Abstract
Objectives
Summarize the existing evidence regarding the prevalence and risk factors of frailty in stroke patients.
Design
A meta-analysis and systematic review.
Participants
Stroke patients in hospitals or communities.
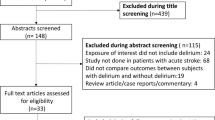
Methods
We undertook a systematic review and meta-analysis using articles available in 8 databases, including PubMed, The Cochrane Library, Web of Science, Embase, Chinese Biomedical Database (CBM), China National Knowledge Infrastructure Database (CNKI), Wanfang Database, and Weipu Database (VIP) from January 1990 to April 2022. Studies were quality rated using the Newcastle-Ottawa Scale and Agency for Healthcare Research and Quality tool.
Results
A total of 24 studies involving 30,423 participants were identified. The prevalence of frailty and pre-frailty in stroke patients was 27% (95%CI: 0.23–0.31) and 47.9% (95%CI: 0.43–0.53). Female gender (OR = 1.76, 95%CI: 1.63–1.91), advanced age (MD = 6.73, 95%CI: 3.55–9.91), diabetes (OR = 1.34, 95%CI: 1.06–1.69), hyperlipidemia (OR = 1.46, 95%CI: 1.04–2.04), atrial fibrillation (OR = 1.36, 95%CI: 1.01–1.82), National Institutes of Stroke Scale (NIHSS) admission scores (MD = 2.27, 95%CI: 1.72–2.81) were risk factors of frailty in stroke patients.
Conclusions
Frailty was more prevalent in stroke patients. Female gender, advanced age, diabetes, hyperlipidemia, atrial fibrillation, and National Institutes of Stroke Scale (NIHSS) admission scores were identified as risk factors for frailty in stroke patients. In the future, medical staff should pay attention to the early screening of frailty in high-risk groups and provide information on its prevention.



Similar content being viewed by others
References
Johnson CO, Nguyen M, Roth GA. Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019; 18(5): 439–458. doi: https://doi.org/10.1016/s1474-4422(19)30034-1.
Wang LD, Liu JM, Yang G, et al. Brief report on stroke prevention and treatment in China, 2020. Chinese Circulation Journal. 2019; 34(2): 105–119. doi: https://doi.org/10.3969/j.issn.1000-3614.2019.02.001. [in Chinese]
Feigin VL, Stark BA, Johnson CO, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021; 20(10): 795–820. doi: https://doi.org/10.1016/S1474-4422(21)00252-0.
Tu WJ, Hua Y, Yan F, et al. Prevalence of stroke in China, 2013–2019: A population-based study. The Lancet Regional Health — Western Pacific. 2022; 10050. doi: https://doi.org/10.1016/j.lanwpc.2022.100550.
Smithard DG. Stroke in frail older people. Geriatrics. 2017; 2(3):24. doi: https://doi.org/10.3390/geriatrics2030024.
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001; 56(3): M146–156. doi: https://doi.org/10.1093/gerona/56.3.m146.
Noguchi M, Kubo H, Kanai M, et al. Relationship between pre-stroke frailty status and short-term functional outcome in older patients with acute stroke-A mediation analysis. Arch Gerontol Geriatr. 2021; 94: 104370. doi: https://doi.org/10.1016/j.archger.2021.104370.
Joyce N, Atkinson T, Mc Guire K, et al. Frailty and stroke thrombectomy outcomes-an observational cohort study. Age Ageing. 2022; 51(2): afab260. doi: https://doi.org/10.1093/ageing/afab260.
Schnieder M, Bähr M, Kirsch M, et al. Analysis of frailty in geriatric patients as a prognostic factor in endovascular treated patients with large vessel occlusion strokes. J Clin Med. 2021; 10(10): 2171. doi: https://doi.org/10.3390/jcm10102171.
Kim MG, Gandhi C, Azizkhanian I, et al. Frailty and spontaneous intracerebral hemorrhage: Does the modified frailty index predict mortality. Clin Neurol Neurosurg. 2020; 194: 105816. doi: https://doi.org/10.1016/j.clineuro.2020.105816.
Li M, Song QY, Wang S, et al. Study on the frailty-related serum markers in older patients with cerebral infarction. Chinese Journal of Geriatrics. 2018; 37(6): 641–645. doi: https://doi.org/10.3760/cma.j.issn.0254-9026.2018.06.008. [in Chinese]
Burton JK, Stewart J, Blair M, et al. Prevalence and implications of frailty in acute stroke: systematic review & meta-analysis. Age Ageing. 2022; 51(3): afac064. doi: https://doi.org/10.1093/ageing/afac064.
