Abstract
Purpose
The severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) has caused substantial mortality worldwide. We investigated clinical and demographic features of COVID-19-related deaths that occurred between March 2020 and January 2022 in Regensburg, Germany.
Methods
We compared data across four consecutive time periods: March 2020 to September 2020 (period 1), October 2020 to February 2021 (period 2), March 2021 to August 2021 (period 3), and September 2021 to January 2022 (period 4).
Results
Overall, 405 deaths in relation to COVID-19 were reported. The raw case fatality ratio (CFR) was 0.92. In periods 1 to 4, the CFRs were 1.70%, 2.67%, 1.06%, and 0.36%. The age-specific CFR and mortality were highest in persons aged ≥ 80 years in period 2 while mortality in younger cases increased with time. The median age at death was 84 years and it varied slightly across periods. Around 50% of cases of death were previously hospitalized. In all time periods, the cause of death was mostly attributed to COVID-19. Over the four periods, we did not find significant changes in the distribution of sex and risk factors for severe disease. The most frequent risk factor was cardio-circulatory disease.
Conclusion
In conclusion, the CFR decreased over time, most prominently for period 4. Mortality was considerable and younger cases were increasingly at risk.
Similar content being viewed by others
Introduction
The severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) has caused hundreds of millions of known cases and millions of deaths worldwide [1]. It has impacted health systems, economies, and social interactions on a mass scale. While even mild disease or the necessity of isolation of asymptomatic cases or quarantine of contacts have caused costs, loss of work force, delayed medical treatment and social deprivation, a death due to COVID-19 is regarded as the most severe outcome [2, 3]. Thus, mortality data have been of major importance for guiding infection control measures.
Changes in viral variants leading to altered pathogenic features and transmission properties, along with evolving population immunity, have raised the question of whether characteristics of COVID-related deaths have changed over time. We, therefore, performed a retrospective observational study and investigated whether case fatality ratio (CFR) and mortality or clinical and demographic features of COVID-related deaths changed across four specific time periods between March 2020 and January 2022 in Regensburg, Germany.
Methods
Study period and population
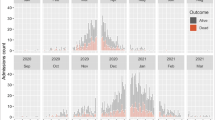
We searched the health department’s database Äsculab21 for all COVID-19-related deaths reported in Regensburg residents (city/county) between March 2020 and March 2022 according to the date of reporting to the Robert Koch Institute (RKI), Germany’s national institute of disease control and prevention. We restricted those deaths to the time period March 2020 to January 2022 by date of death (to exclude the presumed time of onset of the omicron wave [4]). We defined four time periods according to the observed monthly numbers of deaths (Fig. 1A): March to September 2020 (period 1), October 2020 to February 2021 (period 2), March to August 2021 (period 3), and September 2021 to January 2022 (period 4). The overall population of Regensburg (city and county) comprised 346,545 residents (according to [5]).
Number of deaths, incidence, case fatality ratio (CFR) and mortality. A Number of deaths by month between March, 2020, and January, 2022, and mortality per 100,000 (calculated for Regensburg population acc. to [5]). B.1.1.7, Alpha variant; B.1.617.2, Delta variant; B.1.1.529, Omicron variant, acc. to [4]. B Incidence proportion per day in the respective period (left vertical axis), mortality per day, and CFR by period (both right vertical axis)
Case definitions and characteristics of deaths
We applied the case definition of COVID-19/SARS-CoV-2 according to the RKI [6]. Deaths were defined as “death in relation to COVID-19”, including deaths that were reported to the RKI as caused by SARS-CoV-2 and deaths that were reported as caused otherwise. We assessed data on risk factors (RF), hospitalizations, and the attributed cause of death (using Äsculab21 reporting software). For period 1, we took into account additional information on RF documented only on paper.
Statistics
We calculated the raw case fatality ratio (CFR) based on all COVID-related deaths. We calculated incidence proportions and mortality on the basis of population data for Regensburg [5]. For inter-period comparisons, we calculated mortality per day because time periods varied in their duration. Case fatality ratio (CFR) and mortality were compared across periods for the following age groups: 0–59, 60–79, and ≥ 80 years. For descriptive analysis, we present absolute and relative frequencies, and 95% confidence intervals (95% CIs) as interval estimates. For statistical testing, we used a Chi-squared test for categorical variables and a Kruskal–Wallis rank-sum test for comparison of medians (level of significance p < 0.05). All analyses were performed using Microsoft Excel 2016 and Epi Info, version 7.2.5.0.
Results
We found the largest death count and a distinct mortality peak in period 2 (Fig. 1A). The four defined periods roughly correspond with the four infection waves reported for Germany so far [7]. From November 2021 onwards, we found decreasing death counts.
