Abstract
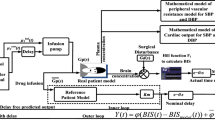
Anesthetic agent propofol needs to be administered at an appropriate rate to prevent hypotension and postoperative adverse reactions. To comprehend more suitable anesthetic drug rate during surgery is a crucial aspect. The main objective of this proposal is to design robust automated control system that work efficiently in most of the patients with smooth BIS and minimum variations of propofol during surgery to avoid adverse post reactions and instability of anesthetic parameters. And also, to design advanced computer control system that improves the health of patient with short recovery time and less clinical expenditures. Unlike existing research work, this system administrates propofol as a hypnotic drug to regulate BIS, with fast bolus infusion in induction phase and slow continuous infusion in maintenance phase of anesthesia. The novelty of the paper lies in possibility to simplify the drug sensitivity-based adaption with infusion delay approach to achieve closed-loop control of hypnosis during surgery. Proposed work uses a brain concentration as a feedback signal in place of the BIS signal. Regression model based estimated sensitivity parameters are used for adaption to avoid BIS signal based frequent adaption procedure and large offset error. Adaptive smith predictor with lead–lag filter approach is applied on 22 different patients’ model identified by actual clinical data. The actual BIS and propofol infusion signals recorded during clinical trials were used to estimate patient’s sensitivity parameters EC50 and λ. Simulation results indicate that patient’s drug sensitivity parameters based adaptive strategy facilitates optimal controller performance in most of the patients. Results are obtained with proposed scheme having less settling time, BIS oscillations and small offset error leads to adequate depth of anesthesia. A comparison with manual control mode and previously reported system shows that proposed system achieves reduction in the total variations of the propofol dose. Proposed adaptive scheme provides better performance with less oscillation in spite of computation delay, surgical stimulations and patient variability. Proposed scheme also provides improvement in robustness and may be suitable for clinical practices.












Similar content being viewed by others
References
Santiago T, Juan M, Josh AR, Reboso H. Adaptive computer control of anesthesia in humans. Comput Methods Biomed Eng. 2009;12:727–34.
Li T-N, Li Y. Depth of anaesthesia monitors and the latest algorithms. Asian Pac J Trop Med. 2004;7:429–37.
Ilyas M, Butt MFU, Bilal M, Mahmood K, Khaqan A, Riaz RA. A review of modern control strategies for clinical evaluation of propofol anesthesia administration employing hypnosis level regulation. Hindawi BioMed Res Int. 2017;1:12.
Bibian S, Ries CR, Huzmezan M, Dumont G. Introduction to automated drug delivery in clinical anesthesia. Eur J Control. 2005;11:535–57.
Reboso JA, Méndez JA, Reboso HJ, León AM. Design and implementation of a closed-loop control system for infusion of propofol guided by bispectral index (BIS). Acta Anaesthesiol Scand. 2012;56:1032–41.
Ionescu CM, Keyser RD, Torrico BC, Smet TD, Struys MMRF, Normey-Rico JE. Robust predictive control strategy applied for propofol dosing using BIS as a controlled variable during anesthesia. IEEE Trans Biomed Eng. 2008;55(9):2161–70.
De Smet T, Struys MM, Neckebroek MM, Van den Hauwe K, Bonte S, Mortier EP. The accuracy and clinical feasibility of a new Bayesian-based closed-loop control system for propofol administration using the bispectral index as a controlled variable. Anesth Analg. 2008;107:1200–10.
Struys MM, De Smet T, Versichelen LF, Van De Velde S, Van den Broecke R, Mortier EP. Comparison of closed-loop controlled administration of propofol using bispectral Index as the controlled variable versus standard practice controlled administration. Anesthesiology. 2001;95:6–17.
Martín-Mateos I, Méndez Pérez JA, Reboso Morales JA, Gómez-González JF. Adaptive pharmacokinetic and pharmacodynamic modeling to predict propofol effect using BIS-guided anesthesia. Comput Biol Med. 2016;75:173–80.
Merigoa Luca, Beschi Manuel, Padula Fabrizio, Latronico Nicola, Paltenghi Massimiliano, Visioli Antonio. Event-based control of depth of hypnosis in anesthesia. Comput Methods Progr Biomed. 2017;147(63–8):3.
Liu N, Le Guen M, Benabbes-Lambert F, Chazot T, Trillat B, Sessler DI, et al. Feasibility of closed loop titration of propofol and remifentanil guided by the spectral M-entropy monitor. Anesthesiology. 2012;116:286–95.
Heusden KV, Dumont GA, Soltesz K, Petersen CL, Umedaly A, West N, et al. Design and clinical evaluation of robust PID control of propofol anesthesia in children. IEEE Trans Control Syst Technol. 2014;22:491–501.
Padula F, Ionescu C, Latronico N, Paltenghi M, Visioli A, Vivacqua G. Optimized PID control of depth of hypnosis in anesthesia. Comput Methods Progr Biomed. 2017;144:21–35.
Yelneedi S, Samavedham L, Rangaiah GP. A comparative study of three advanced controllers for the regulation of hypnosis. J Process Control. 2009;19:1458–69.
Ionescu C, Machado JT, De Keyser R, Decruyenaere J, Struys M. Nonlinear dynamics of the patient’s response to drug effect during general anesthesia. Commun Nonlinear Sci Numer Simul. 2015;20:914–26.
Ionescu CM, Hodrea R, Keyser R. Variable time-delay estimation for anesthesia control during intensive care. IEEE Trans Biomed Eng. 2011;58:363–9.
