Abstract
Background and Objective
Data on real-world healthcare costs for ixekizumab (IXE) and secukinumab (SEC) in biologic-experienced patients with psoriasis are limited. This study compared real-world costs and healthcare resource utilization between IXE and SEC in biologic-experienced patients with psoriasis over an 18-month follow-up period in the USA.
Methods
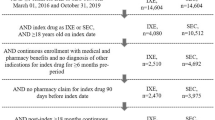
Adult patients with a diagnosis of psoriasis between 1 March, 2015 and 31 October, 2019 were identified using health insurance claims data from IBM Watson Health MarketScan®. The index date was the date of the first IXE or SEC claim. Biologic-experienced patients with one or more pre-period claims for biologic drugs were identified. Inverse probability of treatment weighting was used to reduce cohort imbalances. All-cause and psoriasis-related direct healthcare costs along with index drug costs were estimated during the follow-up and reported as per patient per month. Discount factors published by the Institute for Clinical and Economic Review were applied to psoriasis-related biologics to adjust pharmacy costs.
Results
A total of 411 IXE and 780 SEC users were included. After weighting, all-cause inpatient admissions were similar between IXE (9.5%) and SEC users (10.3%). Weighted, mean ± standard deviation per patient per month all-cause healthcare costs were higher in IXE users ($6670 ± $2910) than in SEC users ($6239 ± $3903; p = 0.049). Psoriasis-related and monthly index drug costs were higher in IXE users ($5609 ± $2009; p < 0.001 and $4688 ± $1994; p < 0.001, respectively) than in SEC users ($5095 ± $2291 and $3853 ± $1977, respectively). After Institute for Clinical and Economic Review adjustment, mean per patient per month all-cause ($4363 ± $2576 vs $4398 ± $3517) and psoriasis-related costs ($3302 ± $1264 vs $3253 ± $1504) were similar between the groups. Institute for Clinical and Economic Review- and adherence-adjusted mean per patient per month index drug costs were similar between IXE and SEC users (p = 0.339).
Conclusions
Institute for Clinical and Economic Review-adjusted all-cause and psoriasis-related costs were comparable between IXE and SEC users among biologic-experienced patients over an 18-month follow-up period.
Similar content being viewed by others
Data from phase III trials demonstrated positive efficacy results for ixekizumab and secukinumab in biologic-experienced patients with psoriasis who were previously treated with anti-tumor necrosis factors. |
In the present study, after applying Institute for Clinical and Economic Review adjustments, all-cause and psoriasis-related costs were comparable between ixekizumab and secukinumab users among biologic-experienced patients over an 18-month follow-up period. |
These results may be important to clinicians when making decisions regarding biologic treatment and their associated cost burden for patients with psoriasis, especially for those with prior use of biologics. |
1 Introduction
Psoriasis is a chronic inflammatory skin disease [1] that is estimated to affect > 8 million people in the USA [2]. Psoriasis increases the physical and psychosocial burden of patients and is associated with high direct and indirect medical costs, healthcare resource utilization (HCRU), and reduced work productivity [3, 4]. In the USA, psoriasis-related direct healthcare costs were $51.7–$63.2 billion and indirect costs (owing to presenteeism, absenteeism, and unemployment) were $23.9–$35.4 billion for the year 2013 [3]. In addition, comorbidities associated with psoriasis impose a substantial economic burden on society, with an estimated annual contribution of $36.4 billion [3, 5]. Furthermore, patients with moderate-to-severe psoriasis are more likely to incur additional costs because of inpatient admissions, emergency room visits, and outpatient visits compared with those without psoriasis [6].
The currently available and approved biologics for psoriasis include tumor necrosis factor inhibitors, interleukin-12/23 inhibitors, interleukin-17 inhibitors, and interleukin-23 inhibitors [7]. Although prior biologic use is known to be associated with lower future biologic efficacy when compared with biologic-naïve patients, both ixekizumab (IXE) and secukinumab (SEC) demonstrated positive efficacy in phase III trials in biologic-experienced patients previously treated with tumor necrosis factor inhibitors [8, 9].