Taylor-Rowan M, Cuthbertson G, Keir R, et al. The prevalence of frailty among acute stroke patients, and evaluation of method of assessment. Clin Rehabil. 2019; 33(10): 1688–1696. doi: https://doi.org/10.1177/0269215519841417.
Liao RT, Chen R, Luo WH, Analysis of frailty and influencing factors in adult patients with acute ischemic stroke. Chongqing Medicine. 2022; 1–10. [in Chinese]
Wang LY, Hu XL, Wang XJ, et al. Predictive value of frailty index derived from comprehensive geriatric assessment for frailty of patients with ischemic stroke. Chinese Journal of Modern Nursing. 2022; 28(2): 167–171. doi: https://doi.org/10.3760/cma.j.cn115682-20210709-03049. [in Chinese]
Wang Y, Tao XJ, Dong KS, et al. Correlation between frailty and cognitive dysfunction in patients with acute ischemic stroke. China Medical Herald. 2021; 18(17): 82–84, 89. [in Chinese]
Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015; 4(1): 1. doi: https://doi.org/10.1186/2046-4053-4-1.
Zeng X, Zhang Y, Kwong JS, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015; 8(1): 2–10. doi: https://doi.org/10.1111/jebm.12141.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010; 25(9): 603–605. doi: https://doi.org/10.1007/s10654-010-9491-z.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002; 21(11): 1539–1558. doi: https://doi.org/10.1002/sim.1186.
Fearon P, Mcarthur KS, Garrity K, et al. Prestroke modified rankin stroke scale has moderate interobserver reliability and validity in an acute stroke setting. Stroke. 2012; 43(12): 3184–3188. doi: https://doi.org/10.1161/strokeaha.112.670422.
Fan F, Yang C, Wang QS. Association between frailty and poststroke cognitive impairment in older ischemic stroke patients. Chin J Geriatr Heart Brian Ves Dis. 2018; 20(12): 1253–1257. doi: https://doi.org/10.3969/j.issn.1009-0126.2018.12.006. [in Chinese]
Liao BY. Research on the correlation between Modified Frailty Index and postoperative complications of spontaneous cerebral hemorrhage in older patients. Chengdu Medical College; 2019.
Taylor-Rowan M, Keir R, Cuthbertson G, et al. Pre-stroke frailty is independently associated with post-stroke cognition: a cross-sectional study. J Int Neuropsychol Soc. 2019; 25(5): 501–506. doi: https://doi.org/10.1017/s1355617719000092.
Shang XF, Zhang Y, Li H, et al. Frailty and post-stroke depression in older patients with acute ischemic stroke. Chinese General Practice. 2020; 23(30): 3834–3838. doi: https://doi.org/10.12114/j.issn.1007-9572.2020.00.462. [in Chinese]
Kanai M, Noguchi M, Kubo H, et al. Pre-stroke frailty and stroke severity in elderly patients with acute stroke. J Stroke Cerebrovasc Dis. 2020; 29(12): 105346. doi: https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105346.
Lin W, Su LL, Yu TZ, et al. Frailty and its risk factors in older ischemic stroke patients with sequelae. Chin J Geriatr Heart Brain Ves Dis. 2021; 23(5): 499–502. doi: https://doi.org/10.3969/j.issn.1009-0126.2021.05.014 [in Chinese].
Murrias Quintana A, Benavente Fernández L, Morís De La Tassa G. Frailty in people over 80 years after an ischemic stroke treated with mechanical thrombectomy. Revista Científica de la Sociedad de Enfermería Neurológica (English ed). 2022; 1–8. doi: https://doi.org/10.1016/j.sedeng.2021.07.001.
Fan F. Association between frailty and serum albumin level and post-stroke cognitive impairment in patients with acute ischemic stroke. Chengdu Medical College; 2020.
Pinho J, Küppers C, Nikoubashman O, et al. Frailty is an outcome predictor in patients with acute ischemic stroke receiving endovascular treatment. Age Ageing. 2021; 50(5): 1785–1791. doi: https://doi.org/10.1093/ageing/afab092.
Winovich DT, Longstreth WT, Jr, Arnold AM, et al. Factors Associated With Ischemic Stroke Survival and Recovery in Older Adults. Stroke. 2017; 48(7): 1818–1826. doi: https://doi.org/10.1161/strokeaha.117.016726.