Nascu I, Krieger A, Ionescu CM, Pistikopoulos EN. Advanced model-based control studies for the induction and maintenance of intravenous anaesthesia. IEEE Trans Biomed Eng. 2015;62:832–41.
Yoshihito S, Eiko F, Gotaro S, Mituhiko A, Kazuhiko F. A model-predictive hypnosis control system under total intravenous anesthesia. IEEE Trans Biomed Eng. 2008;55:874–87.
Dumont GA, Martinez A, Ansermino MJ. Robust control of depth of anesthesia. Int J Adapt Control Signal Process. 2009;23:435–54.
Ionescu CM, Copot D, Keyser R. Anesthesiologist in the loop and predictive algorithm to maintain hypnosis while mimicking surgical disturbance. IFAC Papers Online. 2017;50(1):15080–5.
Saxena S, Yogesh VH. Simple approach to design PID controller via internal model control. Arab J Sci Eng. 2016;41(9):3473–89.
Robin DE, Ionescu CM. A no-nonsense control engineering approach to anaesthesia control during induction phase. In: 8th IFAC symposium on biological and medical systems; 2012, pp. 29–31
Sartori V, Schumacher PM, Bouillon T, Luginbuehl M, Morari M. On-line estimation of propofol pharmacodynamics parameters. In: Proceedings of the 27th annual international conference of the IEEE engineering in medicine and biology, Shanghai, China; 2005, pp. 74–77.
Geun JC, Hyun K, Chong WB, Yong HJ, Je JL. Comparison of bolus versus continuous infusion of propofol for procedural sedation: a meta-analysis. Curr Med Res Opin. 2017;33(11):1935–43.
Shah NK, Harris M, Govindugari K, Rangaswamy HB, Jeon H. Effect of propofol titration v/s bolus during induction of anesthesia on hemodynamics and bispectral index. Middle East J Anaesthesiol. 2011;21(2):275–81.
Martin-Mateos I, Mendez-Perez JA, Reboso JA, Leon A. Modeling propofol pharmacodynamics using BIS-guided anesthesia. Anaesth J. 2013;68:1132–40.
Robayo F, Sendoya D, Hodrea R, Robin DE, Ionescu CM. Estimating the time-delay for predictive control in general anesthesia. In: IEEE control and decision conference (CCDC); 2010, pp. 3719–3724.
Ostertagová Eva. Modeling using polynomial regression. Proc Eng. 2012;48(500):506.
Schnider TW, Minto CF, Shafer SL, Gambus PL, Andresen C, Goodale DB. The influence of age on propofol pharmacodynamics. Anesthesiology. 1999;90:1502–16.
Schuttler J, Ihmsen H. Population pharmacokinetics of propofol: a multicenter study. Anesthesiology. 2000;92(3):727–38.
Abdulla SA, Wen P. Robust internal model control for depth of anesthesia. Int J Mechatron Autom. 2011;1(1):1–8.
Gopi Krishna PV, Subramanyamb MV, Satyaprasad K. Design of cascaded IMC-PID controller with improved filter for disturbance rejection. Int J Appl Sci Eng. 2014;2(12):127–41.
Absalom AR, Sutcliffe N, Kenny GN. Closed-loop control of anesthesia using bispectral index: performance assessment in patients undergoing major orthopedic surgery under combined general and regional anesthesia. Anesthesiology. 2002;96:67–73.
Beck CE, Pohl B, Janda M, Bajorat J, Hofmockel R. Depth of anaesthesia during intubation: comparison between propofol and thiopentone. Der Anaesth. 2006;55(4):401–6.
Absalom AR, Struys MMRF. An overview of target controlled infusions and total intravenous anaesthesia. San Diego: Academia Press; 2007.
Kaya Ibrahim. IMC based automatic tuning method for PID controllers in a smith predictor configuration. Comput Chem Eng. 2004;28(3):281–90.
Ingole DD, Sonawane DN, Naik VV. Linear model predictive controller for closed-loop control of intravenous anesthesia with time delay. ACEEE Int J Control Syst Instrum. 2013;4:8–15.
Soltesz K, Heusden K, Dumont GA, et al. Closed-loop anesthesia in children using a PID controller: a pilot study. In: IFAC conference on advances in PID control; 2012.
Sakai T, Matsuki A, White PF, et al. Use of an EEG-bispectral closed-loop delivery system for administering propofol. Acta Anesthesiol Scand. 2000;44:1007–14.
Ajwad SA, Iqbal J, Ullah MI, et al. A systematic review of current and emergent manipulator control approaches. Front Mech Eng. 2015;10:198–210.
Zhao Z, Liu Z, Zhang J. IMC-PID tuning method based on ensitivity specification for process with time-delay. J Cent S Univ Technol. 2011;18:1153–60.
Saxena Sahaj, Yogesh VH. A simulation study on optimal IMC based PI/PID controller for mean arterial blood pressure. Biomed Eng Lett. 2012;2:240–8.
Acknowledgements
The authors would like to thank to anesthesia department team of the SMIMER hospital, Surat for providing the clinical environment facility and drug dose combination as per proposed scheme. The authors are grateful to anonymous reviewers for their useful suggestions to improve the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Ethical Approval
All procedures performed in study involving human participants were in accordance with the ethical standards of the Surat Municipal Institute of Medical Education and Research (SMIMER), India and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Patel, B., Patel, H., Vachhrajani, P. et al. Adaptive smith predictor controller for total intravenous anesthesia automation. Biomed. Eng. Lett. 9, 127–144 (2019). https://doi.org/10.1007/s13534-018-0090-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13534-018-0090-3