In the overall study period, 405 deaths in relation to COVID-19 were reported (Table 1). The overall CFR was 0.92. The median age was 84 years (range 32–103 years; 195 male [48.15%], 206 female [50.86%], 4 unknown [0.99%]). Hospitalization was reported for 212 cases (52.35%). The most prevalent risk factors were chronic cardio-circulatory disease, neurological/neuromuscular disease, and diabetes. The proportion of unknown risk factors ranged from 28.40% (cardio-circulatory disease) to 37.53% (immunodeficiency/HIV).
Absolute numbers of deaths were 28, 204, 73, and 100 for time periods 1, 2, 3, and 4. Absolute numbers of reported cases for the respective time periods were 1648, 7645, 6909, and 27,972, resulting in incidence proportions of 2.22, 14.61, 10.84, and 52.76 per 100,000 per day. The mortality per 100,000 per day was 0.04, 0.39, 0.11, and 0.19; and the CFR was 1.70%, 2.67%, 1.06%, and 0.36%, respectively (Fig. 1B).
Comparing different age groups (0–59, 60–79, and ≥ 80 years), in all time periods, we found the largest CFRs among cases aged ≥ 80 years, culminating in a CFR of approximately 21% in period 2 (Table 1). Overall, the age-specific CFR decreased in all three age groups from periods 1 through 4 (p = 0.004, p < 0.001, and p < 0.001 for 0–59, 60–79, and ≥ 80 years). COVID-19-related mortality was highest in the age group ≥ 80 years in period 2 (5.065 per 100,000 per day), which was 16-fold higher than in period 1 (Table 1). While mortality in 60–79-year-olds was sixfold higher during period 2, with a decrease in periods 3 and 4, in cases aged 0–59 years it increased steadily from period 1 to 4.
We found no significant differences in the sex distribution across time periods (p = 0.100). The median age at death varied between periods, with a tendency towards higher ages in the winter waves (median age 79, 86, 79, and 82 years; interquartile range 64–85, 80–90, 70–87, and 73–89 years for periods 1 to 4; p < 0.001). Deaths in young cases (< 50 years) were rare (3 cases) and were only observed in period 4. Hospitalizations were more common during the first period: 89.29% (95% CI 71.77–97.73%) of deaths were hospitalized compared to 45.10% (95% CI 38.14–52.20%), 38.36% (95% CI 27.21–50.48%) and 67.00% (95% CI 56.88–76.08%) in periods 2–4. Cause of death was mainly attributed to COVID-19 in all time periods. However, during period 2, 73 deaths (35.78%; 95% CI 29.21–42.78%) were attributed to a different cause.
Discussion
In our retrospective analysis of 405 consecutive COVID-related deaths over four time periods, we found the largest death counts during the second COVID-19 wave (period 2), with a maximum CFR of 2.67% and decreasing values for periods 3 and 4. The overall raw CFR was below 1% in the entire study period. While COVID-19-related mortality was highest in the age groups ≥ 80 years and 60–79 years during period 2, it is noteworthy that mortality in cases up to 59 years of age increased steadily from period 1 to 4.
Official estimates by the RKI state a CFR of 1.8% for Germany (by November, 2021 [8]), which is approximately 100% higher than in our cohort. This finding is consistent with our results from the analysis of the first wave in Regensburg and might be due to differences in the age structure and the distribution of RF [9]. It has been reported that differences in CFRs in Germany depended mainly on the age structure of the population and the confirmed infection rates [10]. Moreover, different observed CFRs across countries converge after adjusting for age [11]. In Regensburg, the old-age dependency ratio (number of persons aged 65 per 100 persons aged 14–64) is lower than the national figures: Regensburg city: 26.4, Regensburg county: 33.1, Germany: 36.9 (data for 2020) [12,13,14]. Yet, the share of persons aged ≥ 80 years in Regensburg (city and county) is only slightly lower than in Germany overall (5.8% and 7.1%, respectively) [5, 15].
We compared raw CFRs between time periods assuming constant age strata. While we found a linear decrease of the CFR from period 2 onwards, mortality increased between periods 3 and 4 by approximately 50%. At the same time, the incidence proportion per day was almost fivefold higher in period 4 than in the previous one. While we must assume significant underreporting of cases during the first wave (resulting probably in overestimating lethality based on the CFR), detection and reporting of cases was facilitated later by growing test capacities. On the other hand, immunity of the population has built up through vaccination and infection, viral tropism has changed with less lower respiratory tract involvement, and thus viral pathogenicity might have decreased [16,17,18]. However, the transmissibility of predominant variants has continuously grown [18]. This—together with higher detection rates—results in larger case numbers, especially in period 4 when variant B.1.617.2 became predominant. Vaccinations started in January 2021. A relatively full vaccination coverage of vulnerable and/or elderly people can be assumed by mid-2021, so the decrease in CFR may also be explained by the protective effect of vaccination against severe disease and death (the effectivity in this regard was stated approximately 90% during the Delta wave, acc. to [4]) [19]. Mortality rates show that old and very old people were at especially high risk of COVID-19-related death in period 2 when vaccines were not available. Comparing our data to national excess mortality data, the marked peaks in absolute numbers of deaths/mortality in periods 1 and 4 (Fig. 1) correspond well with reported excess mortality for both time periods in Germany [20].