Our previously published results during a 1-year follow-up suggested that patients with psoriasis who received either IXE or SEC incurred similar real-world healthcare costs after adjusting for drug discount programs using estimates from the Institute for Clinical and Economic Review (ICER) [10]. However, data describing real-world costs for IXE and SEC in biologic-experienced patients with psoriasis are limited. Thus, in this study, using claims data and accounting for payer discount over 18 months, we compared real-world costs, HCRU, and comorbidity-related costs between IXE and SEC treatments for patients with psoriasis in the USA who were previously treated with biologics.
2 Methods
2.1 Study Design and Data Sources
This retrospective observational study used health insurance claims data between 1 March, 2015 and 31 October, 2019 from the IBM Watson Health MarketScan® Research Databases, Commercial Database, Medicare Supplemental Database, and Early View Database [11].
The MarketScan Commercial Database includes inpatient, outpatient, pharmaceutical, and health plan enrollment data of employees and their dependents covered by employer-sponsored private health insurance in the USA. The Medicare Supplemental Database contains the above information for retirees with Medicare supplemental insurance paid for by employers. The Early View Database includes the same components for healthcare services incurred as late as approximately 60 days before the data release.
All data were obtained using International Classification of Diseases, Ninth/Tenth Revisions, Clinical Modification (ICD-9-CM/ICD-10-CM) codes, Current Procedural Terminology, 4th edition codes, Healthcare Common Procedure Coding System codes, and National Drug Code numbers. All database records were statistically de-identified and certified to be fully compliant with US patient confidentiality requirements outlined in the Health Insurance Portability and Accountability Act of 1996. This study used only deidentified patient records and did not involve the collection, use, or transmittal of individually identifiable data; therefore, institutional review board approval was not necessary.
2.2 Patient Cohort and Selection
To mitigate data coding limitations and data entry errors, patients with one or more inpatient or two or more non-diagnostic outpatient claims (at least 30 days apart) with a diagnosis of psoriasis (ICD-9-CM diagnosis code 696.1x or ICD-10-CM diagnosis codes L40.0–L40.4 or L40.8–L40.9) were identified between 1 March, 2015 and 31 October, 2019. One inpatient diagnosis for psoriasis was considered sufficient as they are more reliable, whereas, for outpatients, two or more diagnoses were considered because they generally return to their healthcare provider for continued treatment. Patients were required to have at least one claim for the index drug (IXE or SEC) between 1 March, 2016 and 31 October, 2019, with a diagnosis of psoriasis before or coinciding with the first claim for that index drug. The date of the first IXE or SEC claim was considered the index date and patients were classified as IXE or SEC users, based on the drug received at the index.
Biologic-experienced patients were identified as patients with one or more claims of the following biologic drugs indicated for psoriasis during a 6-month pre-period: certolizumab pegol, etanercept, adalimumab, infliximab, brodalumab, ustekinumab, guselkumab, SEC, and IXE. Risankizumab was not included, as it was approved on 23 April, 2019. Other inclusion criteria were ≥ 18 years of age at the index date with continuous enrollment with medical and pharmacy benefits for at least 6 months before the index date and 18 months after the index date (post-period). Patients diagnosed with psoriatic arthritis or ankylosing spondylitis (indications approved for IXE or SEC) during the pre-period were excluded. In addition, patients with the index medication claim within 90 days before the index date were excluded.
2.3 Healthcare Resource Utilization
Healthcare resource utilization was reported for the following categories: (a) inpatient; (b) outpatient (emergency room, office visit, other outpatient services), and (c) outpatient prescription. For inpatient services, the number and percentage of patients with an inpatient admission, count of inpatient admissions, and average length of inpatient stay per inpatient admission were reported. All outpatient categories were reported as the number and percentage of patients with a visit and count of visits, and outpatient prescriptions were reported as the number and percentage of patients with an outpatient prescription and count of prescriptions.
All utilization measures were reported as per patient per month (PPPM). For psoriasis-specific utilization, office-administered biologics were also captured and reported. Psoriasis-specific utilization was captured based on inpatient claims with a primary diagnosis for psoriasis, outpatient claims with a psoriasis diagnosis in any position, and medication treatment specifically for psoriasis. All-cause and psoriasis-specific HCRU were measured during the 18-month follow-up period.
