Abstract
Purpose of Review
Positive airway pressure (PAP) therapy is the “gold standard” of treatment for obstructive sleep apnea; however, rates of non-adherence to PAP therapy remain high despite device improvements and the inclusion of PAP education programs in most comprehensive sleep disorders clinics. We aimed to review recent evidence-based trends for improving PAP adherence.
Recent Findings
Remote monitoring and telemedicine interventions in conjunction with mobile patient engagement applications have shown promise in facilitating uptake and maintenance of PAP use. New focus on the bedpartner dyad and managing comorbid conditions are also notable, though more recent evidence for specific interventions is limited.
Summary
Recent trends suggest a shift towards developing more patient-centered programs to support PAP adherence. Advancements in telemedicine and interactive mobile health technologies represent the most promising area of growth for PAP adherence interventions. Continued efforts focused on treatments that address socio-relational factors and comorbid conditions seem warranted.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Strollo PJ, Rogers RM. Obstructive sleep apnea. New England J Med. 1996;334(2):99–104.
Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81.
Calik MW. Treatments for obstructive sleep apnea. J Clin Outcomes Manage. 2016;23(4):181.
Epstein LJ, Kristo D, Strollo PJ, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(03):263–76.
Ayas NT, Fitzgerald JM, Fleetham JA, White DP, Schulzer M, Ryan CF, et al. Cost-effectiveness of continuous positive airway pressure therapy for moderate to severe obstructive sleep apnea/hypopnea. Arch Intern Med. 2006;166(9):977–84.
Guest JF, Helter MT, Morga A, Stradling JR. Cost-effectiveness of using continuous positive airways pressure in the treatment of severe obstructive sleep apnoea/hypopnoea syndrome in the UK. Thorax. 2008;63(10):860–5.
Patel SR, White DP, Malhotra A, Stanchina ML, Ayas NT. Continuous positive airway pressure therapy for treating sleepiness in a diverse population with obstructive sleep apnea: results of a meta-analysis. Arch Intern Med. 2003;163(5):565–71.
Franklin KA, Anttila H, Axelsson S, Gislason T, Maasilta P, Myhre KI, et al. Effects and side-effects of surgery for snoring and obstructive sleep apnea: a systematic review. Sleep. 2009;32(1):27–36.
Engleman HM, Wild MR. Improving CPAP use by patients with the sleep apnoea/hypopnoea syndrome (SAHS). Sleep Med Rev. 2003;7(1):81–99.
Antic NA, Catcheside P, Buchan C, Hensley M, Naughton MT, Rowland S, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34(1):111–9.
Barbé F, Durán-Cantolla J, Capote F, de la Peña M, Chiner E, Masa JF, et al. Long-term effect of continuous positive airway pressure in hypertensive patients with sleep apnea. Am J of Respir and Crit Care Med. 2010;181(7):718–26.
Weaver TE, Maislin G, Dinges DF, Bloxham T, George CFP, Greenberg H, et al. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007;30(6):711–9.
Centers for Medicare and Medicaid Services (CMS). Positive airway pressure (PAP) devices: complying with documentation and coverage requirements. In: Service DoHaH, editor. U.S. Centers for Medicare & Medicaid Services. Baltimore, MD: Medicare Learning Network; 2016.
Wild MR, Engleman HM, Douglas NJ, Espie CA. Can psychological factors help us to determine adherence to CPAP? A prospective study. Eur Respir J. 2004;24(3):461–5.
Means MK, Edinger JD, Husain AM. CPAP compliance in sleep apnea patients with and without laboratory CPAP titration. Sleep Breath. 2004;8(1):7–14.
Shapiro GK, Shapiro CM. Factors that influence CPAP adherence: an overview. Sleep Breath. 2010;14(4):323–35.
BaHammam AS, Singh T, George S, Acosta KL, Barataman K, Gacuan DE. Choosing the right interface for positive airway pressure therapy in patients with obstructive sleep apnea. Sleep Breath. 2017;21(3):569–75.
Sin DD, Mayers I, Man GCW, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430–5.
Smith I, Lasserson TJ, Haniffa M. Interventions to improve use of continuous positive airway pressure for obstructive sleep apnoea. Cochrane Database of Syst Rev. 2004;(4):1–81.
Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15(6):343–56.
Kribbs NB, Pack AI, Kline LR, Smith PL, Schwartz AR, Schubert NM, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993;147(4):887–95.
Richards D, Bartlett DJ, Wong K, Malouff J, Grunstein RR. Increased adherence to CPAP with a group cognitive behavioral treatment intervention: a randomized trial. Sleep. 2007;30(5):635–40.
