Abstract
Introduction
To develop a simulation model assessing the efficiency of using cladribine tablets versus infusion-based disease-modifying drugs (DMDs) for the treatment of relapsing-remitting multiple sclerosis (RRMS) from a facility perspective in the UK.
Methods
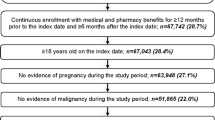
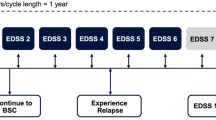
A scheduling algorithm was developed to simulate day-case admissions and calculate the mean changes to resource use and time burden for patients in a facility that transitions from infusion-based treatments to cladribine tablets over 1 year. Model inputs and assumptions were based on previous research and expert opinion. Model validation and quality checks were performed and additional scenario analyses were also conducted.
Results
The model successfully scheduled all infusion treatments in the base case and no patients were left off the schedule as a result of lack of capacity. Modeled base-case outcomes increased in future scenarios owing to a 35% increase in demand. The introduction of cladribine tablets reduced these impacts. Specifically, the difference in mean daily utilization was reduced in the future scenario from 13% to 3% as 8% of patients moved to cladribine tablets; annual administration costs decreased by 96% and annual time burden decreased by 90%. Results from additional scenarios showed the largest benefits from switching current infusion patients to cladribine tablets were realized in facilities having moderate to high resource utilization.
Conclusions
This model provides facility decision-makers the ability to assess the efficiency of using cladribine tablets rather than an infusion-based DMD. The simulation quantified the benefits gained from reducing the burden on facility resources by switching some patients with RRMS from infusion-based DMDs to cladribine tablets. Overall, modeled outcomes increased in future scenarios owing to an increase in demand, although the introduction of cladribine tablets reduced this impact.









Similar content being viewed by others
References
Lublin FD, et al. Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology. 2014;83(3):278–86.
Loma I, Heyman R. Multiple sclerosis: pathogenesis and treatment. Curr Neuropharmacol. 2011;9(3):409–16.
Thompson AJ, et al. Multiple sclerosis. Lancet. 2018;391(10130):1622–36.
Farber RS, Sand IK. Optimizing the initial choice and timing of therapy in relapsing-remitting multiple sclerosis. Ther Adv Neurol Disord. 2015;8(5):212–32.
Giovannoni G, et al. Brain health: time matters in multiple sclerosis. Mult Scler Relat Disord. 2016;9:S5–S48.
Johnson KM, et al. Real-world adherence and persistence to oral disease-modifying therapies in multiple sclerosis patients over 1 year. J Manag Care Spec Pharm. 2017;23(8):844–52.
Scolding N, et al. Association of British Neurologists: revised (2015) guidelines for prescribing disease-modifying treatments in multiple sclerosis. Pract Neurol. 2015;15(4):273–9.
Corbelli I, et al. Early management of patients with medication-overuse headache: results from a multicentre clinical study. Eur J Neurol. 2018;25(8):1027–33.
Andreou AP, et al. Prospective real-world analysis of OnabotulinumtoxinA in chronic migraine post-National Institute for Health and Care Excellence UK technology appraisal. Eur J Neurol. 2018;25(8):1069–e83.
McCool R, et al. Systematic review and network meta-analysis comparing ocrelizumab with other treatments for relapsing multiple sclerosis. Mult Scler Relat Disord. 2019;29:55–61.
Mullen KM. Challenges in having an infusion center. Rheum Dis Clin North Am. 2019;45(1):87–100.
Foley JF, Dunne AM. Successful management of a neurology infusion practice. Int J MS Care. 2011;13(2):95–104.
Leist TP, et al. Effect of oral cladribine on time to conversion to clinically definite multiple sclerosis in patients with a first demyelinating event (ORACLE MS): a phase 3 randomised trial. Lancet Neurol. 2014;13(3):257–67.
Giovannoni G, et al. A placebo-controlled trial of oral cladribine for relapsing multiple sclerosis. N Engl J Med. 2010;362(5):416–26.
