Abstract
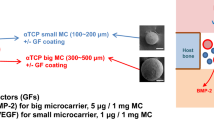
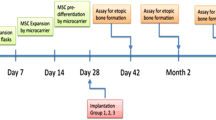
Bone tissue engineering combines biomaterials with biologically active factors and cells to hold promise for reconstructing craniofacial defects. In this study the biological activity of biphasic hydroxyapatite ceramics (HA; a bone substitute that is a mixture of hydroxyapatite and β-tricalcium phosphate in fixed ratios) was characterized (1) in vitro by assessing the growth of MC3T3 mouse osteoblast lineage cells, (2) in ovo by using the chick chorioallantoic membrane (CAM) assay and (3) in an in vivo pig animal model. Biocompatibility, bioactivity, bone formation and biomaterial degradation were detected microscopically and by radiology and histology. HA ceramics alone demonstrated great biocompatibility on the CAM as well as bioactivity by increased proliferation and alkaline phosphatase secretion of mouse osteoblasts. The in vivo implantation of HA ceramics with bone marrow mesenchymal stem cells (MMSCs) showed de novo intramembranous bone healing of critical-size bone defects in the right lateral side of pig mandibular bodies after 3 and 9 weeks post-implantation. Compared with the HA ceramics without MMSCs, the progress of bone formation was slower with less-developed features. This article highlights the clinical use of microporous biphasic HA ceramics despite the unusually shaped elongated micropores with a high length/width aspect ratio (up to 20) and absence of preferable macropores (>100 µm) in bone regenerative medicine.










Similar content being viewed by others
References
Abou Neel EA, Chrzanowski W, Salih VM, Kim HW, Knowles JC (2014) Tissue engineering in dentistry. J Dent 42:915–928
Ball M, Grant DM, Lo WJ, Schotchford CA (2008) The effect of different surface morphology and roughness on osteoblast-like cells. J Biomed Mater Res Part A 86:637–647
Barérre F, van Blitterswijk C, de Groot K (2006) Bone regeneration: molecular and cellular interactions with calcium phosphate ceramics. Int J Nanomed 1:317–332
Barradas AMC, Yuan H, van Blitterswijk CA, Habibovic P (2011) Osteoinductive biomaterials: current knowledge of properties, experimental modls and biological mechanisms. Eur Cell Mater 21:407–429
Biolusova G, Jun DH, King KB et al (2011) Osteoblasts derived from induced pluripotent stem cells form calcified structures in scaffolds both in vivo and in vitro. Stem Cells 29:206–216
Bradamante S, Barenghi L, Maier JAM (2014) Stem cells toward the future: the space challange. Life (Basel) 4:267–280
Campana V, Milano G, Pagano E et al (2014) Bone substitutes in orthopedic surgery: from basic science to clinical practice. J Mater Sci Mater Med 25:2445–2461
Chan O, Coathup MJ, Nesbitt A et al (2012) The effects of microporosity on osteoinduction of calcium phosphate bone graft substitute biomaterials. Acta Biomater 8:2788–2794
Cheng YH, Zhao GJ, Li SL (2000) Bone dinamics of repair of mandibular defect with collagen/hydroxyapatite. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 14:159–161
Ciocca L, De Crescenzio F, Fantini M, Scotti R (2009) CAD/CAM and rapid prototyped scaffold construction for bone regenerative medicine and surgical transfer of virtual planning:a pilot study. Comput Med Imaging Graph 33:58–62
Cordeiro-Spinetti E, de Mello W, Trindade LS, Taub DD, Taichman RS, Balduino A (2014) Human bone marrow mesenchymal progenitors: perspectives on an optimized in vitro manipulation. Front Cell Dev Biol. doi:10.3389/fcell.2014.00007
Danko J, Simon F (2012) Veterinary dictionary. Ikar, Bratislava
Danko J, Simon F, Artimova J (2011) Nomina anatomica veterinaria. University of Veterinary Medicine and Pharmacy, Kosice
