Abstract
In this study we analyse private medical insurance data with respect to civil servants in Germany. This data is applied to pricing purposes in the market and may therefore be deemed as useful. In particular, we discuss average health care expenditure per capita by age over time. Thereby, we analyse inpatient and outpatient benefits as well as hospital cash and dental insurance. In essence, we observe an effect that we call the rectangularisation of the cumulative health care expenditure curve. In line with this finding, we note that the modal age (at which total medical expenses for in force business are highest) has increased by 10 years of age over the last decade with respect to inpatient benefits. Moreover, we apply a linear regression model based on mortality rates as regressor. We use the Siegel test for comparing different expenditure profiles and judging goodness of fit. As a result, we find that steepening of private medical expenses by age over time is prevalent for three out of four benefit types in certain age bands. As for outpatient claims provided to male civil servants, medicalisation dominates the evolution of the average claim amount by attained age over time. On the other hand, compression is of relatively high importance for inpatient claims.
Zusammenfassung
Gegenstand dieser Studie sind aggregierte Daten der Privaten Krankenversicherung in Deutschland. Konkret untersuchen wir Zeitreihen von Kopfschäden nach Leistung, Geschlecht, Alter und Kalenderjahr. Insbesondere beobachten wir die sogenannte Quadratur der kumulativen Krankheitskosten im Verlauf des Lebens. Dabei zeigt sich, dass das modale Alter, indem die höchsten Krankenhauskosten für die Bevölkerung auftreten, im Verlauf der letzten Dekade um zehn Lebensjahr gestiegen ist. Außerdem modellieren wir die Krankheitskosten als Summe von Sterbekosten einerseits und Kosten zum Erhalt der Gesundheit andererseits. Mit Hilfe eines linearen Regressionsmodells und des Siegel-Tests zum Vergleich von Kopfschadenprofilen erhalten wir Einsichten in die Evolution der altersabhängigen Kopfschäden in der Zeit: Kopfschadenprofile wurden für gewisse Altersgruppen im Verlauf der Jahre nachweislich steiler. Außerdem entdecken wir einen dominierenden Medikalisierungseffekt im ambulanten Sektor und einen bedeutenden Kompressionseffekt im stationären Sektor.
Similar content being viewed by others
1 Introduction
Population ageing is prevalent in many countries around the world, see Lutz et al. (2008) for instance. There are two main reasons for ageing of society: longevity on the one hand and low fertility rates on the other hand. Oeppen and Vaupel (2002) elucidated the effect of rising longevity in the world: record life expectancy has increased by about one year of life every four calendar years.
As a consequence, there are serious implications for social welfare systems including national health services. Then, as people reach higher ages medical expenses per capita tend to increase. Some researchers argue this observation is caused by wear and tear of the human body. Others outline that proximity to death is the main driver. It still remains debatable which influencing factor, attained age or remaining life span, dominates medical spending over a person’s lifetime.
Fries (1980) established the so-called compression theory. The monetary version of this concept states that the bulk of medical expenses during the lifetime of a human being is due in the last years of life. In line with increasing longevity the majority of health care cost is shifted to higher ages. As such, the claims profile is stretched over a wider life span. Therefore, an ageing society does not necessarily imply increased spending for public health. The compression theory is consistent with the belief that in the future we may primarily enjoy a longer period of life in good health.
On the other hand, according to the monetary version of the medicalisation theory, Verbrugge (1984) stated that an ageing population implies increasing medical expenses for society. The reason being that higher attained ages imply greater morbidity. Hip replacements und cataracts, for instance, are common surgical procedures in German hospitals. These medical operations tend to be conducted for elderly people. Population ageing implies that higher age groups make up a larger share of the population. As a consequence, public spending for health care increases, too.
Zweifel et al. (1999) argued that the cost of dying is central to the understanding as to why total health care expenditure rises with age. The authors found out that health care expenditure per capita was much higher in the last quarter of life than in the preceding seven quarters. They concluded that proximity to death is the main driver for the rise of health care expenditure per capita by age. Then, at higher ages there are plenty of people who are close to death. Consequently, health care expenditure for the elderly is higher than for younger people. Taking increasing longevity into account the bulk of a person’s medical expenses is increasingly deferred to a later point in life. Hence, the curve of total health care expenditure per capita by age thus becomes flatter over time.
Seshamani and Gray (2004) replicated the above mentioned study. They concluded that both attained age and proximity to death explain the increase of health care expenditure per capita over time. In a subsequent study Zweifel et al. (2004) highlighted that attained age is significant for all those people who did not die soon afterwards. Wong et al. (2010) confirmed that both factors determine health care expenditure per head. According to these studies, proximity to death is the dominant factor in determining health care expenditure per capita by age over time.