2.4 Healthcare Costs (Unadjusted)
The unadjusted all-cause and psoriasis-related direct healthcare costs along with index drug costs for IXE and SEC users were estimated over an 18-month follow-up. Psoriasis-related costs were based on a similar approach as outlined above for psoriasis-specific utilization. Costs were reported in total and by service category, including inpatient services, outpatient services, and outpatient pharmacy. Healthcare costs were estimated using paid amounts of adjudicated claims, including insurer and health plan payments along with patient cost-sharing (co-payment, deductible, and coinsurance). The cost for services provided under capitated arrangements was estimated using the payment proxies. These payment proxies from the Commercial and Medicare Supplemental Databases were based on paid claims at the procedure level. All costs were adjusted to 2019 dollars using the Medical Care Component of the Consumer Price Index.
2.5 Healthcare Cost Adjustments: ICER-Adjusted and ICER-Adherence-Adjusted Costs
As insurance claims may not always or consistently capture pharmacy rebates, patient assistance programs, and commissions to wholesalers, healthcare cost comparison can be biased if one drug has a higher discount factor than the other. To obtain adjusted all-cause and psoriasis-related costs, published ICER discount factors (based on net price divided by wholesale acquisition cost) were applied to biologics specific for psoriasis to adjust pharmacy costs (i.e., drug costs × [1-ICER discount factor]) [12].
The ICER discount rates of 0.44 and 0.38 were applied to IXE and SEC, respectively [12]. Adjusted all-cause and psoriasis-related costs were obtained by combining (a) ICER-adjusted costs for index drugs and other psoriasis-related biologics and (b) all-cause or psoriasis-related healthcare costs after excluding psoriasis-specific biologics costs. Sensitivity analyses were performed by varying the index drug discount rates by ± 5% to estimate mean cost differences in ICER-adjusted all-cause costs and psoriasis-related costs.
Drug costs can be impacted by treatment adherence as higher adherence results in more consumption of medication. Adjustment by adherence was performed (by dividing ICER-adjusted index drug costs by treatment adherence for each cohort) to obtain ICER-adherence-adjusted index drug costs. The adjusted costs represent the index drug costs when patients are fully adherent to treatment over 18 months. Adherence was measured as the proportion of days covered and was defined as the number of days with medication on hand during the follow-up period for each cohort divided by 730. When two prescriptions overlapped, the start date of the second prescription was adjusted to the date after the end of the prior prescription. Days’ supply from the last claim beyond the end of follow-up was truncated. Quarterly ICER-adjusted all-cause costs, psoriasis-related costs, and index-drug costs during the follow-up period were also reported.
2.6 Discrete Monthly Costs and Comorbidity-Related Costs
Unadjusted and ICER-adjusted all-cause costs, psoriasis-related costs, index drug costs, and comorbidity-related costs incurred in months 4–6 and 1–3 before the index and at each quarter from months 1 to 18 after the index were reported. Pre- and post-period cost differences and changes in the cost of related comorbidities between IXE and SEC users were evaluated. These cost outcomes would shed light on whether the biologic treatments led to reduced comorbidity-related costs, hence, a cost offset of the high drug costs. Comorbid conditions are listed in the “Covariates” section below. The approach used to capture comorbidity-related costs was similar to that used for identifying psoriasis-related costs.
2.7 Covariates
Demographic characteristics were measured at the index date and included the following variables: age, sex, payer, health plan type, and geographic region. Clinical characteristics were measured in the pre-period and included Deyo–Charlson Comorbidity Index and any comorbid diseases (anxiety, coronary heart disease, depression, diabetes mellitus, hyperlipidemia, hypertension, obesity, other autoimmune disorders, osteoarthritis, and sleep apnea). Psoriasis-related medication use in the pre-period, such as systemic agents/targeted oral therapies (apremilast, acitretin, systemic steroids, cyclosporine, methotrexate, azathioprine, hydroxyurea, isotretinoin, leflunomide, methoxsalen, mycophenolate mofetil, sulfasalazine, or thioguanine), topical treatments, and phototherapy were also included. Other covariates were pre-period psoriasis-related costs and comorbidity-related costs.
Similarly, to estimate the adjusted comorbidity-related costs, the following covariates were included in the multivariable logistic regression model: demographic characteristics (age, sex, payer, health plan type, and geographic region), pre-period Deyo–Charlson Comorbidity Index, psoriasis-related medication use in the pre-period, such as systemic agents/targeted oral therapies (listed above), topical treatments, phototherapy, and pre-period psoriasis- and comorbidity-related costs.