Deligianni DD, Katsala ND, Koutsoukos PG, Missirlis YF (2001) Effect of surface rougness of hydroxyapatite on human bone marrow cell adhesion, proliferation and detachment strength. Biomaterials 22:87–96
D’Lima JP, Paul J, Palathingal P, Varma B, Bhat M, Mohanty M (2014) Histological and histometrical evaluation of two synthetic hydroxyapatite based biomaterials in the experimental periodontal defects in dogs. J Clin Diagn Res 8:52–55
Fellah BH, Gauthier O, Weiss P, Chappard D, Layrolle P (2008) Osteogenicity of biphasic calcium phosphate ceramics and bone autograft in a goat model. Biomaterials 29:1177–1188
Guo J, Meng Z, Chen G et al (2012) Restoration of critical-size defects in the rabbit mandible using porous nanohydroxyapatite-polyamide scaffolds. Tissue Eng Part A 18:1239–1252
Harvanova D, Hornak S, Amrichova J et al (2014) Isolation, cultivation and characterisation of pigeon osteoblasts seeded on xenogeneic demineralised cancellous bone scaffold for bone grafting. Vet Res Commun 38:221–228
Havlik RJ (2002) Hydroxyapatite. Plast Reconstr Surg 110:1176–1179
Herten M, Rothamel D, Schwarz F, Friesen K, Koegler G, Becker J (2009) Surface-and nonsurface-dependent in vitro effects of bone substitutes on cell viability. Clin Oral Invest 13:149–155
Jensen SS, Bornstein MM, Dard M, Bosshardt D, Buser D (2009) Comparative study of bisphasic calcium phosphates with different HA/TCP ratios in mandibular bone defects. A long-term histomorphometric study in minipigs. J Biomed Mater Res B Appl Biomater 90:171–181
Jiang H, Zuo Y, Zou Q et al (2013) Biomimetic spiral-cylindrical scaffold based on hybrid chitosan/cellulose/nanohydroxyapatite membrane for bone regeneration. ASC Appl Mater Interfaces 5:12036–12044
Jimi E, Hirata S, Osawa K, Terashita M, Kitamura C, Fukushima H (2012) The current and future therapies of bone regeneration to repair bone defects. Int J Dent. doi:10.1155/2012/148261
Keller JC, Collins JG, Niederauer GG, McGee TD (1997) In vitro attachment of osteoblast-like cells to osteoceramic materials. Dent Mater 13:62–68
Kirchhoff M, Lenz S, Henkel KO et al (2011) Lateral augmentation of the mandible in minipigs with a synthetic nanostructured hydroxyapatite block. J Biomed Mater Res B Appl Biomater 96:342–350
Kurashina K, Kurita H, Wu Q, Ohtsuka A, Kobayashi H (2002) Ectopic osteogenesis with biphasic ceramics of hydroxyapatite and tricalcium phosphate in rabbits. Biomaterials 23:407–412
LeGeros RZ (2002) Properties of osteoconductive biomaterials: calcium phosphates. Clin Orthop Relat Res 395:81–98
Lin FH, Liao CJ, Chen KS, Sun JS, Lin CP (2001) Petal-like apatite formed on the surface of tricalcium phosphate ceramic after soaking in distilled water. Biomaterials 22:2981–2992
Liu X, Wang X, Horii A (2012) In vivo studies on angiogenic activity of two designer self-assembling peptide scaffold hydrogels in the chicken embryo chorioallantoic membrane. Nanoscale 4:2720–2727
Lobo SE, Arinzeh TL (2010) Biphasic calcium phosphate ceramics for bone regeneration and tissue engineering applications. Materials 3:815–826
Mao JJ, Giannobile WV, Helms JA et al (2006) Craniofacial tissue engineering by stem cells. J Dent Res 85:966–979
Medvecky L, Giretova M, Stulajterova R (2012) Chemical modification of hydroxyapatite ceramic surface by calcium phosphate coatings and in vitro osteoblast response. Powder Metall Prog 12:224–233
Mello A, Hong Z, Rossi AM et al (2007) Osteoblast proliferation on hydroxyapatite thin coatings produced by right angle magnetron sputtering. Biomed Mater 2:67–77