In fact, medical spending aimed at preserving good health is deemed effective with respect to increasing longevity, see Becker et al. (2005) for instance. Ignoring this effect leads to overestimating the effect of proximity to death on total health care expenditure. Salas and Raftery (2001) pointed to the potential endogeneity of closeness to death. Felder et al. (2010) analysed endogeneity as a part of an empirical study. They concluded that the increase of health care expenditure is primarily caused by medical advances rather than population ageing.
Stearns and Norton (2004) pointed out that closeness to death is negatively correlated with both attained age and health care expenditure per capita. Yang et al. (2003) showed that time to death is the main reason for increasing inpatient care expenditures. Population ageing on the other hand causes long term care expenditure to increase. Notably, French et al. (2017) found out that medical spending in the last twelve months of life accounted for 8.5–11.2% of overall medical spending in different countries. All of this research shows that proximity to death must be considered when projecting total health care expenditure. Breyer and Felder (2006) calculated that per capita health expenditures of social health insurance would be overestimated when the cost of dying is ignored.
Getzen (1992) showed that total healthcare expenditure is correlated with gross domestic product. He deduced that the increase of health care expenditure over time may be mitigated by budget restrictions. Brockmann (2002) found out that the cost of dying decreases for the oldest old. This finding may indicate age related rationing. Busse et al. (2002) arrived at a similar finding when analysing days spent in hospital by age. Likewise, Niehaus (2006) showed that that the cost of dying is significant and decreases with age for the oldest. However, considering a fixed age band the cost of dying has increased over time due to medical inflation. Moreover, Niehaus disclosed that both, attained age and proximity to death, are significant drivers for health expenditure per capita. He concluded that medical inflation is the dominant cost driver.
In this paper, we analyse average medical claim amounts per capita by age over time. The subject of our research are civil servants in Germany from 2000 to 2019. In particular, we analyse inpatient and outpatient benefits as well as hospital cash cover and dental insurance. Our aim is to explore how average claims cost profiles changed over time. This research gives us some insights into the driving factors of the evolution of medical expenses by age over time.
To begin with, we discuss the secondary statistics of private medical data available to us. In the following section, we analyse average medical amounts per capita by age over time. Thereby, we distinguish between different benefits types. In Sect. 4 we compute total health care expenditure by age over time. In addition, we calculate cumulative distributions. In Sect. 5 we apply a linear regression model. It allows us to evaluate steepness and steepening of average medical claim amounts per capita over age bands rather than locally for specific ages. Finally, in Sect. 6, we decompose the evolution of private medical expenses per capita over time into two effects: compression and medicalisation.
2 Data
The German authority for financial supervision regularly publishes detailed statistics on private medical insurance business (BaFin 2021). This data is collected on a yearly basis from all insurance companies that are active in the German private health care market. In particular, BaFin provides figures on average medical claim amounts per capita by age, gender and benefit type for each calendar year. The data is presented in as so-called probability tables. In addition, there are mortality tables relating to the privately insured population as well as numbers of insureds exposed to risk.
It is worth highlighting that we analyse secondary data only. There may be changes over time in the way data was collected or summarised that are unkown to us since BaFin does not provide comprehensive documentation on this matter. In particular, the data comprises input from all insurance companies in the market. If some of these insurers or major players alter their data collection procedure the resulting effects might not be revealed to BaFin.
Notably, we do not adjust claim amounts as provided by BaFin for inflation. The reason being that we want to analyse the drivers of cost changes over time. We focus on data for insurance cover provided to civil servants as this is the main business for private medical insurance companies in Germany. In general, civil servants are not covered by the national health service—so-called sickness funds that are compulsory for most of the population. The state directly provides certain payments in case of sickness to its civil servants. The remainder of typically around 30–50% usually is covered by private medical insurance. Attention is given to inpatient benefits, outpatient benefits, hospital cash and dental insurance. Tables 1 and 2 highlight the number of persons exposed to risk within the aggregated market data.
As for the age profile of the in force business, we compare vital statistics in Germany with male and female civil servants who are private medically insured with respect to outpatient benefits. Figure 1 shows the distributions by age and sex applicable to calendar year 2014. Within our insured population, younger ages are underrepresented. On the other hand, the share of older ages is higher than in the general population of Germany.
3 Medical cost profiles over time
BaFin (2021) provides data on average claim amounts per head by age, benefit type and calendar year. We define ht(x) as the average claim amount per head during calendar year t for people aged x. Furthermore, we analyse relative changes in subsequent years: \(h_{t+1}\left(x\right)/h_{t}\left(x\right)-1\). For outpatient benefits over the period from 2000 to 2019 the average annual rate of increase has been above 2.5% per annum for all age groups (see Fig. 2).
