Abstract
Background
Proper synthesis of existing epidemiologic studies on diabetes in Iran can guide future research efforts. We aimed to conduct a comprehensive scoping review on all research articles that investigated any aspect of diabetes epidemiology in Iran during 2015–2019.
Methods
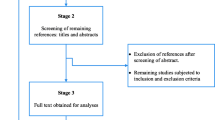
This work was conducted as a part of the Iran Diabetes Research Roadmap and completed under Arksey and O'Malley’s framework for scoping reviews. The Scopus and PubMed databases were searched on Feb 15th, 2020. Eligible document types on diabetes epidemiology in the Iranian population, in Persian or English, that published during the 2015–2019 period underwent eligibility assessment. A total of 315 relevant articles were included and further analysis was performed on the original studies (n = 268). Through classifying them into six domains: Diabetes incidence; the prevalence of diabetes and associated factors; the incidence/prevalence of complications/comorbid conditions; mortality/survival; burden; and prediction modeling.
Results
In total, 64 (20.3%) papers were published in Q1 journals, and 40 (12.6%) were international collaborations. No clear annual trend was present in the number of published primary or secondary articles, the portion of papers published in Q1 journals, international collaborations or relative domain proportions. Few review articles were found on prediction modeling, mortality or burden (excluding global studies).
Conclusions
Our findings show a minor portion of works on diabetic epidemiology in Iran meets the quality standards of Q1 journals. Researchers have neglected some critical subjects and have occasionally fallen for common pitfalls of epidemiologic research. In particular, adhering to established guidelines can help authors implement rigorous methods to develop, validate, and deploy practical clinical prediction models. Researchers should prioritize investigating longitudinally collected data that aid in measuring disease incidence and enable casual inference.





Similar content being viewed by others
References
Nathan DM. Long-term complications of diabetes mellitus. N Engl J Med. 1993;328(23):1676–85.
Saeedi P, Salpea P, Karuranga S, Petersohn I, Malanda B, Gregg EW, et al. Mortality attributable to diabetes in 20–79 years old adults, 2019 estimates: Results from the International Diabetes Federation Diabetes Atlas. Diabetes research and clinical practice. 2020: 108086.
Emerging Risk Factors Collaboration, Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375(9733):2215–22.
Bourne RR, Stevens GA, White RA, Smith JL, Flaxman SR, Price H, et al. Causes of vision loss worldwide, 1990–2010: a systematic analysis. Lancet Glob Health. 2013;1(6):e339–49.
Saran R, Li Y, Robinson B, Abbott KC, Agodoa LY, Ayanian J, et al . US Renal Data System 2015 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am J Kidney Dis. 2016;67(3 Suppl 1): Svii, S1-305.
Djalalinia S, Modirian M, Sheidaei A, Yoosefi M, Zokaiee H, Damirchilu B, et al. Protocol Design for Large-Scale Cross-Sectional Studies of Surveillance of Risk Factors of Non-Communicable Diseases in Iran: STEPs 2016. Arch Iran Med. 2017;20(9):608–16.
Aguiree F, Brown A, Cho N, Dahlquist G, Aguiree B, Cho D, et al. Whiting (2013) IDF Diabetes Atlas. IDF Diabetes Atlas, 6th Edition, International Diabetes Federation, Basel.74–90.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–1530.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Süt N. Study designs in medicine. Balkan Med J. 2014;31(4):273.
Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services, 2020.
Zand A, Ibrahim K, Patham B. Prediabetes: Why Should We Care? Methodist Debakey Cardiovasc J. 2018;14(4):289–97.
Kharroubi AT, Darwish HM. Diabetes mellitus: The epidemic of the century. World J Diabetes. 2015;6(6):850.
Kriegsman DM, Penninx BW, Van Eijk JTM, Boeke AJP, Deeg DJ. Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly: a study on the accuracy of patients’ self-reports and on determinants of inaccuracy. J Clin Epidemiol. 1996;49(12):1407–17.
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract. 2019;157: 107843.
Goldman N, Lin I-F, Weinstein M, Lin Y-H. Evaluating the quality of self-reports of hypertension and diabetes. J Clin Epidemiol. 2003;56(2):148–54.
Spronk I, Korevaar JC, Poos R, Davids R, Hilderink H, Schellevis FG, et al. Calculating incidence rates and prevalence proportions: not as simple as it seems. BMC Public Health. 2019;19(1):1–9.
Song JW, Chung KC. Observational studies: cohort and case-control studies. Plast Reconstr Surg. 2010;126(6):2234.
Rothman KJ, Greenland S. Causation and causal inference in epidemiology. Am J Public Health. 2005;95(Suppl 1):S144–50.