Olsen S, Smith SS, Oei TP, Douglas J. Motivational interviewing (MINT) improves continuous positive airway pressure (CPAP) acceptance and adherence: a randomized controlled trial. J Consult Clin Psychol. 2012;80(1):151–63.
Aloia MS, Arnedt JT, Riggs RL, Hecht J, Borrelli B. Clinical management of poor adherence to CPAP: motivational enhancement. Behav Sleep Med. 2004;2(4):205–22.
Hoy CJ, Vennelle M, Kingshott RN, Engleman HM, Douglas NJ. Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome? Am J Respir Crit Care Med. 1999;159(4):1096–100.
Parthasarathy S, Wendel C, Haynes PL, Atwood C, Kuna S. A pilot study of CPAP adherence promotion by peer buddies with sleep apnea. J Clin Sleep Med. 2013;9(06):543–50.
Bartlett D, Wong K, Richards D, Moy E, Espie CA, Cistulli PA, et al. Increasing adherence to obstructive sleep apnea treatment with a group social cognitive therapy treatment intervention: a randomized trial. Sleep. 2013;36(11):1647–54.
Chen X, Chen W, Hu W, Huang K, Huang J, Zhou Y. Nurse-led intensive interventions improve adherence to continuous positive airway pressure therapy and quality of life in obstructive sleep apnea patients. Patient Prefer Adherence. 2015;9:1707.
Smith CE, Dauz E, Clements F, Werkowitch M, Whitman R. Patient education combined in a music and habit-forming intervention for adherence to continuous positive airway (CPAP) prescribed for sleep apnea. Patient Educ Couns. 2009;74(2):184–90.
D’Rozario AL, Galgut Y, Bartlett DJ. An update on behavioural interventions for improving adherence with continuous positive airway pressure in adults. Curr Sleep Med Rep. 2016;2(3):166–79.
Rauscher H, Formanek D, Popp W, Zwick H. Self-reported vs measured compliance with nasal CPAP for obstructive sleep apnea. Chest. 1993;103(6):1675–80.
Watson NF. Health care savings: the economic value of diagnostic and therapeutic care for obstructive sleep apnea. J Clin Sleep Med. 2016;12(08):1075–7.
Hwang D. Monitoring progress and adherence with positive airway pressure therapy for obstructive sleep apnea: the roles of telemedicine and mobile health applications. Sleep Med Clin. 2016;11(2):161–71.
Isetta V, Negrín MA, Monasterio C, Masa JF, Feu N, Álvarez A, et al. A Bayesian cost-effectiveness analysis of a telemedicine-based strategy for the management of sleep apnoea: a multicentre randomised controlled trial. Thorax. 2015;70(11):1054–61.
Turino C, de Batlle J, Woehrle H, Mayoral A, Castro-Grattoni AL, Gómez S, et al. Management of continuous positive airway pressure treatment compliance using telemonitoring in obstructive sleep apnoea. Eur Respir J. 2017;49(2):1601128.
Stepnowsky CJ, Palau JJ, Marler MR, Gifford AL. Pilot randomized trial of the effect of wireless telemonitoring on compliance and treatment efficacy in obstructive sleep apnea. J Med Internet Res. 2007;9(2):e14.
• Hoet F, Libert W, Sanida C, Van den Broecke S, Bruyneel AV, Bruyneel M. Telemonitoring in continuous positive airway pressure-treated patients improves delay to first intervention and early compliance: a randomized trial. Sleep Med. 2017;39:77–83 A small study which found that telemonitoring of PAP use reduced delays to first intervention for PAP device issues. Telemonitoring was not found to improve the percentage of nights with adequate PAP adherence.
Sedkaoui K, Leseux L, Pontier S, Rossin N, Leophonte P, Fraysse J-L, et al. Efficiency of a phone coaching program on adherence to continuous positive airway pressure in sleep apnea hypopnea syndrome: a randomized trial. BMC Pulm Med. 2015;15(1):102–9.
Frasnelli M, Baty F, Niedermann J, Brutsche MH, Schoch OD. Effect of telemetric monitoring in the first 30 days of continuous positive airway pressure adaptation for obstructive sleep apnoea syndrome: a controlled pilot study. J Telemed Telecare. 2016;22(4):209–14.
Munafo D, Hevener W, Crocker M, Willes L, Sridasome S, Muhsin M. A telehealth program for CPAP adherence reduces labor and yields similar adherence and efficacy when compared to standard of care. Sleep Breath. 2016;20(2):777–85.
• Woehrle H, Ficker JH, Graml A, Fietze I, Young P, Teschler H, et al. Telemedicine-based proactive patient management during positive airway pressure therapy. Somnologie. 2017;21(2):121–7 Observed that use of telemonitoring-triggered interventions for PAP non-adherence reduced risk for PAP termination during first year of therapy.
