Abstract
Purpose
This study aimed to evaluate the clinical significance of toxin positivity and toxin gene load, and the relation between them in the broad spectrum of Clostridium difficile infection (CDI) including colonization, significant diarrhea, and severe disease.
Methods
We included 2671 fecal samples submitted for CDI diagnosis and 180 samples from healthy individuals. The clinical spectrum was categorized as category I (toxigenic C. difficile positive without clinical CDI criteria), category II (mild CDI), and category III (severe CDI). Clinical parameters were compared based on toxin EIA and tcdB C t values. C t values of tcdB PCR for predicting toxin EIA positivity were assessed using receiver-operating characteristic (ROC) curves.
Results
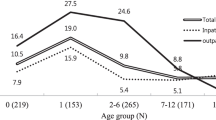
The median C t values of tcdB PCR and toxin positivity were not significantly correlated with clinical spectrum of CDI (27.5, 28.2, and 26.1 for tcdB C t and 55.0, 56.6, and 60.9% for toxin EIA positivity in category I, II, and III, respectively, P > 0.05). There were significant differences in the tcdB C t values between toxin EIA-positive and -negative groups (P < 0.001). Optimal cutoff for the tcdB C t value for estimating toxin EIA positivity was 26.3 with 79.3% sensitivity and 83.6% specificity with good area under the curves (AUC, 0.848).
Conclusions
The C t values successfully predicted toxin EIA positivity and could be used as a surrogate for toxin EIA positivity in the diagnostic algorithm and routine analysis. Further studies are needed to validate the clinical significance of tcdB PCR C t value in toxigenic C. difficile colonization and infection.



Similar content being viewed by others
References
Martin JS, Monaghan TM, Wilcox MH. Clostridium difficile infection: epidemiology, diagnosis and understanding transmission. Nat Rev Gastroenterol Hepatol. 2016;13:206–16.
Cohen SH, Gerding DN, Johnson S, Kelly CP, Loo VG, McDonald LC, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31:431–55.
Planche TD, Davies KA, Coen PG, Finney JM, Monahan IM, Morris KA, et al. Differences in outcome according to Clostridium difficile testing method: a prospective multicentre diagnostic validation study of C. difficile infection. Lancet Infect Dis. 2013;13:936–45.
Bagdasarian N, Rao K, Malani PN. Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA. 2015;313:398–408.
Polage CR, Gyorke CE, Kennedy MA, Leslie JL, Chin DL, Wang S, et al. Overdiagnosis of Clostridium difficile infection in the molecular test era. JAMA Intern Med. 2015;175:1792–801.
Debast SB, Bauer MP, Kuijper EJ. European Society of Clinical Microbiology and Infectious Diseases: update of the treatment guidance document for Clostridium difficile infection. Clin Microbiol Infect. 2014;20:1–26.
Banaei N, Anikst V, Schroeder LF. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372:2368–9.
Anikst VE, Gaur RL, Schroeder LF, Banaei N. Organism burden, toxin concentration, and lactoferrin concentration do not distinguish between clinically significant and nonsignificant diarrhea in patients with Clostridium difficile. Diagn Microbiol Infect Dis. 2016;84:343–6.
Crobach MJ, Planche T, Eckert C, Barbut F, Terveer EM, Dekkers OM, et al. European Society of Clinical Microbiology and Infectious Diseases: update of the diagnostic guidance document for Clostridium difficile infection. Clin Microbiol Infect. 2016;22:S63–81.
Surawicz CM, Brandt LJ, Binion DG, Ananthakrishnan AN, Curry SR, Gilligan PH, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108:478–98.
Fang FC, Polage CR, Wilcox MH. Point-counterpoint: what is the optimal approach for detection of Clostridium difficile infection? J Clin Microbiol. 2017;55:670–80.
Terhes G, Urban E, Soki J, Hamid KA, Nagy E. Community-acquired Clostridium difficile diarrhea caused by binary toxin, toxin A, and toxin B gene-positive isolates in Hungary. J Clin Microbiol. 2004;42:4316–8.
Truong CY, Gombar S, Wilson R, Sundararajan G, Tekic N, Holubar M, et al. Real-time electronic tracking of diarrheal episodes and laxative therapy enables verification of Clostridium difficile clinical testing criteria and reduction of Clostridium difficile infection rates. J Clin Microbiol. 2017;55:1276–84.
Burnham CA, Carroll KC. Diagnosis of Clostridium difficile infection: an ongoing conundrum for clinicians and for clinical laboratories. Clin Microbiol Rev. 2013;26:604–30.
Burnham CA, Dubberke ER, Kociolek LK, Polage CR, Riley TV. Clostridium difficile-diagnostic and clinical challenges. Clin Chem. 2016;62:310–4.
Polage CR, Solnick JV, Cohen SH. Nosocomial diarrhea: evaluation and treatment of causes other than Clostridium difficile. Clin Infect Dis. 2012;55:982–9.
Banaei N, Schroeder LF. Toxin Immunoassays and Clostridium difficile Infection. JAMA Intern Med. 2016;176:413.
Wilcox MH, Planche T, Fang FC, Gilligan P. What is the current role of algorithmic approaches for diagnosis of Clostridium difficile infection? J Clin Microbiol. 2010;48:4347–53.
Dionne LL, Raymond F, Corbeil J, Longtin J, Gervais P, Longtin Y. Correlation between Clostridium difficile bacterial load, commercial real-time PCR cycle thresholds, and results of diagnostic tests based on enzyme immunoassay and cell culture cytotoxicity assay. J Clin Microbiol. 2013;51:3624–30.
Jazmati N, Hellmich M, Licanin B, Plum G, Kaasch AJ. PCR cycle threshold value predicts the course of Clostridium difficile infection. Clin Microbiol Infect. 2016;22:e7–8.
Truong C, Schroeder LF, Gaur R, Anikst VE, Komo I, Watters C, et al. Clostridium difficile rates in asymptomatic and symptomatic hospitalized patients using nucleic acid testing. Diagn Microbiol Infect Dis. 2017;87:365–70.
Senchyna F, Gaur RL, Gombar S, Truong CY, Schroeder LF, Banaei N. Clostridium difficile PCR cycle threshold predicts free toxin. J Clin Microbiol. 2017;55:2651–60.
Acknowledgements
This work was supported by the Konkuk University Medical Center Research Grant 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, H.N., Kim, H., Moon, HW. et al. Toxin positivity and tcdB gene load in broad-spectrum Clostridium difficile infection. Infection 46, 113–117 (2018). https://doi.org/10.1007/s15010-017-1108-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-017-1108-y