Moreover, we visualise average claims cost profiles ht(x) by age x for certain calendar years t. Thereby, we plot the average claim amount per head on the vertical axis versus attained age on the horizontal axis. By so doing, we observe the change in claims profiles over time.
As for outpatient benefits, average claims amounts have significantly increased over time for all ages. In parts, this finding may be due to the fact that certain medical procedures have been more and more outsourced from hospitals into day clinics. Another reason for the year-to-year increase might be (medical) inflation.
Albeit not reported here in more detail, we would like to highlight a few more findings on the data: The age profiles for inpatient benefits have also increased over time albeit at a lower rate. We do not see a clear trend for the number of days spent in hospital over time. Note that there is a grace period of up to six weeks before hospital cash cover kicks in. The reason being that the state initially provides for ill people by continuing to pay salaries to its civil servants. As for people aged 60+, however, we note a pronounced increase in the number of days spent in hospital. Average claim amounts for dental cover have increased sharply between 1999 and 2019, in particular for older people. However, as for most ages we have more recently seen a slight decrease. This observation may be due to better dental hygiene that comes with a more widespread use of an electric toothbrush.
Figures 3 and 4 illustrate average claim amount profiles by age over time for different benefit types with respect to male insureds.
As for female insureds, we observe some peculiarities. With respect to inpatient benefits in 2019 we see a significantly different profile of average claim amounts compared to previous years. There is a hump for younger females suggesting that pregnancy benefits may be part of the reason that the profile is different from previous years when pregnancy benefits may have been reported separately. Hospital cash average claim amounts in 2019 are in line with those for males. Previous years in comparison seem to be too low. As we neither can fully explain nor correct these oddities within the secondary data set we primarily focus in the following on male insureds.
4 Total health care expenditure over time
The private medical insurance data provided by BaFin (2021) allows for computing total claim amounts by gender, age, benefit type and calendar year. To do so, we multiply the number of exposed to risk lx(t) at age x during calendar year t with the average claim amount per capita ht(x) in that year. Consequently, we derive total health care expenditure e(x,t):
As a result, we observe that the maximum of e(x,t) as a function of age for a given calendar year t has shifted to a higher age over time. To be specific, in 2009 approximately 50.8 million Euro were spent on inpatient claims for male civil servants aged 69. In 2019, the maximum was 82.5 million Euro for 79 year olds.
We define the modal age of health care expenditure M(t) in calendar year t as the age where expenditure is highest:
To sum up, the modal age of health care expenditure with respect to inpatient benefits has increased from age 69 in 2009 to age 79 in 2019 (see Fig. 5). This finding is in line with observations regarding the modal age at death that has also increased over time, see Kannisto (2001), Robine (2001) and Canudas-Romo (2010), for instance.
In conclusion, the evolution of total health care expenditure by age over time may be characterised in two ways. Over time, the maximum has shifted to the right and also upwards.
In order to identify the drivers of this development, we consider a constant average claim amount of 1000 € per head. It does not matter what amount we choose. Our findings hold likewise true for any other amount.
In essence, we assume that attained age has no impact on frequency and severity of medical claims. We then apply the constant claim profile to the number of exposed to risk for each calendar year, i.e., we set \(\tilde{e}\left(x{,}t\right)=l_{x}\left(t\right)\cdot 1000\). Fig. 6 elucidates the hypothetical total health care expenditure if we apply a constant average claim amount per head.
As for to expenditure with respect to inpatient benefits, the mode shifted 10 years of age during the last decade: from age 60 to age 70. Therefore, we have identified ageing of the in force business as the main driver for increasing the modal age of health care expenditure. Then the average claim amount is constant over age in this hypothetical modelling approach. On the other hand, the actual claims cost profile by age is responsible for shifting the maximum upwards.
As for outpatient benefits for male and female insureds alike the shift of the total expenditure curve is still visible but the change in the modal age is not as pronounced as can be seen in Fig. 7.
Finally, we define cumulative health care expenditure as
and plot it against time in Fig. 8.
Focussing on inpatient benefits we find some interesting insights. Total claims cost for males aged 65 and below made up 46% of total health care expenditure in 2009 but only 29% in 2019. Thus, medical claims for the part of the population that is potentially economically active, i.e. under the age of 65, made up a decreasing part of total health care expenditure.
Discussing the lower quartile, we find that 75% of medical expenses were attributable to males aged 57 and above in 2009. In 2019 three quarter of total health care expenditure referred to ages 64 and above. Hence, the vast majority of total private medical claims is paid to ever older people.