Numbers of hospitalizations differed between periods. In period 1, 90% of cases who died were previously admitted to hospital. One reason for this finding might be that there was less experience with this new disease. For period 2, there were fewer capacities as case counts were rising. Cases tended to be even older (interquartile range IQR 80–90 years), and many died in retirement homes because they were likely not eligible or willing to be hospitalized. However, reporting hospitalizations of COVID-19 patients was not mandatory before July 2021, so information bias is likely [21].
Overall, deaths were mainly attributed to COVID-19. In comparison, a greater share of deaths was not attributed to COVID-19 in period 2. One reason for this is the higher age of the deceased in this time period. Differences between periods might also reflect uncertainty in the causal attribution of deaths, as reported previously [22].
Our analysis is limited by its retrospective nature and small sample size. Due to differences in the distribution of age and risk factors, our results may not be applicable to other geographic regions. Data were collected by telephone interviews and are therefore prone to several types of bias (selection, reporting, and interviewer bias). Data on vaccination status were incomplete and were therefore not considered for evaluation. Data on hospitalizations were dependent on reports by clinicians and could not be verified. The attribution of the cause of death to COVID-19 or an alternative cause has been an unresolved problem [22].
In conclusion, we found that between March 2020 and January 2022, mainly elderly people died in relation to COVID-19. Demographic and clinical characteristics of deaths did not change significantly over time. The CFR decreased over time, most likely owing to higher transmissibility of new variants and increasing immunity based on vaccination coverage and continuous endemic transmission. Yet, with higher contagiousness in period 4, death counts are still considerable and younger cases are at risk.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Johns Hopkins University. Coronavirus Resource Center [Internet]. [cited 2022 Jul 25]. Available from: https://coronavirus.jhu.edu/map.html
Pires SM, Redondo HG, Espenhain L, Jakobsen LS, Legarth R, Meaidi M, et al. Disability adjusted life years associated with COVID-19 in Denmark in the first year of the pandemic. BMC Public Health. 2022;22:1315.
Rubio-Tomás T, Skouroliakou M, Ntountaniotis D. Lockdown due to COVID-19 and Its consequences on diet, physical activity, lifestyle, and other aspects of daily life worldwide: a narrative review. Int J Environ Res Public Health. 2022;19:6832.
Robert Koch Institute. Wöchentlicher Lagebericht des RKI zur Coronavirus-Krankheit-2019 (COVID-19) 27.01.2022—AKTUALISIERTER STAND FÜR DEUTSCHLAND [Internet]. [cited 2022 Jul 25]. Available from: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/Wochenbericht/Wochenbericht_2022-01-27.pdf?__blob=publicationFile
Bayerisches Landesamt für Statistik—GENESIS online—Bevölkerung: Kreis, Geschlecht, Altersjahre (75)/ Altersjahre (88), Stichtag [Internet]. [cited 2022 Aug 3]. Available from: https://www.statistikdaten.bayern.de/genesis/online#astructure
Robert Koch Institute (RKI) Case definition: falldefinition Coronavirus-Krankheit-2019 (COVID-19) (SARS-CoV-2) [Internet]. Available from: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Falldefinition.pdf?__blob=publicationFile. Accessed 22 Feb 2021
Rober Koch Institute. COVID-19-Dashboard—Auswertungen basierend auf den aus den Gesundheitsämtern gemäß IfSG übermittelten Meldedaten [Internet]. [cited 2022 Jul 26]. Available from: https://experience.arcgis.com/experience/478220a4c454480e823b17327b2bf1d4
Robert Koch Innstitute. Epidemiologischer Steckbrief zu SARS-CoV-2 und COVID-19 [Internet]. [cited 2022 Jul 25]. Available from: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Steckbrief.html;jsessionid=27BEAB8F81E082F5D590513AC37E6BF9.internet112?nn=13490888#doc13776792bodyText13
Lampl BMJ, Buczovsky M, Martin G, Schmied H, Leitzmann M, Salzberger B. Clinical and epidemiological data of COVID-19 from Regensburg, Germany: a retrospective analysis of 1084 consecutive cases. Infection [Internet]. 2021 Mar 5 [cited 2021 Jul 2]; Available from: http://link.springer.com/10.1007/s15010-021-01580-2
Morwinsky S, Nitsche N, Acosta E. COVID-19 fatality in Germany: demographic determinants of variation in case-fatality rates across and within German federal states during the first and second waves. Demogr Res. 2021;22:1355–72.