2.8 Statistical Analyses
Descriptive statistics were reported for IXE versus SEC; categorical variables were presented as percentages and continuous variables were presented as means and standard deviations. The MarketScan Research Databases include only fully adjudicated claims, and no patients were excluded because of missing data. To address potential cohort imbalances, inverse probability of treatment weighting was employed using a logistic regression model with IXE versus SEC as a dependent variable [13]. All the demographic and clinical variables listed in the above section were included as covariates along with pre-period psoriasis-related costs. The propensity score was defined as the probability of being treated by IXE. With p = estimated propensity score, the weights were defined as 1/p for IXE users and 1/(1 − p) for SEC users. Unweighted and weighted results are presented for pre-period patient characteristics. Cohort balances were evaluated by standardized difference (Std Diff) and a Std Diff of ≤ 10 indicates a good balance. Except for the difference between the change in pre- and post-period costs of related comorbidities, all cost data presented in this study were weighted via inverse probability of treatment weighting. Statistical tests of significance for comparison of weighted values were performed by weighted t tests for continuous variables and weighted Chi-square tests for binary/categorical variables. The a priori p value of < 0.05 was considered statistically significant.
A two-part model was used to estimate the adjusted comorbidity-related costs. First, the association between index treatment and any costs was estimated using a weighted multivariable logistic regression model. Second, the association between index treatment and follow-up period comorbidity-related costs were estimated using a Gamma-family generalized linear model with a log link. Predicted costs were estimated for each index drug using the recycled predictions method. Demographic variables, pre-period psoriasis treatment (psoriasis systemic agents/targeted oral therapies, topical agents, and phototherapy), log pre-period psoriasis-related costs, and pre-period comorbidity-related costs were included as covariates. Descriptive data were analyzed using WPS Analytics version 4.02 (World Programming, Romsey, UK). Inverse probability of treatment weighting and multivariable analyses were conducted using R version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria).
3 Results
3.1 Demographics and Clinical Characteristics
A total of 1191 patients (IXE users, n = 411; SEC users, n = 780) were included in the study (Fig. 1). Demographic and clinical characteristics are summarized in Table 1. Before weighting, the mean age of patients in the IXE and SEC groups was 48.8 and 48.5 years, respectively. Of all patients, 56.9 and 52.9% were male in the IXE and SEC groups, respectively. The most common comorbidities in IXE and SEC users were hypertension (26.0 vs 28.2%, Std Diff 4.9), hyperlipidemia (22.1 vs 21.8%, Std Diff 0.8), and obesity (19.7 vs 18.3%, Std Diff 3.5). At baseline, before weighting, all-cause ($4695 vs $4718, Std Diff 0.7) and psoriasis-related healthcare costs ($3895 vs $3810, Std Diff 4.3) were comparable between the two groups. After weighting, all the baseline demographic and clinical characteristics, except for the health plan type, were balanced between IXE and SEC groups.
3.2 Healthcare Utilization
After weighting, all-cause inpatient admissions were similar between IXE (9.5%) and SEC users (10.3%, p = 0.682) during the 18-month follow-up period (Table 2). Outpatient visits (emergency room visits, outpatient office visits, and other outpatient services) were comparable between IXE and SEC users. The same was observed for psoriasis-related outpatient services.
3.3 Unadjusted Healthcare Costs
The mean ± standard deviation PPPM all-cause healthcare costs (after weighting) during the 18-month follow-up period were higher in IXE users ($6670 ± $2910) than in SEC users ($6239 ± $3903; p = 0.049). Similarly, psoriasis-related costs and index drug costs were higher in IXE users ($5609 ± $2009; p < 0.001 and $4688 ± $1994, respectively; p < 0.001) than in SEC users ($5095 ± $2291 and $3853 ± $1977, respectively; Table 3). For IXE and SEC users, outpatient pharmacy costs comprised 87.1 and 84.5% of all-cause costs and 98.6 and 98.2% of psoriasis-related costs, respectively.
