Abstract
The “Guidelines for Cadaver Dissection in Education and Research of Clinical Medicine” drafted by the Japan Surgical Society (JSS) and the Japanese Association of Anatomists in 2012 helped dispel legal concerns over cadaver surgical training (CST) and the usage of donated human bodies for research and development (R&D) in the country. Subsequently, in the fiscal year 2018, the Ministry of Health, Labour and Welfare increased the funding for CST, prompting its wider implementation. This study analyzed data obtained in 2012–2021 through the reporting system of the JSS-CST Promotion Committee to map the usage of cadavers for clinical purposes, specifically education and R&D, in Japan. We found that the number of medical universities using cadavers for CST and R&D programs was just 5 in 2012, and it reached 38 for the decade. Thus, about half of Japan’s medical universities implemented such programs over the period. Meanwhile, the total number of programs was 1,173. In the clinical field, the highest number of programs were implemented in orthopedics (27%), followed by surgery (21%), and neurosurgery (12%). Based on the purpose, the most common objective of the programs (approximately 70%) was acquiring advanced surgical techniques. Further, the highest number of programs and participants were recorded in 2019 (295 programs, 6,537 participants). Thus, the guidelines helped expand cadaver usage for clinical purposes in Japan. To further promote the clinical usage of cadavers in medical and dental universities throughout Japan, sharing know-how on operating cadaver laboratories and building understanding among the general public is recommended.
Similar content being viewed by others
Introduction
Since the Japan Surgical Society (JSS) and the Japanese Association of Anatomists (JAA) published the “Guidelines for Cadaver Dissection in Education and Research of Clinical Medicine” in 2012 (revised in 2018; JSS and JAA 2018), legal concerns regarding the implementation of cadaver surgical training (CST) and the usage of human bodies for research and development (R&D) have been resolved (Shichinohe and Kobayashi 2021). The path to the publication of the guidelines was as follows: In 1997, a workshop on dental implant procedures organized by a company in Japan invited intense media scrutiny over the use of imported cranial cadavers. Responding to the news reports, the former Ministry of Health and Welfare warned that improper CST implementation could result in corpse damage, which is considered a crime under the Penal Code of Japan. With this, CST became a legal “gray zone” and universities were forced to limit themselves to “clinical anatomy studies” performed under the supervision of their faculty of anatomy. Since CST was not established as a training program in Japan, a large number of surgeons attempting to learn new surgical techniques, such as endoscopic surgery, had to travel overseas for such training.
Gradually, growing demand for CST among surgeons seeking to advance their surgical skills became a critical issue. This led late professor Satoshi Kondo of Hokkaido University to conduct two studies, “Survey of Training Systems for Surgical Skills and Procedures” and “Study Group for Future Training Systems of Surgical Skills and Procedures” using grants from the Ministry of Health, Labour and Welfare (MHLW). These researches, that covered fiscal years (FY) 2008 to 2010, examined the status of several types of surgical training, including CST, in Japan and worldwide. In the final year of these researches, the “Draft of Guidelines for Cadaver Dissection in Education and Research of Clinical Medicine” was proposed to dispel the legal uncertainty over the implementation of CST. Based on this draft, the “Guidelines for Cadaver Dissection in Education and Research of Clinical Medicine” were published in 2012 by JSS and JAA.
The guidelines lay down some rules for CST and the clinical usage of cadavers for R&D, such as for developing novel surgical procedures and medical devices. They restrict the implementation of CST and R&D to the campuses of medical universities (including medical colleges and dental universities and colleges). They require centralized management of cadavers by the department of anatomy in each university. Registered donors need to be informed about CST and the clinical usage of cadavers for R&D, which differ from human body dissections performed at the undergraduate level. Written and advance consent needs to be obtained from the deceased prior to their death for the use of their body for CST and R&D. Further, consent must be obtained from their family as well. An expert committee needs to be established within a university to monitor the clinical usage of donated cadavers. As per the guidelines, the committee must coordinate each CST and R&D with the department of anatomy and review the protocols before submitting them to the ethics committee. The expert committee must summarize the contents of the implementation of the program, including the details of the training program, operating costs, and conflicts of interest (COI), and the summaries are required to be reported to the CST Promotion Committee (CST-PC) of JSS using the prescribed form. According to the guidelines, from a medical safety perspective, it is desirable that doctors who do not belong to the university can also participate in the CST program. In addition, as per the “Recommendations on the Usage of Cadavers in Clinical Research of Medicine,” published by the CST-PC of JSS in 2020 (JSS CST-PC, 2020), the usage of cadavers for R&D must comply with the "Ethical Guidelines for Medical and Biological Research Involving Human Subjects” published by the Japanese government as well as the “Guidelines for Cadaver Dissection in Education and Research of Clinical Medicine”.