Seamon BA, Simpson KN. The effect of frailty on discharge location for medicare beneficiaries after acute stroke. Arch Phys Med Rehabil. 2019; 100(7): 1317–1323. doi: https://doi.org/10.1016/j.apmr.2019.02.006.
Evans NR, Wall J, To B, et al. Clinical frailty independently predicts early mortality after ischaemic stroke. Age Ageing. 2020; 49(4): 588–591. doi: https://doi.org/10.1093/ageing/afaa004.
Zhang W, Anderson CS, Kilkenny MF, et al. Hospital admissions prior to primary intracerebral haemorrhage and relevant factors associated with survival. J Stroke Cerebrovasc Dis. 2020; 29(9): 105026. doi: https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105026.
Kilkenny MF, Phan HT, Lindley RI, et al. Utility of the hospital frailty risk score derived from administrative data and the association with stroke outcomes. Stroke. 2021; 52(9): 2874–2781. doi: https://doi.org/10.1161/strokeaha.120.033648.
Wæhler IS, Saltvedt I, Lydersen S, et al. Association between in-hospital frailty and health-related quality of life after stroke: the Nor-COAST study. BMC Neurol. 2021; 21(1): 100. doi: https://doi.org/10.1186/s12883-021-02128-5.
Pilotto A, Brass C, Fassbender K, et al. Premorbid frailty predicts short- and long-term outcomes of reperfusion treatment in acute stroke. J Neurol. 2022; 269(6): 3338–3342. doi: https://doi.org/10.1007/s00415-022-10966-7.
Siriwardhana DD, Hardoon S, Rait G, et al. Prevalence of frailty and prefrailty among community-dwelling older adults in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open. 2018; 8(3): e018195. doi: https://doi.org/10.1136/bmjopen-2017-018195.
Franse CB, Van Grieken A, Qin L, et al. Socioeconomic inequalities in frailty and frailty components among community-dwelling older citizens. PLoS One. 2017; 12(11): e0187946. doi: https://doi.org/10.1371/journal.pone.0187946.
Gomes CDS, Guerra RO, Wu YY, et al. Social and economic predictors of worse frailty status occurrence across selected countries in North and South America and Europe. Innov Aging, 2018; 2(3): igy037. doi: https://doi.org/10.1093/geroni/igy037.
Abellan van Kan G, Rolland Y, Bergman H, et al. The IANA Task Force on frailty assessment of older people in clinical practice. J Nutr Health Aging. 2008; 12(1): 29–37. doi: https://doi.org/10.1007/BF02982161.
Gilbert T, Neuburger J, Kraindler J, et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet. 2018; 391(10132): 1775–1782. doi: https://doi.org/10.1016/S0140-6736(18)30668-8.
Velanovich V, Antoine H, Swartz A, et al. Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. J Surg Res. 2013; 183(1): 104–110. doi: https://doi.org/10.1016/j.jss.2013.01.021.
Xu R, Li Q, Guo F, et al. Prevalence and risk factors of frailty among people in rural areas: a systematic review and meta-analysis. BMJ Open. 2021; 11(4): e043494. doi: https://doi.org/10.1136/bmjopen-2020-043494.
Appelros P, Nydevik I, Viitanen M. Poor outcome after first-ever stroke: predictors for death, dependency, and recurrent stroke within the first year. Stroke. 2003; 34(1): 122–126. doi: https://doi.org/10.1161/01.str.0000047852.05842.3c.
Bushnell CD, Chaturvedi S, Gage KR, et al. Sex differences in stroke: Challenges and opportunities. J Cereb Blood Flow Metab. 2018; 38(12): 2179–2191. doi: https://doi.org/10.1177/0271678x18793324.
Navaneethan PR, Kekre A, Jacob KS, et al. Vitamin D deficiency in postmenopausal women with pelvic floor disorders. J Midlife Health. 2015; 6(2): 66–69. doi: https://doi.org/10.4103/0976-7800.158948.
Gale CR, Cooper C, Sayer AA. Prevalence of frailty and disability: findings from the English Longitudinal Study of Ageing. Age Ageing. 2015; 44(1): 162–165. doi: https://doi.org/10.1093/ageing/afu148.
Collard RM, Boter H, Schoevers RA, et al. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012; 60(8): 1487–1492. doi: https://doi.org/10.1111/j.1532-5415.2012.04054.x.