Schooling CM, Jones HE. Clarifying questions about “risk factors”: predictors versus explanation. Emerg Themes Epidemiol. 2018;15(1):1–6.
Craun GF, Calderon RL. How to interpret epidemiological associations. Nutrients in Drinking Water. 2005;108:108–15.
Abbasi SH, Sundin Ö, Jalali A, Soares J, Macassa G. Ethnic differences in the risk factors and severity of coronary artery disease: a patient-based study in Iran. J Racial Ethn Health Disparities. 2018;5(3):623–31.
Spanakis EK, Golden SH. Race/ethnic difference in diabetes and diabetic complications. Curr DiabRep. 2013;13(6):814–23.
Jo C. Cost-of-illness studies: concepts, scopes, and methods. Clin Mol Hepatol. 2014;20(4):327.
Mauskopf JA, Paul JE, Grant DM, Stergachis A. The role of cost—consequence analysis in healthcare decision—making. Pharmacoeconomics. 1998;13(3):277–88.
Abbasi A, Peelen LM, Corpeleijn E, van der Schouw YT, Stolk RP, Spijkerman AM, et al. Prediction models for risk of developing type 2 diabetes: systematic literature search and independent external validation study. BMJ. 2012;345:e5900.
Hemingway H, Croft P, Perel P, Hayden JA, Abrams K, Timmis A, et al. Prognosis research strategy (PROGRESS) 1: a framework for researching clinical outcomes. BMJ. 2013;346:e5595.
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD) the TRIPOD statement. Circulation. 2015;131(2):211–9.
Steyerberg EW, Pencina MJ, Lingsma HF, Kattan MW, Vickers AJ, Van Calster B. Assessing the incremental value of diagnostic and prognostic markers: a review and illustration. Eur J Clin Invest. 2012;42(2):216–28.
Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, et al. Assessing the performance of prediction models: a framework for some traditional and novel measures. Epidemiology. 2010;21(1):128.
Steyerberg EW, Harrell FE Jr. Prediction models need appropriate internal, internal-external, and external validation. J Clin Epidemiol. 2016;69:245.
Bleeker S, Moll H, Steyerberg E, Donders A, Derksen-Lubsen G, Grobbee D, et al. External validation is necessary in prediction research: A clinical example. J Clin Epidemiol. 2003;56(9):826–32.
Van Calster B, McLernon DJ, Van Smeden M, Wynants L, Steyerberg EW. Calibration: the Achilles heel of predictive analytics. BMC Med. 2019;17(1):1–7.
Moons KG, Kengne AP, Woodward M, Royston P, Vergouwe Y, Altman DG, et al. Risk prediction models: I. Development, internal validation, and assessing the incremental value of a new (bio) marker. Heart. 2012;98(9):683–90.
Steyerberg, EW. Selection of main effects. In: Steyerberg, EW, editors. Clinical Prediction Models: A Practical Approach to Development, Validation, and Updating. Springer International Publishing; 2019. p. 207–225.
Moons KG, Kengne AP, Grobbee DE, Royston P, Vergouwe Y, Altman DG, et al. Risk prediction models: II. External validation, model updating, and impact assessment. Heart. 2012;98(9):691–8.
Shafiee G, Nasli-Esfahani E, Bandarian F, Peimani M, Yazdizadeh B, Razi F, et al. Iran Diabetes Research Roadmap (IDRR): the study protocol. J Diabetes Metab Disord. 2016;15:58.
Esmaeili S, Bandarian F, Razi F, Adibi H, Jalili A, Arjmand B, et al. An overview of diabetes research achievements during a quarter of a century in Diabetes Research Center. J Diabetes Metab Disord. 2021;1–8.
Acknowledgements
The authers would like to express their gratitude to all the researchers and personell at the Endocrinology and Metabolism Research Institute who supported the conduct of this work.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
The research protocol and ethical conduct for Iran Diabetes Research Roadmap were approved by the Endocrinology and Metabolism Research Institute at Tehran University of Medical Sciences (Code: IR.TUMS.EMRIEC,1399.004).
a project numbered 1398–1-97–974 approved by the Endocrinology and Metabolism Research Institute, Tehran University of Medical Silences.
The Ethics Committee of Tehran University of Medical Sciences approved the present study with the approval number of IR. TUMS.EMRIREC. 1399.004.
Competing interests
None declared.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gharishvandi, F., Moheimani, H., Esmaeili, S. et al. Epidemiology of diabetes in Iran: A scoping review of studies published during 2015–2019. J Diabetes Metab Disord 21, 1913–1921 (2022). https://doi.org/10.1007/s40200-022-01094-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-022-01094-0