From FY 2012, the MHLW started a competitive grant for covering CST expenses of universities under the “Training project for improving practical surgical procedural techniques”. Under the grant, approximately 45 million Japanese yen was provided every year to six universities located in each of six areal blocks in Japan. The aim was to promote CST and contribute to public welfare by improving medical safety (Kobayashi and Nudeshima 2018). Subsequently, in FY 2018, the ministry raised the annual grant for CST to approximately 300 million yen, out of which 200 million yen was meant for acquiring equipment and 100 million yen for covering the expenses of running CST programs of two universities in each of the six areal blocks. The grants continued into FY 2022. All these developments paved the way for more widespread adoption of CST and usage of cadavers in clinical research and medical device development.
This study is the first to analyze and quantify all CST and R&D programs reported to CST-PC of JSS in the decade since the 2012 guidelines were published.
Materials and methods
Reporting system for CST and data analysis
The 2012 guidelines require university committees to submit reports on each CST program to the CST-PC of JSS. In accordance with the CST-PC reporting system, reports of the programs implemented from April of the previous year to March of the current year must be submitted by July 15 of each year. The items that committees need to report are listed in Table 1. The CST-PC evaluates whether the implementation of the program is appropriate and recommends corrective action, if necessary. We analyzed reports registered in the reporting system between 2012 and 2021. The raw data for each item were further reclassified based on criteria discussed below and the analyzed data were represented by the median and the values of 25% and 75% percentiles were shown in the parentheses.
Year of implementation
For some programs that had multiple implementation dates spanning years, the year of implementation was set as the starting date of the implementation.
Names of universities and colleges
Even if multiple reports were registered by the university’s medical school and university hospital, or by different branches of medical centers of the same university hospital, they were all compiled under the name of the university.
Classification of clinical fields
The university departments and clinical units implementing CST or research were reclassified into surgery (such as gastroenterological, cardiovascular, respiratory, breast, and pediatric surgery), orthopedics, neurosurgery, otorhinolaryngology, urology, obstetrics and gynecology, plastic surgery, ophthalmology, dentistry and oral surgery, emergency and intensive care unit (ICU), anesthesiology, internal medicine, and clinical training center. The skills training for general intervention procedures conducted by clinical training centers was not reclassified in the clinical field and was described as it was.
Purpose of the programs
The purpose of cadaver usage was broadly categorized into two types: education/surgical training (E) and R&D (R). Category E was further subdivided into three categories based on the level of education: E-a, basic medical techniques such as tracheal intubation and chest tube insertion; E-b, standard surgical techniques and medical procedures in each field of surgery such as laparoscopic cholecystectomy and colectomy in gastrointestinal surgery; E-c, advanced surgical techniques and medical procedures such as robotic surgery in each field. Category R was also subdivided into three categories according to the purpose of R&D: R-a: research of clinical anatomy to further knowledge regarding accurate and safe operations; R-b: research and development of novel surgical procedures, for example development of a novel approaches to target organs based on anatomical rationality; R-c: research and development of medical devices such as developing a new surgical robot. Since multiple descriptions could be selected for each report, duplicate counts were allowed in the aggregation.
Number of cadavers used and preservation procedures
The number of cadavers was determined based on their total count. Since cadavers are usually used by multiple programs, it was difficult to determine the actual number of cadavers used over an entire study. Some programs reported multiple preservation procedures to embalm cadavers; therefore, duplicate counts were allowed in the tally. Further, descriptions of frozen, fresh and frozen, and unfixed cadavers were categorized as “unfixed.”
Number of participants and participation fee
Since 2019, when the electronic registration system was launched, participants with medical or dental license were categorized into “trainees” (hands-on training, observation practice), “trainers” or “lecturers,” “doctors in charge of management tasks,” and “supervision doctors from the faculty of anatomy.” The participants were further categorized based on their affiliation: “university,” “affiliate hospitals,” and “others.” For data registered up to FY 2018, participants were divided into “participants” and “observers” and their affiliation information was recorded. Further, for this analysis, all participants (medical and dental doctors) were counted and classified into two categories: on-campus and off-campus (including affiliated hospitals, by public offering, and others). In the records concerning the participation fee, some reports listed multiple participation fees, such as hands-on and observation fees. In the case of multiple participation fees, the highest fee was used for the analysis.
Program expenses
Since multiple trainings or research were conducted under some programs, the total expenditure per session was calculated by dividing the total expenses by the number of sessions.