Li G, Prior JC, Leslie WD, et al. Frailty and risk of fractures in patients with type 2 diabetes. Diabetes Care. 2019; 42(4): 507–513. doi: https://doi.org/10.2337/dc18-1965.
Lau LH, Lew J, Borschmann K, et al. Prevalence of diabetes and its effects on stroke outcomes: A meta-analysis and literature review. J Diabetes Investig. 2019; 10(3): 780–792. doi: https://doi.org/10.1111/jdi.12932.
Assar ME, Laosa O, Rodríguez Mañas L. Diabetes and frailty. Curr Opin Clin Nutr Metab Care. 2019; 22(1): 52–57. doi: https://doi.org/10.1097/mco.0000000000000535.
Dong BR, Gu XQ, Chen HY, et al. Correlation analysis of senile frailty and cardiovascular disease risk factors. Shanghai Medical. 2021; 42(12): 45–48,58. doi: https://doi.org/10.3969/j.issn.1006-1533.2021.12.013. [in Chinese]
Geladari E, Tsamadia P, Vallianou NG. ANGPTL3 Inhibitors- Their Role in Cardiovascular Disease Through Regulation of Lipid Metabolism. Circ J. 2019; 83(2): 267–273. doi: https://doi.org/10.1253/circj.CJ-18-0442.
Bastos-Barbosa RG, Ferriolli E, Coelho EB, et al. Association of frailty syndrome in the elderly with higher blood pressure and other cardiovascular risk factors. Am J Hypertens. 2012; 25(11): 1156–1161. doi: https://doi.org/10.1038/ajh.2012.99.
Hwang AC, Liu LK, Lee WJ, et al. Association of frailty and cardiometabolic risk among community-dwelling middle-aged and older people: results from the I-Lan longitudinal aging study. Rejuvenation Res. 2015; 18(6): 564–572. doi: https://doi.org/10.1089/rej.2015.1699.
Matsuoka M, Inoue T, Shinjo T, et al. Cardiovascular risk profile and frailty in Japanese outpatients: the Nambu Cohort Study. Hypertens Res. 2020; 43(8): 817–823. doi: https://doi.org/10.1038/s41440-020-0427-z.
Villani ER, Tummolo AM, Palmer K, et al. Frailty and atrial fibrillation: A systematic review. Eur J Intern Med. 2018; 56: 33–38. doi: https://doi.org/10.1016/j.ejim.2018.04.018.
Hung CY, Wu TJ, Wang KY, et al. Falls and atrial fibrillation in elderly patients. Acta Cardiol Sin. 2013; 29(5): 436–443. doi: https://doi.org/10.1016/j.numecd.2012.04.006.
Magnani JW, Wang N, Benjamin EJ, et al. Atrial fibrillation and declining physical performance in older adults: the health, aging, and body composition study. Circ Arrhythm Electrophysiol. 2016; 9(5): e003525. doi: https://doi.org/10.1161/CIRCEP.115.003525.
Hanlon P, Nicholl BI, Jani BD, et al. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493 737 UK Biobank participants. Lancet Public Health. 2018; 3(7): e323–e332. doi: https://doi.org/10.1016/S2468-2667(18)30091-4.
Xia HY, Cao Q, Zhou DD. Analysis on status quo and influencing factors of frailty in elderly patients with stroke. Shanghai Nursing. 2022; 22(1): 28–32. doi: https://doi.org/10.3969/j.issn.1009-8399.2022.01.007. [in Chinese]
Zhang L, Zhang XM. A Study on the relationship between asthenia and myopathy in patients with cerebral infarction. Hebei Medicine. 2021; 27(4): 659–664. doi: https://doi.org/10.3969/j.issn.1006-6233.2021.04.028. [in Chinese]
Funding
This study was supported by the National Nature Science Foundation of China (72274087, 71704071), The National Social Science Fund of China (20CGL053), The Fundamental Research Funds for the Central Universities (lzujbky -2020-10, lzujbky-2021-33), and The Natural Science Foundation of Gansu Province (22JR5RA218).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
This study did not include any animal or human experiments.
Additional information
Conflicting of interests
None authors have financial disclosures or conflicts of interest.
Rights and permissions
About this article
Cite this article
Huang, Y.N., Yan, F.H., Wang, X.Y. et al. Prevalence and Risk Factors of Frailty in Stroke Patients: A Meta-Analysis and Systematic Review. J Nutr Health Aging 27, 96–102 (2023). https://doi.org/10.1007/s12603-023-1879-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-023-1879-z