Sudharsanan N, Didzun O, Bärnighausen T, Geldsetzer P. The contribution of the age distribution of cases to COVID-19 case fatality across countries: a nine-country demographic study. Ann Intern Med. 2020;173:714–20.
Bundesministerium für Arbeit und Soziales—Alternde Gesellschaft [Internet]. [cited 2022 Aug 10]. Available from: https://www.bmas.de/DE/Soziales/Rente-und-Altersvorsorge/Fakten-zur-Rente/Alternde-Gesellschaft/alternde-gesellschaft.html
Bayerisches Landesamt für Statisitk—Regionalisierte Bevölkerungsvorausberechnung für Bayern bis 2040. Demographisches Profil für die Kreisfreie Stadt Regensburg Beiträge zur Statistik Bayerns, Heft 554 Hrsg. im Januar 2022 [Internet]. [cited 2022 Aug 10]. Available from: https://www.statistik.bayern.de/mam/statistik/gebiet_bevoelkerung/demographischer_wandel/demographische_profile/09362.pdf
Bayerisches Landesamt für Statisitk—Statistik kommunal 2021. Landkreis Regensburg - Eine Auswahl wichtiger statistischer Daten [Internet]. [cited 2022 Aug 10]. Available from: https://www.statistik.bayern.de/mam/produkte/statistik_kommunal/2021/09375.pdf
DESTATIS - Statistisches Bundesamt—Bevölkerung nach Altersgruppen [Internet]. [cited 2022 Aug 11]. Available from: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/Bevoelkerungsstand/Tabellen/bevoelkerung-altersgruppen-deutschland.html
Menni C, Valdes AM, Polidori L, Antonelli M, Penamakuri S, Nogal A, et al. Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: a prospective observational study from the ZOE COVID Study. The Lancet. 2022;399:1618–24.
Lamers MM, Mykytyn AZ, Breugem TI, Groen N, Knoops K, Schipper D, et al. SARS-CoV-2 Omicron efficiently infects human airway, but not alveolar epithelium [Internet]. Microbiology. http://biorxiv.org/lookup/doi/10.1101/2022.01.19.476898. 2022 Jan [cited 2022 Jul 25].
de Souza AS, de Freitas Amorim VM, Guardia GDA, dos Santos FF, Ulrich H, Galante PAF, et al. Severe acute respiratory syndrome coronavirus 2 variants of concern: a perspective for emerging more transmissible and vaccine-resistant strains. Viruses. 2022;14:827.
Bundesministerium für Gesundheit (BMG)—impfdashboard [Internet]. Available from: https://impfdashboard.de/. [cited 2022 Jul 25].
European Mortality Monitoring (EUROMOMO) Project—graphs and maps [Internet]. Available from: https://www.euromomo.eu/graphs-and-maps. [cited 2022 Jul 25]
Verordnung über die Erweiterung der Meldepflicht nach § 6 Absatz 1 Satz 1 Nummer 1 des Infektionsschutzgesetzes auf Hospitalisierungen in Bezug auf die Coronavirus-Krankheit-2019 Vom 11. Juli 2021 [Internet]. Available from: https://www.bundesanzeiger.de/pub/publication/cOkgVOjc5QJiLFoaIQK/content/cOkgVOjc5QJiLFoaIQK/BAnz%20AT%2012.07.2021%20V1.pdf?inline. [cited 2022 Jul 25].
Lampl BMJ, Lang M, Jochem C, Leitzmann MF, Salzberger B. COVID or not COVID: attributing and reporting cause of death in a community cohort. Public Health. 2022;205:157–63.
Acknowledgements
We thank the members of the contact tracing teams for collecting the data.
Funding
This research did not receive any funding.
Author information
Authors and Affiliations
Contributions
Conceptualization BL and BS; data curation: BL; formal analysis: BL; methodology: BL; project administration: BL; writing—original draft: BL. Writing—review and editing: BL, BE, ML and BS.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
Ethics approval
Not applicable. Data were collected as part of routine investigations based on the German Infection Protection Act (Infektionsschutzgesetz, IfSG).
Consent to participate/consent to publish
Not applicable. Data were collected as part of routine investigations based on the German Infection Protection Act (Infektionsschutzgesetz, IfSG). Identifying information on individual patients/cases is not provided in the article.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lampl, B.M.J., Edenharter, B., Leitzmann, M.F. et al. COVID-19-related deaths: a 2-year inter-wave comparison of mortality data from Germany. Infection 51, 1147–1152 (2023). https://doi.org/10.1007/s15010-023-01982-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-023-01982-4