3.4 ICER-Adjusted Costs
After ICER adjustment, mean PPPM all-cause costs (IXE, $4363 ± $2576; SEC, $4398 ± $3517; p = 0.861) and psoriasis-related costs ($3302 ± $1264 vs $3253 ± $1504; p = 0.576) were comparable between IXE and SEC users (Fig. 2a). Sensitivity analyses showed no significant differences in mean all-cause ICER-adjusted costs between IXE and SEC users after varying the ICER discount factors by ± 5% (Electronic Supplementary Material).
a Mean all-cause and psoriasis (PsO)-related healthcare costs per patient per month (PPPM) before and after Institute for Clinical and Economic Review (ICER) adjustments; b ICER- and adherence-adjusted index drug costs. ICER Institute for Clinical and Economic Review, PPPM per patient per month, PsO psoriasis, USD US dollars
The ICER-adjusted mean PPPM index drug costs were higher in IXE users ($2626 ± $1117) than in SEC users ($2389 ± $1225; p = 0.001, Fig. 2b). Mean adherence (proportion of days covered) during follow-up in IXE and SEC users was 0.65 and 0.61, respectively (p = 0.033). After applying ICER and adherence adjustments, mean PPPM index drug costs were similar between IXE and SEC users ($4056 vs $3943, p = 0.339, Fig. 2b).
3.5 Costs by Discrete Months
The discrete monthly cost trend showed that the ICER-adjusted mean all-cause healthcare costs, psoriasis-related costs, and index drug costs were substantially reduced after the first 3 months for both IXE and SEC users (Fig. 3).
3.6 Pre- and Post-period Comorbidity-Related Costs
Post-period comorbidity-related costs (unweighted) accounted for 5–7% of total all-cause healthcare costs in IXE and SEC users. The unweighted pre-period ($321 ± $934) and post-period ($333 ± $752) differences in all comorbidity-related costs were not statistically significant in IXE users ($12, p = 0.789), whereas significant differences were observed in SEC users ($67, p = 0.036). The difference in pre- and post-period change in comorbidity-related costs of individual treatment between IXE and SEC was − $55 (for all conditions combined). After multivariable adjustment, no significant differences were observed in post-period weighted comorbidity-related costs between IXE and SEC users ($442 and $466; difference: $24; p = 0.770).
4 Discussion
These real-world administrative claims analyses compared healthcare costs in biologic-experienced patients with psoriasis who were treated with IXE or SEC over 18 months. The findings suggest that although the unadjusted all-cause and psoriasis-related costs were higher in IXE users than in SEC users, these costs were similar after adjusting for payer discounts. Pharmacy rebates, patient assistance programs, and commissions to wholesale are typically not captured in insurance payments. In addition, the specifics of drug discounts are usually confidential, which makes it challenging to understand the actual healthcare costs. The discount factors published by the ICER provided a viable approach to address this issue and evaluate the real-world costs of psoriasis treatment. In this study, sensitivity analyses were performed by varying the IXE and SEC discount factors by ± 5%. Sensitivity analysis results corroborated with the main analysis that the ICER-adjusted all-cause and psoriasis-related costs were comparable between IXE and SEC users.
At the 1-year follow-up, our previous study reported the unadjusted PPPM all-cause costs ($7313 vs $6477), psoriasis-related costs ($6303 vs $5437), and index drug costs ($5613 vs $4626) in patients initiating IXE or SEC [10]. These monthly costs were higher than those in the current study. Another study reported (average of 7.5 months follow-up period) higher unadjusted PPPM all-cause costs ($8560) and psoriasis-related costs ($7792) following IXE initiation in a sub-group of biologic-experienced patients [14] when compared with those in the current study (all cause: $6670; psoriasis related: $5609). However, in our study, these costs were comparable for IXE (all cause: $4363, psoriasis related: $3302) and SEC users (all cause: $4398, psoriasis related: $3253) after applying ICER discounts. Both IXE and SEC have an induction period that requires a higher dosage resulting in higher daily costs than the maintenance period. A longer follow-up period, hence, a longer maintenance therapy period, as in the current study, may explain the lower monthly costs. The higher ICER-adjusted healthcare and index drug costs for IXE and SEC users observed in the first quarter of the follow-up period could also be attributed to the higher number of induction doses required during IXE or SEC initiation. However, the costs dropped substantially after the first quarter and did not fluctuate between the IXE and the SEC users. For index drugs, the mean unadjusted costs were higher for IXE when compared with SEC but were similar after adjusting for payer discounts and treatment adherence.
The ICER report estimated first-year costs to be $51,374 for IXE and $49,624 for SEC when patients were fully adherent and received a standard price discount [12]. In this study, the estimated adjusted costs over 18 months were $73,540 and $71,505 for IXE and SEC users, respectively, among biologic-experienced patients.
