with control subjects [41, 43]. The protein expression appears to be lower than the respective activity, which may be due to contamination of the microsomal preparation with non-hepatocyte microsomes. For dose adjustments, the functional data are therefore more relevant than the protein expression data. In two studies, the mRNA expressions of different CYPs were also assessed, which roughly correlated with the protein expression data, suggesting that the decrease in CYP activity in liver cirrhosis is due to impaired transcription [42, 44]. The reasons why liver cirrhosis affects CYP transcription have so far not been reported.
As shown in Table 4 of the ESM and in Figs. 3 and 4, there were multiple significant linear correlations between liver function parameters and pharmacokinetic variables. However, the correlations were not strong enough that liver function tests could be recommended as surrogates for CYP activity. In addition, the variable effect of liver cirrhosis on the activity of the individual CYPs precludes the use of liver function parameters as a surrogate for CYP activity.
The study has several limitations. First, we did not genotype the subjects included. Although the influence of liver cirrhosis on the pharmacokinetics of most substrates is evident, we cannot exclude additional effects by the underlying genotype. Second, oral ingestion of the probe drugs includes not only hepatic but also intestinal metabolism and the metabolites formed are usually further metabolized, which has an impact on the MR. These are arguments to use the elimination rate constant as a marker for CYP activity, which avoids these weaknesses. Third, the parent drug may not only be metabolized by the CYP investigated but also by other CYPs [45], which can impair the informative value of the MR.
In conclusion, liver cirrhosis affects CYP activity differently, depending on the severity of cirrhosis and of the CYP considered. The cocktail approach is suitable to assess the activity of different CYPs in patients with liver cirrhosis in one step.
References
Franz CC, Egger S, Born C, Rätz Bravo AE, Krähenbühl S. Potential drug-drug interactions and adverse drug reactions in patients with liver cirrhosis. Eur J Clin Pharmacol. 2012;68(2):179–88.
Lucena MI, Andrade RJ, Tognoni G, Hidalgo R, De La Cuesta FS. Multicenter hospital study on prescribing patterns for prophylaxis and treatment of complications of cirrhosis. Eur J Clin Pharmacol. 2002;58(6):435–40.
Lucena MI, Andrade RJ, Tognoni G, Hidalgo R, de la Cuesta FS. Drug use for non-hepatic associated conditions in patients with liver cirrhosis. Eur J Clin Pharmacol. 2003;59(1):71–6.
Delco F, Tchambaz L, Schlienger R, Drewe J, Krahenbuhl S. Dose adjustment in patients with liver disease. Drug Saf. 2005;28(6):529–45.
Johnson TN, Boussery K, Rowland-Yeo K, Tucker GT, Rostami-Hodjegan A. A semi-mechanistic model to predict the effects of liver cirrhosis on drug clearance. Clin Pharmacokinet. 2010;49(3):189–206.
Taegtmeyer AB, Haschke M, Tchambaz L, Buylaert M, Tschopl M, Beuers U, et al. A study of the relationship between serum bile acids and propranolol pharmacokinetics and pharmacodynamics in patients with liver cirrhosis and in healthy controls. PLoS ONE. 2014;9(6): e97885.
Franz CC, Hildbrand C, Born C, Egger S, Rätz Bravo AE, Krähenbühl S. Dose adjustment in patients with liver cirrhosis: impact on adverse drug reactions and hospitalizations. Eur J Clin Pharmacol. 2013;69(8):1565–73.
Berger B, Dingemanse J, Sabattini G, Delahaye S, Duthaler U, Muehlan C, et al. Effect of liver cirrhosis on the pharmacokinetics, metabolism, and tolerability of daridorexant, a novel dual orexin receptor antagonist. Clin Pharmacokinet. 2021;60(10):1349–60.
Nebert DW, Russell DW. Clinical importance of the cytochromes P450. Lancet. 2002;360(9340):1155–62.
Derungs A, Donzelli M, Berger B, Noppen C, Krähenbühl S, Haschke M. Effects of cytochrome P450 inhibition and induction on the phenotyping metrics of the Basel cocktail: a randomized crossover study. Clin Pharmacokinet. 2016;55(1):79–91.
Donzelli M, Derungs A, Serratore MG, Noppen C, Nezic L, Krahenbuhl S, et al. The basel cocktail for simultaneous phenotyping of human cytochrome P450 isoforms in plasma, saliva and dried blood spots. Clin Pharmacokinet. 2014;53(3):271–82.
Suenderhauf C, Berger B, Puchkov M, Schmid Y, Muller S, Huwyler J, et al. Pharmacokinetics and phenotyping properties of the Basel phenotyping cocktail combination capsule in healthy male adults. Br J Clin Pharmacol. 2020;86(2):352–61.