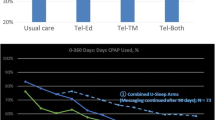
•• Hwang D, Chang JW, Benjafield AV, Crocker ME, Kelly C, Becker KA, et al. Effect of telemedicine education and telemonitoring on continuous positive airway pressure adherence: the Tele-OSA randomized trial. Am J Respir and Crit Care Med. 2018;197(1):117–26 RCT of telemedicine-based education and telemonitoring with automated feedback. Greatest benefits to PAP adherence found for interventions of telemonitoring with automated feedback.
•• Woehrle H, Arzt M, Graml A, Fietze I, Young P, Teschler H, et al. Effect of a patient engagement tool on positive airway pressure adherence: analysis of a German healthcare provider database. Sleep Med. 2018;41:20–6 This study found that patients who also had access to a patient engagement mobile health program reported greater PAP adherence compared to telemonitoring-guided monitoring only.
Lynch S, Blase A, Wimms A, Erikli L, Benjafield A, Kelly C, Willes L. Retrospective descriptive study of CPAP adherence associated with use of the ResMed myAir application. Resmed Sci Cent. 2015. Available from: http://www.resmed.com/us/dam/documents/products/data-management/myair/1018839_myair_white-paper_amer_eng.pdf
• Hostler JM, Sheikh KL, Andrada TF, Khramtsov A, Holley PR, Holley AB. A mobile, web-based system can improve positive airway pressure adherence. J Sleep Res. 2017;26(2):139–46 Small trial suggests that patients who used a mobile health application, which encouraged increased engagement in PAP treatment, used PAP on more nights and more nights > 4+ h.
Isetta V, Torres M, González K, Ruiz C, Dalmases M, Embid C, et al. A new mHealth application to support treatment of sleep apnoea patients. J Telemed Telecare. 2017;23(1):14–8.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215.
Dzierzewski JM, Wallace DM, Wohlgemuth WK. Adherence to continuous positive airway pressure in existing users: self-efficacy enhances the association between continuous positive airway pressure and adherence. J Clin Sleep Med. 2016;12(02):169–76.
ResMed. ResTraxx Online. Basel, Switzerland. https://www.respshop.com/manuals/resmed-s9-wireless-module-368797-restraxx-online.pdf
Guralnick AS, Balachandran JS, Szutenbach S, Adley K, Emami L, Mohammadi M, et al. Educational video to improve CPAP use in patients with obstructive sleep apnoea at risk for poor adherence: a randomised controlled trial. Thorax. 2017;72(12):1132–9.
McArdle N, Kingshott R, Engleman HM, Mackay TW, Douglas NJ. Partners of patients with sleep apnoea/hypopnoea syndrome: effect of CPAP treatment on sleep quality and quality of life. Thorax. 2001;56(7):513–8.
Beninati W, Harris CD, Herold DL, Shepard JW Jr, editors. The effect of snoring and obstructive sleep apnea on the sleep quality of bed partners. Mayo Clin Proc. New York City: Elsevier; 1999.
Parish JM, Lyng PJ. Quality of life in bed partners of patients with obstructive sleep apnea or hypopnea after treatment with continuous positive airway pressure. Chest. 2003;124(3):942–7.
Homish GG, Leonard KE. Spousal influence on general health behaviors in a community sample. Am J Health Behav. 2008;32(6):754–63.
Falba TA, Sindelar JL. Spousal concordance in health behavior change. Health Serv Res. 2008;43(1p1):96–116.
Luyster FS, Dunbar-Jacob J, Aloia MS, Martire LM, Buysse DJ, Strollo PJ. Patient and partner experiences with obstructive sleep apnea and CPAP treatment: a qualitative analysis. Behav Sleep Med. 2016;14(1):67–84.
Baron KG, Smith TW, Berg CA, Czajkowski LA, Gunn H, Jones CR. Spousal involvement in CPAP adherence among patients with obstructive sleep apnea. Sleep Breath. 2011;15(3):525–34.
Batool-Anwar S, Baldwin CM, Fass S, Quan SF. Role of spousal involvement in continuous positive airway pressure (CPAP) adherence in patients with obstructive sleep apnea (OSA). Southwest J Pulm Crit Care. 2017;14(5):213–27.
Baron KG, Gunn HE, Wolfe LF, Zee PC. Relationships and CPAP adherence among women with obstructive sleep apnea. Sleep Sci Pract. 2017;1(1):10.