Conflict of interest
For the analysis of each program, any financial support, provision of equipment, or labor by a company was described as a COI. The provision or rental of equipment, whether on payment or free of charge, was considered a COI because rental fees can be set arbitrarily by companies. Further, guidance from company staff on the proper use of equipment and the use of company staff for transporting the equipment for the program were regarded as a COI, regardless of whether any payment was made or not.
Ethical considerations
All programs conducted at the universities were approved by their respective ethical boards. In addition, anonymized data reported to the JSS, in accordance with the guidelines, were used for the current study.
Results
Number and names of universities implementing CST
When the 2012 guidelines were published, there were just 5 universities implementing CST. By 2019, their number increased to 31, and the total number further climbed to 38 by the end of the study period (Tables 2, 3). During the study period, 38 out of the 81 (47%) medical universities and colleges, 28 out of the 50 (56%) national and public universities, and 10 out of the 31 (32%) private universities and colleges submitted CST reports. No program was reported from dental colleges and universities.
Trend of program implementation, participation
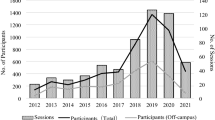
We recorded 1,200 reports on the system for 2012–2021. After excluding duplicate reports for resubmissions, the total number of programs was 1,173 (Fig. 1, Table 3). The data for programs and implementations in 2021 was from January to March 2021 in FY 2020. The number of sessions was different from the number of programs because some programs implemented multiple sessions. The total number of sessions was 2,677 (Table 3). In 71% of the programs, sessions of CST and other activities were reported as one-time implementations, while others reported repeat sessions up to 50 times by program. During the decade from 2012 to 2021, the highest number of programs (295) and sessions (504) were recorded in 2019 (Fig. 1, Table 3). The higher figure can be attributed to the expansion of MHLW funding for CST programs from FY 2018.
Annual trends in the number of programs and participants. The annual breakdown of the number of programs is shown in the line graph. The breakdown of the total number of participants and the number of off-campus participants by year are shown in the bar graphs. Total: Total number of medical and dental doctors. Off-campus: Number of participants who do not belong to a university, doctors belonging to affiliated hospitals, trainees through public offerings, and other doctors are included in this category
Following the COVID-19 pandemic and restrictions on social activities in Japan from April 2020, the number of participants in the FY 2020 showed a decline to 66% compared to 2019. The acceptance of off-campus participants also fell from 54 to 41%. Even under the impact of COVID-19, some CST implementation appeared to have continued since the risk of infection from cadavers is less likely. Most of the facilities have allegedly rejected the acceptance of dead bodies suspected to be infected with COVID-19, and some facilities introduced biological testing of COVID-19. Moreover, conducting CST in dissection rooms with well-ventilated environments and participants’ wearing full personal protective equipment minimized the risk of infection (Kobayashi and Schichinohe 2021).
Classification of clinical fields and program purpose
The number of programs classified by clinical fields is shown in Fig. 2. The highest number of programs were implemented in orthopedics, followed by surgery, neurosurgery, and otorhinolaryngology.
Number and percentage of programs classified by clinical fields. The programs are categorized into each clinical field based on the affiliation of the implementation representative. The percentages and number of program implementations for each category are shown in the figure. The percentage of each field is calculated by dividing the number of implementations by the total number of implementations (1,173). ICU intensive care unit
The aggregate data by purpose are described in Fig. 3. About 70% of the programs focused on surgical education. Whereas the usage of cadavers for the research and development of medical devices (R-c) was 5% (61), and only 19 programs (1.6%) were solely conducted for R-c.
Purpose of the programs. This figure shows aggregate data on the purpose of the programs, based on the reported description. Duplicate counts are allowed in the aggregation as multiple descriptions could be provided for each report. The purposes are broadly categorized into two categories: education of surgical training (E) and research and development (R&D: R). Subclassifications of category E: E-a: basic medical technique; E-b: standard surgical technique and medical procedures; E-c: advanced surgical technique and medical procedures. Subclassifications of category R: R-a: Research of clinical anatomy; R-b: Research and development of novel surgical procedures; R-c: Research and development of medical devices
Number of cadavers used and preservation procedures
In most cases, a single cadaver was used for multiple programs. Thus, the actual number of cadavers used throughout a program could not be determined. However, the total number of cadavers used was 4,492 (Table 3). For preserving the cadavers, some programs applied multiple procedures and aggregated 1,260 procedures for 1,173 implementations, with 844 fixed by the Thiel embalming method (Thiel 1992) (67%), 231 were unfixed (18.3%), 154 were fixed by formalin (12.2%), 26 were preserved by the saturated salt solution method (Coleman and Kogan 1998; Hayashi et al. 2014) (2.1%), and 5 were others and unspecified (0.3%) (Fig. 4). The main reasons for preferring the Thiel method are as follows: the condition of the organs is similar to that of unfixed cadavers, capable of simulating laparoscopic surgery; through formalin in the fixation solution, same as formalin-fixed cadavers, the cadavers can be preserved at room temperature, eliminating the risk of infection during the operative procedure.