Camblin M, Berger B, Haschke M, Krahenbuhl S, Huwyler J, Puchkov M. CombiCap, a novel drug formulation for the Basel phenotyping cocktail. Int J Pharm. 2016;512(1):253–61.
Frye RF, Zgheib NK, Matzke GR, Chaves-Gnecco D, Rabinovitz M, Shaikh OS, et al. Liver disease selectively modulates cytochrome P450-mediated metabolism. Clin Pharmacol Ther. 2006;80(3):235–45.
Kraul H, Truckenbrodt J, Huster A, Töpfer R, Hoffmann A. Comparison of in vitro and in vivo biotransformation in patients with liver disease of differing severity. Eur J Clin Pharmacol. 1991;41(5):475–80.
Renner E, Wietholtz H, Huguenin P, Arnaud MJ, Preisig R. Caffeine: a model compound for measuring liver function. Hepatology. 1984;4(1):38–46.
Adedoyin A, Arns PA, Richards WO, Wilkinson GR, Branch RA. Selective effect of liver disease on the activities of specific metabolizing enzymes: investigation of cytochromes P450 2C19 and 2D6. Clin Pharmacol Ther. 1998;64(1):8–17.
Ohnishi A, Murakami S, Akizuki S, Mochizuki J, Echizen H, Takagi I. In vivo metabolic activity of CYP2C19 and CYP3A in relation to CYP2C19 genetic polymorphism in chronic liver disease. J Clin Pharmacol. 2005;45(11):1221–9.
Larrey D, Babany G, Tinel M, Freneaux E, Amouyal G, Habersetzer F, et al. Effect of liver disease on dextromethorphan oxidation capacity and phenotype: a study in 107 patients. Br J Clin Pharmacol. 1989;28(3):297–304.
Albarmawi A, Czock D, Gauss A, Ehehalt R, Lorenzo Bermejo J, Burhenne J, et al. CYP3A activity in severe liver cirrhosis correlates with Child-Pugh and model for end-stage liver disease (MELD) scores. Br J Clin Pharmacol. 2014;77(1):160–9.
MacGilchrist AJ, Birnie GG, Cook A, Scobie G, Murray T, Watkinson G, et al. Pharmacokinetics and pharmacodynamics of intravenous midazolam in patients with severe alcoholic cirrhosis. Gut. 1986;27(2):190–5.
Pentikäinen PJ, Välisalmi L, Himberg JJ, Crevoisier C. Pharmacokinetics of midazolam following intravenous and oral administration in patients with chronic liver disease and in healthy subjects. J Clin Pharmacol. 1989;29(3):272–7.
Trouvin JH, Farinotti R, Haberer JP, Servin F, Chauvin M, Duvaldestin P. Pharmacokinetics of midazolam in anaesthetized cirrhotic patients. Br J Anaesth. 1988;60(7):762–7.
Bickel M, Stephan C, Rottmann C, Carlebach A, Haberl A, Kurowski M, et al. Severe CNS side-effect and persistent high efavirenz plasma levels in a patient with HIV/HCV coinfection and liver cirrhosis. Scand J Infect Dis. 2005;37(6–7):520–2.
Meynard JL, Lacombe K, Poirier JM, Legrand J, Morand-Joubert L, Girard PM. Influence of liver fibrosis stage on plasma levels of efavirenz in HIV-infected patients with chronic hepatitis B or C. J Antimicrob Chemother. 2009;63(3):579–84.
Conn HO. A peek at the Child-Turcotte classification. Hepatology. 1981;1(6):673–6.
Preisig R. Foreign substances as indicators of liver function. Schweiz Med Wochenschr Suppl. 1985;19:36–42.
Reichen J, Widmer T, Cotting J. Accurate prediction of death by serial determination of galactose elimination capacity in primary biliary cirrhosis: a comparison with the Mayo model. Hepatology. 1991;14(3):504–10.
Ohnishi K, Chin N, Sugita S, Saito M, Tanaka H, Terabayashi H, et al. Quantitative aspects of portal-systemic and arteriovenous shunts within the liver in cirrhosis. Gastroenterology. 1987;93(1):129–34.
Bachmann F, Blaser L, Haschke M, Krähenbühl S, Duthaler U. Development and validation of an LC-MS/MS method for the bioanalysis of the major metamizole metabolites in human plasma. Bioanalysis. 2020;12(3):175–89.
Bachmann F, Duthaler U, Krähenbühl S. Effect of deglucuronidation on the results of the Basel phenotyping cocktail. Br J Clin Pharmacol. 2021;87(12):4608–18.
Cristofoletti R, Nair A, Abrahamsson B, Groot DW, Kopp S, Langguth P, et al. Biowaiver monographs for immediate release solid oral dosage forms: efavirenz. J Pharm Sci. 2013;102(2):318–29.