The current study reported the costs of IXE and SEC in biologic-experienced patients with psoriasis. Biologics carry a substantial cost burden. In general, some patients treated with biologics do not respond to the treatment (primary failure), while others who respond initially may lose response over time (secondary failure) [15]. As a result, in clinical practice, switching to alternate biologics and dose escalation are used in subgroups of patients as a measure to improve efficacy and manage increasing dose tolerance issues over time [15, 16]. Although this is well tolerated in most of the patients, failing a prior biologic and switching to alternate biologics potentially increase costs owing to an increased dosing frequency during the induction period and therefore, higher costs for the payers [17].
The major drivers for all-cause and psoriasis-related HCRU in both the groups were outpatient services and pharmacy. This conforms with the results of another study in which HCRU and cost in biologic-treated patients with moderate-to-severe psoriasis were primarily driven by higher pharmacy costs and more outpatient encounters [18]. Additionally, patients with psoriasis have been reported to have a greater number of comorbidities leading to higher HCRU and costs [18].
A recent network meta-analysis reported that IXE was the most cost-effective biologic in the USA while targeting complete resolution, as measured using the Psoriasis Area and Severity Index 100 in patients with psoriasis [19]. Costs of IXE and SEC were comparable after adjusting for ICER discounts and treatment adherence, which is supported by the current data. Together, these findings support a cost profile for IXE comparable to that of SEC in the routine care of biologic-experienced patients with psoriasis.
A few limitations should be considered when interpreting the data from this study. Because of data coding limitations, data entry errors, or inaccurate codes, there could be misclassifications or errors potentially affecting study outcomes. Prior biologic exposure was based on a 6-month pre-period and therefore, may have missed patients who were treated prior to the index date. The Early View Database was used to capture the most recent utilization of study drugs. Although the Early View Database contains fully adjudicated claims, the medical component of care may not have been complete, resulting in an underestimation of healthcare costs. Inverse probability of treatment weighting and multivariable modeling were employed to address cohort imbalances. The unobservable imbalances that remained can impact the findings from this study. The ICER discount rates published in 2018 were used for the entire study period. As this analysis focused on patient populations with commercial and Medicare supplemental insurance, findings may not be generalizable to other insured or uninsured US or international patient populations.
5 Conclusions
This retrospective analysis showed that after applying ICER adjustments, all-cause and psoriasis-related costs were comparable over an 18-month follow-up period between IXE and SEC users among biologic-experienced patients. In addition, psoriasis-related costs of IXE and SEC were similar after considering payer discounts and treatment adherence. These results may be beneficial to payers in making informed decisions on coverage and formulary placements on these two biologics. The results also provide important real-world evidence to aid clinicians in making decisions regarding biologic treatment for patients with psoriasis who are previously treated with biologics.
References
Boehncke W-H, Schön MP. Psoriasis. Lancet. 2015;386(9997):983–94.
Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. 2014;70(3):512–6.
Brezinski EA, Dhillon JS, Armstrong AW. Economic burden of psoriasis in the United States: a systematic review. JAMA Dermatol. 2015;151(6):651–8.
Kimball AB, et al. The psychosocial burden of psoriasis. Am J Clin Dermatol. 2005;6(6):383–92.
Bagel J, et al. Dose escalation and associated costs in biologic treatment of psoriasis based on real-world data. J Med Econ. 2021;24(1):782–91.
Feldman SR, et al. Economic and comorbidity burden among patients with moderate-to-severe psoriasis. J Manag Care Spec Pharm. 2015;21(10):874–88.
Shahwan KT, Kimball AB. Managing the dose escalation of biologics in an era of cost containment: the need for a rational strategy. Int J Womens Dermatol. 2016;2(4):151–3.
Griffiths CE, et al. Comparison of ixekizumab with etanercept or placebo in moderate-to-severe psoriasis (UNCOVER-2 and UNCOVER-3): results from two phase 3 randomised trials. Lancet. 2015;386(9993):541–51.
Wang T-S, et al. Secukinumab in psoriasis patients with prior ustekinumab treatment: results of a single-center experience. Dermatol Sin. 2017;35(1):25–9.
Blauvelt A, et al. Comparison of health care costs among patients with psoriasis initiating ixekizumab, secukinumab, or adalimumab. J Manag Care Spec Pharm. 2019;25(12):1366–76.
