Abstract
Background
Given the broad scope of the spillover effects of illness, it is important to characterize the variability in these outcomes to identify relationship types in which secondary impacts of illness are particularly important to include in health economic evaluations.
Purpose
To examine heterogeneity in spillover effects of chronic conditions on family members by type of familial relationship with patient.
Methods
Adults (aged ≥18 years) and adolescents (aged 13–17 years) who had a parent, spouse, or child in their household with a chronic condition (Alzheimer’s disease/dementia, arthritis, cancer, or depression) were recruited from a US national panel to participate in an on-line survey. Respondents were asked to rate the spillover effect of their family member’s illness on their own health on a 0–100 scale, with lower scores indicating greater spillover. Regression analysis was used to evaluate the association between rating scale scores and relationship with an ill family member (ill parent, child, or spouse) for each illness separately, controlling for caregiving responsibility and the health status of the ill family member.
Results
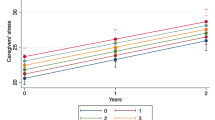
1,267 adults and 102 adolescents met inclusion criteria. In adjusted analyses, having a sick child was significantly (p < 0.05) associated with lower rating scale scores compared with having a spouse with the same condition (cancer: −24.2; depression −9.7). Having a non-elderly or elderly adult parent with a condition, compared with a spouse, was significantly associated with lower rating scale scores for arthritis (−3.8) and depression (−5.3), but not for Alzheimer’s disease/dementia or cancer.
Conclusions
The impact of illness on family members, measured with a rating scale, varies by relationship type for certain illnesses. Having a child with cancer, a parent with arthritis, or either with depression, is significantly associated with greater spillover, compared with having a spouse with one of these conditions.


Similar content being viewed by others
References
Wittenberg E, Prosser LA. Disutility of illness for caregivers and families: a systematic review of the literature. Pharmacoeconomics. 2013;31(6):489–500.
Bobinac A, van Exel NJ, Rutten FF, Brouwer WB. Caring for and caring about: disentangling the caregiver effect and the family effect. J Health Econ. 2010;29(4):549–56.
Bobinac A, van Exel NJ, Rutten FF, Brouwer WB. Health effects in significant others: separating family and care-giving effects. Med Decis Mak. 2011;31(2):292–8.
Brouwer WB. Too important to ignore: informal caregivers and other significant others. Pharmacoeconomics. 2006;24(1):39–41.
Brouwer WBF. Incorporating caregiver and family effects in economic evaluations of child health. In: Ungar WJ, editor. Economic evaluation in child health. Oxford: Oxford University Press; 2010. p. 55–76.
Wittenberg E, Ritter GA, Prosser LA. Evidence of spillover of illness among household members: EQ-5D scores from a US sample. Med Decis Mak. 2013;33(2):235–43.
Basu A, Dale W, Elstein A, Meltzer D. A time tradeoff method for eliciting partner’s quality of life due to patient’s health states in prostate cancer. Med Decis Mak. 2010;30(3):355–65.
Basu A, Meltzer D. Implications of spillover effects within the family for medical cost-effectiveness analysis. J Health Econ. 2005;24(4):751–73.
Poley MJ, Brouwer WBF, van Exel NJA, Tibboel D. Assessing health-related quality-of-life changes in informal caregivers: an evaluation in parents of children with major congenital anomalies. Qual Life Res. 2012;21(5):849–61.
Brouwer WBF, van Exel NJ, Van De Berg B, Dinant HJ, Koopmanschap MA, van den Bos GAM. Burden of caregiving: evidence of objective burden, subjective burden, and quality of life impacts on informal caregivers of patients with rheumatoid arthritis. Arthritis Rheum. 2004;51(4):570–7.
Neumann PJ, Kuntz KM, Leon J, Araki SS, Hermann RC, Hsu MA, et al. Health utilities in Alzheimer’s disease: a cross-sectional study of patients and caregivers. Med Care. 1999;37(1):27–32.
Davidson T, Krevers B, Levin LA. In pursuit of QALY weights for relatives: empirical estimates in relatives caring for older people. Eur J Health Econ. 2008;9(3):285–92.
Argyriou AA, Karanasios P, Ifanti AA, Iconomou G, Assimakopoulos K, Makridou A, et al. Quality of life and emotional burden of primary caregivers: a case-control study of multiple sclerosis patients in Greece. Qual Life Res. 2011;20(10):1663–8.
Brisson M, Senecal M, Drolet M, Mansi JA. Health-related quality of life lost to rotavirus-associated gastroenteritis in children and their parents: a Canadian prospective study. Pediatr Infect Dis J. 2010;29(1):73–5.
Dixon S, Walker M, Salek S. Incorporating carer effects into economic evaluation. Pharmacoeconomics. 2006;24(1):43–53.
Kuhlthau K, Kahn R, Hill KS, Gnanasekaran S, Ettner SL. The well-being of parental caregivers of children with activity limitations. Matern Child Health J. 2010;14(2):155–63.