Musumeci G, Castrogiovanni P, Leonardi R et al (2014) New perspectives for articular cartilage repair treatment through tissue engineering: a contemporary review. World J Orthop 5:80–88
Naujoks C, Langenbach F, Berr K et al (2011) Biocompatibility of osteogenic predifferentiated human cord blood stem cells with biomaterials and the influence of the biomaterial on the process of differentiation. J Biomater Appl 25:497–512
Noshi T, Yoshikawa T, Ikeuchi M et al (2000) Enhancement of the in vivo osteogenic potential of marrow/hydroxyapatite composites by bovine bone morphogenic protein. J Biomed Mater Res 52:621–630
Ong JL, Hoppe CA, Cardenas HL et al (1998) Osteoblast precursor cell activity on HA surfaces of different treatments. J Biomed Mat Res Part A 39:176–183
Pieri F, Lucarelli E, Corinaldesi G et al (2008) Mesenchymal stem cells and platelet-rich plasma enhance bone formation in sinus grafting: a histomorphometric study in minipigs. J Clin Periodontol 35:539–546
Rajzer I, Menaszek E, Kwiatkowski R, Chrzanowski W (2014) Bioactive nanocomposite PLDL/nano-hydroxyapatite electrospun membranes for bone tissue engineering. J Mater Sci Mater Med 25:1239–1247
Ribatti D, Nico B, Vacca A, Presta M (2006) The gelatin sponge-chorioallantoic membrane assay. Nat Protoc 1(1):85–91
Rumpel E, Wolf E, Kauschke E et al (2006) The biodegradation of hydroxyapatite bone graft substitues in vivo. Folia Morphol (Warsz) 65:43–48
Smith LA, Liu X, Hu J, Ma PX (2010) The enhancement of human embryonic stem cell osteogenic differentiation with nano-fibrous scaffolding. Biomaterials 31:5526–5535
Suzuki O, Nakamura M, Miyasaka Y, Kagayama M, Sakurai M (1991) Bone formation on synthetic precursors of hydroxyapatite. Tohoku J Exp Med 164:37–50
Tovar N, Jimbo R, Witek L et al (2014) The physicochemical characterization and in vivo response of micro/nanoporous bioactive ceramic particulate bone graft materials. Mater Sci Eng C Mater Biol Appl 43:472–480
Yoo JJ, Kim HJ, Seo SM, Oh KS (2014) Preparation of a hemiporous hydroxyapatite scaffold and evaluation as a cell-mediated bone substitute. Ceram Int 40:3079–3087
Yuann H, Kurashina K, de Bruijn JD, Li Y, de Groot K, Zhang X (1999) A preliminary study on osteoinduction of two kinds of calcium phosphate ceramics. Biomaterials 20:1799–1806
Yun JH, Han SH, Choi SH et al (2014) Effects of bone marrow-derived mesenchymal stem cells and platelet-rich plasma on bone regeneration for osseointegration of dental implants: preliminary study in canine three-wall intrabony defects. J Biomed Mater Res B Appl Biomater 102:1021–1030
Zhang Q, Lu H, Kawazoe N, Chen G (2013) Preparation of collagen scaffolds with controlled pore structures and improved mechanical property for cartilage tissue engineering. J Bioact Compat Polym 28:426–438
Zwadlo-Klarwasser G, Görlitz K, Hafemann B, Klee D, Klosterfalfen B (2001) The chorioallantoic membrane of the chick embryo as a simple model for the study of the angiogenic and inflammatory response to biomaterials. J Mater Sci Mater Med 12:195–199
Acknowledgments
This work was realized within the framework of the project ITMS no. 26220120066 “Centre of excellence for biomedical technologies,” which is supported by the Operational Program “Research and Development” financed through the European Regional Development Fund and within the project of the Ministry of Education VEGA no. 1/0046/16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Tomco, M., Petrovova, E., Giretova, M. et al. In vitro and in vivo study of microporous ceramics using MC3T3 cells, CAM assay and a pig animal model. Anat Sci Int 92, 569–580 (2017). https://doi.org/10.1007/s12565-016-0362-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12565-016-0362-x