Berardi A, et al. Estimating the comparative efficacy of cladribine tablets versus alternative disease modifying treatments in active relapsing-remitting multiple sclerosis: adjusting for patient characteristics using meta-regression and matching-adjusted indirect treatment comparison approaches. Curr Med Res Opin. 2019;35(8):1371–8.
Siddiqui MK, et al. Systematic literature review and network meta-analysis of cladribine tablets versus alternative disease-modifying treatments for relapsing–remitting multiple sclerosis. Curr Med Res Opin. 2017;34(8):1361–71.
Hettle R, Harty G, Wong SL. Cost-effectiveness of cladribine tablets, alemtuzumab, and natalizumab in the treatment of relapsing-remitting multiple sclerosis with high disease activity in England. J Med Econ. 2018;21(7):676–86.
Eagle T, et al. Treatment satisfaction across injectable, infusion, and oral disease-modifying therapies for multiple sclerosis. Mult Scler Relat Disord. 2017;18:196–201.
Jonker MF, et al. Summarizing patients’ preferences for the competitive landscape of multiple sclerosis treatment options. Med Decis Mak. 2020;40(2):198–211.
Rosenburg K. Split scheduling for chemotherapy increases efficiency, reduces costs. J Multidiscip Cancer Care. 2010;3(7):18–9.
Santibáñez P, et al. Operations research methods improve chemotherapy patient appointment scheduling. Jt Comm J Qual Patient Saf. 2012;38(12):541–53.
Alvarado MM, et al. Modeling and simulation of oncology clinic operations in discrete event system specification. Simulation. 2017;94(2):105–21.
Ahmed Z, Elmekkawy T, Bates S. Developing an efficient scheduling template of a chemotherapy treatment unit: a case study. Aust Med J. 2011;4(10):575–88.
Van Driel ML, et al. Learnings and challenges to deploy an interprofessional and independent medical education programme to a new audience. J Eur CME. 2017;6(1):1400857.
Kristoffersen ES, et al. Medication-overuse headache detoxification reduces headache disability—the Akershus study of chronic headache. Eur J Neurol. 2018;25(9):1140–7.
Chen ZY, et al. Altered brainstem volume in medication-overuse headache: a pilot magnetic resonance imaging evaluation. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2018;40(2):158–62.
De Cock E, et al. Monitoring burden of multiple sclerosis (MS) treatment in the UK: feasibility phase for an observations time and motion (T&M) study. Baltimore: ISPOR; 2018.
Athanasakis K, et al. Greek NHS capacity constraints regarding intravenous treatment for rheumatoid arthritis patients. Rheumatol Int. 2012;32(4):921–6.
Royal College of Physicians. Underfunded. Underdoctored. Overstretched. The NHS in 2016. London: Royal College of Physicians; 2016.
Acknowledgements
Funding
Financial support for this study and the Rapid Service Fee was provided by a contract between EMD Serono, Inc. a business of Merck KGaA, Darmstadt, Germany and Evidera.
Medical Writing and/or Editorial Assistance
The authors wish to thank Jason Allaire, PhD of Generativity Solutions Group for his assistance with editing the paper. This assistance was funded by EMD Serono, Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
AT: conducted research, analysis, manuscript development; AC: conducted research, analysis manuscript development; GH: conducted interpretation and manuscript development; JM: conducted interpretation and manuscript development; SLW: conducted interpretation and manuscript development.
Disclosures
Gerard Harty and Schiffon L. Wong are employees of EMD Serono, Inc. and hold stock in EMD Serono, Inc. Ali Tafazzoli, Ameya Chavan, and Jorgen Moller are employed by Evidera, a consultancy, who received funds from EMD Serono for developing this efficiency model.
Compliance with Ethics Guidelines
This article is not based on a study/studies that involved human participants or animals, performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12562604.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tafazzoli, A., Chavan, A., Harty, G. et al. Efficiency Model of Cladribine Tablets Versus Infusion-Based Disease-Modifying Drugs for Patients with Relapsing-Remitting Multiple Sclerosis. Adv Ther 37, 3791–3806 (2020). https://doi.org/10.1007/s12325-020-01426-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-020-01426-7