Mohide EA, Torrance GW, Streiner DL, Pringle DM, Gilbert R. Measuring the wellbeing of family caregivers using the time trade-off technique. J Clin Epidemiol. 1988;41(5):475–82.
Serrano-Aguilar PG, Lopez-Bastida J, Yanes-Lopez V. Impact on health-related quality of life and perceived burden of informal caregivers of individuals with Alzheimer’s disease. Neuroepidemiology. 2006;27(3):136–42.
Tilford JM, Grosse SD, Robbins JM, Pyne JM, Cleves MA, Hobbs CA. Health state preference scores of children with spina bifida and their caregivers. Qual Life Res. 2005;14(4):1087–98.
van Exel NJ, Koopmanschap MA, van den Berg B, Brouwer WB, van den Bos GA. Burden of informal caregiving for stroke patients: identification of caregivers at risk of adverse health effects. Cerebrovasc Dis. 2005;19(1):11–7.
Lieberman MA, Fisher L. The impact of chronic illness on the health and well-being of family members. Gerontologist. 1995;35(1):94–102.
Bell CM, Araki SS, Neumann PJ. The association between caregiver burden and caregiver health-related quality of life in Alzheimer disease. Alzheimer Dis Assoc Disord. 2001;15(3):129–36.
KnowledgePanel® Design Summary 2012 [cited 2013 August 27]. http://www.knowledgenetworks.com/knpanel/docs/knowledgePanel(R)-design-summary-description.pdf.
Respondent Incentives for Knowledge Panel®. 2009 [cited 2013 July 1]. http://www.knowledgenetworks.com/ganp/irbsupport/docs/KNIRBDoc-Section4-RespondentIncentives.doc.
Efron B. Better bootstrap confidence-intervals. J Am Stat Assoc. 1987;82(397):171–85.
Akaike H. New look at statistical-model identification. IEEE Trans Automat Contr. 1974;19(6):716–23.
Gold MR. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996.
Robinson A, Dolan P, Williams A. Valuing health status using VAS and TTO: what lies behind the numbers? Soc Sci Med. 1997;45(8):1289–97.
Glick H. Assessing quality-adjusted life years: economic evaluation in clinical trials. Oxford: Oxford University Press; 2007. p. 59–87.
Wittenberg E, Saada A, Prosser LA. How illness affects family members: a qualitative interview survey. Patient. 2013;6(4):257–68.
Eisenberg D, Freed GL, Davis MM, Singer D, Prosser LA. Valuing health at different ages: evidence from a nationally representative survey in the US. Appl Health Econ Health Policy. 2011;9(3):149–56.
Lavelle TA, Meltzer MI, Gebremariam A, Lamarand K, Fiore AE, Prosser LA. Community-based values for 2009 pandemic influenza A H1N1 illnesses and vaccination-related adverse events. PLoS One. 2011;6(12):e27777.
Pullenayegum EM, Tarride JE, Xie F, O’Reilly D. Calculating utility decrements associated with an adverse event: marginal Tobit and CLAD coefficients should be used with caution. Med Decis Mak. 2011;31(6):790–9.
Pullenayegum EM, Tarride JE, Xie F, Goeree R, Gerstein HC, O’Reilly D. Analysis of health utility data when some subjects attain the upper bound of 1: are Tobit and CLAD models appropriate? Value Health. 2010;13(4):487–94.
Brazier J, Ratcliffe J, Salomon JA, Tsuchiya A. Valuing health: measuring and valuing health benefits for economic evaluation. Oxford: Oxford University Press; 2007. p. 83–138.
Acknowledgments
The authors thank Acham Gebremariam for his programming assistance.
Source of financial support
Funding for this study was provided by the National Institute of Nursing Research (7-R01-NR-011880-03).
Author Contributions
Tara A. Lavelle: Dr. Lavelle contributed to the conceptualization and design of the study, carried out all data analyses, drafted the manuscript, and approved the final manuscript as submitted. Dr. Lavelle takes responsibility for the overall content of the manuscript.
Eve Wittenberg: Dr. Wittenberg contributed to the conceptualization and design of the study, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Kara Lamarard: Ms. Lamarand coordinated data collection, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Lisa A. Prosser: Dr. Prosser contributed to the conceptualization and design of the study, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Conflict of interest
Tara A. Lavelle: Dr. Lavelle reports no conflict of interest.
Eve Wittenberg: Dr. Wittenberg reports no conflict of interest.
Kara Lamarard: Ms. Lamarand reports no conflict of interest.
Lisa A. Prosser: Dr. Prosser reports no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lavelle, T.A., Wittenberg, E., Lamarand, K. et al. Variation in the Spillover Effects of Illness on Parents, Spouses, and Children of the Chronically Ill. Appl Health Econ Health Policy 12, 117–124 (2014). https://doi.org/10.1007/s40258-014-0079-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-014-0079-8