• Luyster FS, Aloia MS, Buysse DJ, Dunbar-Jacob J, Martire LM, Sereika SM, et al. A couples-oriented intervention for positive air- way pressure therapy adherence: a pilot study of obstructive sleep apnea patients and their partners. Behav Sleep Med. 2018:1–12. https://doi.org/10.1080/15402002.2018.1425871. A pilot investigation of a motivational enhancement-based education and support intervention that involved patients’ spouses/partners.
• Krakow B, McIver ND, Ulibarri VA, Nadorff MR. Retrospective, nonrandomized controlled study on autoadjusting, dual-pressure positive airway pressure therapy for a consecutive series of complex insomnia disorder patients. Nat and Science of Sleep. 2017;9:81–95 This study found COMISA patients who previously “failed” CPAP and used alternative PAP modalities (ABPAP and ASV) that were hypothesized to be more tolerable experienced improvements in insomnia symptoms.
• Sweetman A, Lack L, Lambert S, Gradisar M, Harris J. Does comorbid obstructive sleep apnea impair the effectiveness of cognitive and behavioral therapy for insomnia? Sleep Med. 2017;39:38–46 Investigation of CBTi in patients with insomnia and COMISA before beginning PAP therapy. The authors found that treatment was effective in both groups, which suggests that CBTi before PAP could be effective strategy for managing COMISA.
BaHammam AS, Kendzerska T, Gupta R, Ramasubramanian C, Neubauer DN, Narasimhan M, et al. Comorbid depression in obstructive sleep apnea: an under-recognized association. Sleep and Breath. 2016;20(2):447–56.
Krakow BJ, Ulibarri VA, Moore BA, McIver ND. Posttraumatic stress disorder and sleep-disordered breathing: a review of comorbidity research. Sleep Med Rev. 2015;24:37–45.
American Academy of Sleep Medicine. The international classification of sleep disorders, diagnostic and coding manual. 3rd ed. Westchester, IL: American Academy of Sleep Medicine; 2014.
Luyster FS, Buysse DJ, Strollo PJ. Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med. 2010;6(02):196–204.
Guilleminault C, Eldridge FL, Dement WC. Insomnia with sleep apnea: a new syndrome. Science. 1973;181(4102):856–8.
Sweetman AM, Lack LC, Catcheside PG, Antic NA, Chai-Coetzer CL, Smith SS, et al. Developing a successful treatment for co-morbid insomnia and sleep apnoea. Sleep Med Rev. 2017;33:28–38.
Bjornsdottir E, Janson C, Arnardóttir E, Pack A, Gíslason T, Benediktsdottir B. Symptoms of insomnia among OSA patients before and after 2 years of PAP treatment. Sleep Med. 2013;14:e74.
Wickwire EM, Smith MT, Birnbaum S, Collop NA. Sleep maintenance insomnia complaints predict poor CPAP adherence: a clinical case series. Sleep Med. 2010;11(8):772–6.
Smith S, Dunn N, Douglas J, Jorgensen G. Sleep onset insomnia is associated with reduced adherence to CPAP therapy. Sleep Biol Rhythms. 2009;7:116.
Nguyên X-L, Chaskalovic J, Rakotonanahary D, Fleury B. Insomnia symptoms and CPAP compliance in OSAS patients: a descriptive study using data mining methods. Sleep Med. 2010;11(8):777–84.
Edinger JD, Wohlgemuth WK, Radtke RA, Marsh GR, Quillian RE. Cognitive behavioral therapy for treatment of chronic primary insomnia: a randomized controlled trial. J Am Med Assoc. 2001;285(14):1856–64.
Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125–33.
Wallace DM, Sawyer AM, Shafazand S. Comorbid insomnia symptoms predict lower 6-month adherence to CPAP in US veterans with obstructive sleep apnea. Sleep Breath. 2018;22(1):5–15.
Eysteinsdottir B, Gislason T, Pack AI, Benediktsdottir B, Arnardottir ES, Kuna ST, et al. Insomnia complaints in lean patients with obstructive sleep apnea negatively affect positive airway pressure treatment adherence. J Sleep Res. 2017;26(2):159–65.
• Crawford MR, Turner AD, Wyatt JK, Fogg LF, Ong JC. Evaluating the treatment of obstructive sleep apnea comorbid with insomnia disorder using an incomplete factorial design. Contemp Clin Trials. 2016;47:146–52 Description and rationale for active RCT designed to evaluate sequence of treatments (CBTi and PAP) for COMISA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Earl Crew, William Wohlgemuth, and Douglas Wallace declare no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Sleeping and Breathing
Rights and permissions
About this article
Cite this article
Crew, E.C., Wohlgemuth, W.K. & Wallace, D.M. Improving Adherence to PAP Therapy: an Update. Curr Pulmonol Rep 8, 1–13 (2019). https://doi.org/10.1007/s13665-019-0220-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-019-0220-0