Link B, Haschke M, Grignaschi N, Bodmer M, Aschmann YZ, Wenk M, et al. Pharmacokinetics of intravenous and oral midazolam in plasma and saliva in humans: usefulness of saliva as matrix for CYP3A phenotyping. Br J Clin Pharmacol. 2008;66(4):473–84.
Wilkinson GR, Shand DG. Commentary: a physiological approach to hepatic drug clearance. Clin Pharmacol Ther. 1975;18(4):377–90.
Kupferschmidt HH, Ha HR, Ziegler WH, Meier PJ, Krähenbühl S. Interaction between grapefruit juice and midazolam in humans. Clin Pharmacol Ther. 1995;58(1):20–8.
Pentikainen PJ, Valisalmi L, Himberg JJ, Crevoisier C. Pharmacokinetics of midazolam following intravenous and oral administration in patients with chronic liver disease and in healthy subjects. J Clin Pharmacol. 1989;29(3):272–7.
Andersson T, Olsson R, Regårdh CG, Skånberg I. Pharmacokinetics of [14C]omeprazole in patients with liver cirrhosis. Clin Pharmacokinet. 1993;24(1):71–8.
Kumar R, Chawla YK, Garg SK, Dixit RK, Satapathy SK, Dhiman RK, et al. Pharmacokinetics of omeprazole in patients with liver cirrhosis and extrahepatic portal venous obstruction. Methods Find Exp Clin Pharmacol. 2003;25(8):625–30.
Regårdh CG, Jordö L, Ervik M, Lundborg P, Olsson R, Rönn O. Pharmacokinetics of metoprolol in patients with hepatic cirrhosis. Clin Pharmacokinet. 1981;6(5):375–88.
Farrell GC, Cooksley WG, Powell LW. Drug metabolism in liver disease: activity of hepatic microsomal metabolizing enzymes. Clin Pharmacol Ther. 1979;26(4):483–92.
George J, Murray M, Byth K, Farrell GC. Differential alterations of cytochrome P450 proteins in livers from patients with severe chronic liver disease. Hepatology. 1995;21(1):120–8.
Yang LQ, Li SJ, Cao YF, Man XB, Yu WF, Wang HY, et al. Different alterations of cytochrome P450 3A4 isoform and its gene expression in livers of patients with chronic liver diseases. World J Gastroenterol. 2003;9(2):359–63.
Prasad B, Bhatt DK, Johnson K, Chapa R, Chu X, Salphati L, et al. Abundance of phase 1 and 2 drug-metabolizing enzymes in alcoholic and hepatitis C cirrhotic livers: a quantitative targeted proteomics study. Drug Metab Dispos. 2018;46(7):943–52.
George J, Liddle C, Murray M, Byth K, Farrell GC. Pre-translational regulation of cytochrome P450 genes is responsible for disease-specific changes of individual P450 enzymes among patients with cirrhosis. Biochem Pharmacol. 1995;49(7):873–81.
Berger B, Bachmann F, Duthaler U, Krähenbühl S, Haschke M. Cytochrome P450 enzymes involved in metoprolol metabolism and use of metoprolol as a CYP2D6 phenotyping probe drug. Front Pharmacol. 2018;9:774.
Acknowledgments
We thank the study nurses Claudia Bläsi and Joyce Jesus de Santos, the laboratory technician Beatrice Vetter, and Dr. Tim Bühler for their valuable help in organizing and performing the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding provided by University of Basel. The study was financed by a grant of the University of Basel to CS and by funds of the Department of Clinical Pharmacology and Toxicology of the University Hospital of Basel.
Conflict of interest
None of the authors reports a conflict of interest regarding this study.
Ethics approval
The study has been approved by the local ethics committee EKNZ (Ethikkommission Nordwestschweiz/Zentralschweiz, BASEC-Nr: 2017-01329) and was conducted in accordance with good clinical practice guidelines and the current version of the Declaration of Helsinki.
Consent to participate
The study subjects signed the informed consent sheet.
Consent for publication
The informed consent sheet also contained the consent of the participants for publication.
Availability of data and material
Data are available on request.
Code availability
Not applicable.
Author contributions
UD and SK wrote the manuscript, FB, CS, MH, and SK designed the research, FB, TG, FP, PH, JB, and SK performed the research, UD, FB, and SK analyzed data, and UD and FB contributed analytical tools.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Duthaler, U., Bachmann, F., Suenderhauf, C. et al. Liver Cirrhosis Affects the Pharmacokinetics of the Six Substrates of the Basel Phenotyping Cocktail Differently. Clin Pharmacokinet 61, 1039–1055 (2022). https://doi.org/10.1007/s40262-022-01119-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-022-01119-0