Leigh Hansen. IBM MarketScan Research Databases for life sciences researchers. April 2018. https://www.ibm.com/downloads/cas/0NKLE57Y. Accessed 15 May 2021.
Reiner Banken, Foluso Agboola, Katherine Fazioli, et al. Institute for Clinical and Economic Review. Targeted immunomodulators for the treatment of moderate-to-severe plaque psoriasis: effectiveness and value. June 12, 2018. https://icer.org/wp-content/uploads/2020/10/ICER_Psoriasis_Update_Evidence_Report_061218.pdf. Accessed 15 May 2021.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424.
Murage MJ, et al. Ixekizumab treatment patterns and healthcare utilization and costs for patients with psoriasis. J Dermatol Treat. 2021;32(1):56–63.
Feldman SR, et al. Patterns of medication utilization and costs associated with the use of etanercept, adalimumab, and ustekinumab in the management of moderate-to-severe psoriasis. J Manag Care Spec Pharm. 2015;21(3):201–9.
Brezinski EA, Armstrong AW. Off-label biologic regimens in psoriasis: a systematic review of efficacy and safety of dose escalation, reduction, and interrupted biologic therapy. PLoS ONE. 2012;7(4): e33486.
Bewley A, et al. Dose increase beyond labelled dose of biologics is associated with incremental pharmacy costs: results from a real-world study in the UK. J Dermatol Treat. 2019;30(4):376–82.
Murage MJ, et al. Healthcare resource utilization and costs among psoriasis patients treated with biologics, overall and by disease severity. J Med Econ. 2018;21(8):745–54.
Al Sawah S, et al. Cost per additional responder for ixekizumab and other FDA-approved biologics in moderate-to-severe plaque psoriasis. J Med Econ. 2017;20(12):1224–30.
Acknowledgements
The authors acknowledge Bilal Atiya (Eli Lilly and Company, Indianapolis, IN, USA) for his contribution to study implementation. The medical writing support was provided by Priyanka Bannikoppa, PhD and Amit Koushik, MS of Eli Lilly and Company.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Eli Lilly and Company.
Conflicts of interest
Andrew Blauvelt has served as a scientific adviser and/or clinical study investigator for AbbVie, Abcentra, Aligos, Almirall, Amgen, Arcutis, Arena, Aslan, Athenex, Boehringer Ingelheim, Bristol-Myers Squibb, Dermavant, EcoR1, Eli Lilly and Company, Evommune, Forte, Galderma, Incyte, Janssen, Landos, Leo, Novartis, Pfizer, Rapt, Regeneron, Sanofi Genzyme, Sun Pharma, UCB Pharma, and Vibliome. Nianwen Shi, Carolyn R. Lew, and Nicole M. Zimmerman are employees of IBM Watson Health who were compensated by Eli Lilly and Company for conducting this research. Najwa Somani, Scott A. Kern, Russel Burge, Terri Ridenour, Baojin Zhu, and Mwangi Murage are full-time employees and stockholders of Eli Lilly and Company.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Data for these analyses are derived from the IBM MarketScan® Research Databases. The data are not publicly available because of data use agreements and can be accessed by purchasing a license through IBM Watson Health. Interested individuals may visit https://www.ibm.com/products/marketscan-research-databases for more information on accessing the MarketScan® Research Databases.
Code availability
Not applicable.
Author contributions
NS had full access to all the data in the study and was responsible for the integrity of the data and the accuracy of data analysis. AB, NS, RB, BZ, and MJM were involved in the conception and design of the study. AB, NS, RB, CRL, NMZ, SAK, BZ, and MJM acquired, analyzed, or interpreted the data. AB, NS, RB, CRL, NMZ, BZ, SAK, and MJM contributed towards the critical revision of the manuscript for important intellectual content. NMZ conducted the statistical analysis. The manuscript was drafted under the supervision of MJM and NS. All authors contributed to the data analysis, drafting, and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Blauvelt, A., Shi, N., Somani, N. et al. Comparison of Real-World Costs, Healthcare Resource Utilization, and Comorbidity-Related Costs Between Ixekizumab and Secukinumab Among Biologic-Experienced Patients with Psoriasis Over 18 Months in the USA. Clin Drug Investig 43, 185–196 (2023). https://doi.org/10.1007/s40261-022-01240-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-022-01240-9