Preservation procedure of the cadavers. Aggregated number of procedures in all reported programs. Some programs applied multiple preservation procedures and aggregated 1,260 for 1,173 implementations. The total implementation and trends in the top four clinical fields are shown in the graph. Frozen, fresh and frozen, and unfixed cadavers are categorized as “unfixed” Thiel Thiel embalming method, SSS saturated salt solution method
Only 7 out of the 38 (18%) universities that implemented CST provided unfixed cadavers. The preparation of an unfixed cadaver requires equipment (such as a freezer) and biohazard precautions. When we compared preservation procedures in the top four clinical fields, Thiel fixation was most frequent throughout; unfixed cadavers tended to be preferred in orthopedics, while formalin-fixed cadavers were in neurosurgery (Fig. 4). Of the 154 programs that used formalin for fixation, 58 pertained to neurosurgery and 24 to otorhinolaryngology. Formalin fixation tended to be selected in training in these surgical fields because of the excellent fixation of the brain. Meanwhile, the analysis of 231 programs using unfixed cadavers revealed that about half (111) were used in orthopedics, this supports the preference for unfixed cadavers seen in biomechanical research of orthopedics.
Number of participants and participation fee
The median number of participants in one session was 10 (5; 19), and the highest number of participants was 99 doctors, who took part in cadaver workshop on otorhinolaryngology that used five cadavers.
In terms of participation fee, 57% of programs (674) were free of charge, and the median fee was 0 yen (0; 20,000) (Fig. 5). When we analyzed the aggregated data for the 499 programs that charged a participation fee, the most frequent value was 10,000 yen (76), and the median fee was 25,000 yen (10,000; 50,000).
Participation fees for cadaver surgical training and other activities. Participation fees for cadaver surgery training and other activities have been classified by their value. If multiple participation fees are reported, the highest fee is adopted for the analysis. The median fee is 0 yen (0; 20,000)
Balance of the program, support, and COI
Thirty percent (352) of the programs were supported by the MHLW grant. In contrast, only 5.7% (67) were supported by a program co-organized with academic societies. When the expense per session was calculated, the median value was 153,180 yen (20,750; 470,240) (Fig. 6). There was no expenditure involved in 146 programs (12%). When COI was examined, 57% (670) of the programs showed COI. In the breakdown, 4.3% (51) of the programs acquired financial support, 48% (560) received provision of equipment, and 43% (503) received provision of labor (Fig. 7).
Discussion
Our data analysis showed that the implementation of CST and the clinical usage of cadavers for R&D in Japan has spread rapidly over the past decade. In particular, the increase in the MHLW grant in the FY 2018 can be considered a major factor in the increased adoption of CST given the rapid climb in CST program implementation in 2019. Between 2017 and 2019 (i.e., before and after the funding expansion, respectively), the number of universities implementing CST increased from 14 to 31, and the number of programs increased from 77 to 295. In addition, the number of sessions of CST and clinical usage of cadavers for R&D increased from 171 to 504, and the number of participants increased from 2,181 to 6,537.
Based on our data, the major issue that needs to be considered is that only less than half the universities have so far conducted CST and used cadavers for R&D. Given that there are departments of anatomy in each medical university, and there is a need for CST and R&D to develop the field of clinical medicine, it is necessary to create an environment for the implementation of CST in all medical universities.
The 2012 guidelines allow the implementation of CST not only in all medical schools, but also in all 29 dental schools in Japan. However, just 72 programs (6.1%) from 12 universities were reported in the field of dentistry and oral surgery from 2012 to 2021. Further, there were no CST reports from dental colleges. The data underlines the need to enhance the training environment given the need for CST in the field of dentistry.
The cost of CST is an important issue for the maintenance of a cadaver lab. In this statistical analysis, the median expense per program session was 153,180 yen. This expense included the cost of consumables, such as plastic gloves, gowns, drapes, and surgical equipment used in each session, and the fee for leasing medical devices, such as surgical endoscopes. In addition, other expenses, including teaching fees and transportation expenses for lecturers, were also included. As the style of CST varies according to the purpose of training, there is no “standard expense” for such programs; some can be performed with just scissors and scalpels, while others require the use of expensive medical equipment. Therefore, the expense varies depending on the content of the training, and setting a “standard expense” is difficult. However, in facilities implementing a large number of CST programs, the average expense per session can be deemed to be about 150,000 yen.
When we analyzed the participation fee, 57% of the programs were found to be offering the training free of charge. Meanwhile, there were 42 programs with participation fee of over 100,000 yen, and the top three among them covered orthopedics (11), neurosurgery (10), and otorhinolaryngology (7). Meanwhile, the median number of participants per session was 10 (5; 19), and only 31 programs (2.6%) had 50 or more participants. This shows that many facilities have just started CST with their peers in each department, and the development of large-scale CST programs with relatively high participation fees, such as overseas cadaver workshops, remains not to be well disseminated in Japan. In the future, it will be necessary to expand CST implementation facilities and integrate and share large-scale and public offering programs.
The limitation of this investigation is that the costs of purchasing, repairing, and storing equipment for conducting CST, and fees for using human resources, such as faculty members and technical staff of the department of anatomy, were not included as survey items. The survey included 12% of programs with zero expenses. This does not mean that their implementation involved no costs, but rather that universities bore the necessary expenses, including the cost of maintaining the donation system of human body. Future research could fill this gap by analyzing the essential expenses indispensable to the implementation of CST.
In conclusion, while the 2012 guidelines have helped boost CST and R&D involving the usage of cadavers, it is necessary to share the know-how on operating cadaver laboratories and gain the understanding and support of the general public to so that the programs cover all medical and dental colleges and universities in Japan.
References
Coleman R, Kogan I (1998) An improved low-formaldehyde embalming fluid to preserve cadavers for anatomy teaching. J Anat 192:443–446. https://doi.org/10.1046/j.1469-7580.1998.19230443.x
Hayashi S, Homma H, Naito M et al (2014) Saturated salt solution method: a useful cadaver embalming for surgical skills training. Medicine (baltimore) 93:e196. https://doi.org/10.1097/MD.0000000000000196
Kobayashi E, Nudeshima J (2018) Current state of surgical training using cadavers in Japan compared with Western countries. Surg Today 48:891–893. https://doi.org/10.1007/s00595-018-1673-4
Kobayashi E, Shichinohe T (2021) Suzuki T Cadaver surgical education and research under the SARS-CoV-2 pandemic in Japan. Otolaryngol Head Neck Surg. https://doi.org/10.1177/01945998211036422
Shichinohe T, Kobayashi E (2021) Cadaver surgical training in Japan: its past, present, and ideal future perspectives. Surg Today. https://doi.org/10.1007/s00595-021-02330-5
The CST-Promotion Committee of the Japan Surgical Society (2020) Recommendations on the usage of cadavers in clinical research of medicine (in Japanese). https://jp.jssoc.or.jp/uploads/files/aboutus/guidelines/cst20200929.pdf. Accessed Jan 2022
The Japan Surgical Society and the Japanese Association of Anatomists (2018) Guidelines for cadaver dissection in education and research of clinical medicine (in Japanese). https://www.jssoc.or.jp/journal/guideline/info20180406-01.pdf. Accessed Jan 2022
Thiel W (1992) Die Konservierung ganzer Leichen in natürlichen Farben [The preservation of the whole corpse with natural color] (in German). Ann Anat 174:185–195
Acknowledgements
The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. The results from such research can potentially increase mankind's overall knowledge, which can further improve patient care. Therefore, these donors and their families deserve our highest gratitude. We would like to express our gratitude to late Dr. Satoshi Kondo, who led the research to publish the guidelines discussed in the study, but passed away before their publication. We would also like to thank Dr. Takashi Kondo, Dr. Yoshiro Matsui, Dr. Chizuka Ide, Dr. Toshihiko Iwanaga, Dr. Yasuo Uchiyama, Dr. Akio Kikuta, Dr. Yutaka Nohara, Dr. Kazunari Yoshida, Dr. Toshio Terashima, Dr. Takanori Shibata, and Dr. Haruo Takahashi, who are former members of CST-PC, and their predecessors, the CST Guidelines Committee of the JSS. Finally, we are grateful to Mr. Uesawa and Mr. Kaneko and the members of the JSS office for supporting the activities of CST-PC and maintaining the reporting system.
Funding
Programs obtaining financial support from companies; Provision of Equipment: Programs receiving equipment from companies, whether on payment or free of charge; Provision of Labor: Programs receiving labor from companies, whether on payment or free of charge.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shichinohe, T., Date, H., Hirano, S. et al. Usage of cadavers in surgical training and research in Japan over the past decade. Anat Sci Int 97, 241–250 (2022). https://doi.org/10.1007/s12565-022-00659-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12565-022-00659-6