Let us assume that the trend of the historic evolution of the curve towards the lower right corner continues into the future. For most percentiles, we observe a horizontal shift to the right at the magnitude of about six years of life per decade. As a consequence, the median would increase from age 72 in 2019 to age 90 in 2049. I.e., in 2049 50% of all medical inpatient claims would be caused by peopled aged 90+. In 2019, on the other hand, the share of total inpatient medical expenses relating to ages 90 and above was 2.2% only.
The curve of cumulative health care expenditure remains rather flat for longer and longer. Then, at ever higher ages, cumulative expenses steeply rise to reach 100%. This finding with respect to private medical expenses is in line with observations fist made by Nusselder and Mackenbach (1996) in Dutch demographics concerning the so called rectangularisation of the survival curve: More and more people reach a very high age before most of them die relatively quickly.
There also is a clear trend towards a more rectangular shape of the health care expenditure curve. We call the effects described above and presented in Fig. 8 as the rectangularisation of the cumulative total health care expenditure curve. The finding remains valid for both sexes and outpatients benefits as Fig. 9 exhibits.
5 Steepness and steepening
We showed that the average claim amount per capita increases with age for all benefit types and most ages. In this section we analyse the slope as well as changes in the slope.
Buchner and Wasem (2006) defined steepness by analysing health expenditure in the dimensions of attained age and calendar year. A claims profile is supposed to become steeper if in two given calendar years if claims cost for older people increase more than for younger people. Felder et al. (2010) define steepness by the partial cross derivative of health care expenditure by age and calendar year. Gregersen (2014) found evidence of steepening when a applying a methodology in line with Felder et al. (2010). Similarly, Gregersen did not reject steepening for inpatient benefits in relation to the age group 50+ when applying the methodology of Buchner and Wasem (2006).
In general, the slope of the health care expenditure per capita curve must be defined locally by the slope of the tangent. As we are interested in broader age ranges, we fit a straight line to the health care expenditure curve by applying a linear regression model. As such, the slope of the approximated linear function is taken as the slope of the given health care expenditure curve. Our task then is to analyse changes in the slope over time with respect to a given age range.
Notably, we apply a linear approximation applicable to an age band instead of considering the tangent for each individual age. As such, or modelling approach still constitutes a local fit. We choose an appropriate age range and estimate goodness of fit.
For each benefit type we identify an age band where the linear approximation suitably covers a comparatively large age range. Obviously, our modelling approach is broadly valid albeit results for other age bands will be different. In this sense, the results presented in the following may be viewed for illustration purposes and proof of concept.
5.1 A linear model
We model average health care expenditure per capita h(x) by
Thereby, kqx is the probability that an x year old male dies with the next k years and the complement \(_{k}p_{x}=1-_{k}q_{x}\) is the probability that an x year old male survives the next k years. Equivalently, we find
In this modelling approach, f(x) is the medical cost of death and g(x) is the medical cost for survival. Alternatively, we may interpret g(x) as the base cost applicable to every insured person and \(\left(f(x)-g(x)\right)\) as the add-on cost of death. Furthermore, we assume that the estimated average claim amount is given by
In essence, we apply a linear model with kqx being the regressand and \(\hat{h}\left(x\right)=\hat{h}\left(_{k}q_{x}\right)\) being the regressor. In the following, we set \(k=2\) for illustration purposes and apply the regression for each calendar year \(t\in [2009;2019]\), i.e. to data for the last available decade.
5.2 The Siegel test
Siegel (2002) devised a statistical test to compare two claims cost profiles. Our aim is to judge whether the average medical claim cost profile by age \(h_{{t_{0}}}(x)\) for a given calendar year t0 and its estimator \(\hat{h}_{{t_{0}}}\left(x\right)\) deviate by chance. The statistical hypothesis H states that both profiles are the same for all ages.
According to Siegel (2002) it is necessary to normalise both profiles. Then, normalisation implies stochastic independence. Furthermore, we need to know volatility of claim amounts. As this information is lacking in BaFin (2021) data we rely on specific recommendations by Siegel (2002). Finally, Siegel showed that the test statistic is asymptotically distributed chi squared.
As for illustration purposes and proof of principle, we first consider outpatient benefits and restrict our analysis to values of 2qx between 0.009 and 0.0014. The associated age range is between 40 and 65 in 2019. As for inpatient benefits, we consider \(_{2}q_{x}\in [0.0025;0.0125]\) which relates to \(x\in [49;64]\) in 2019 The ranges for hospital cash cover are \(_{2}q_{x}\in [0.0009;0.009]\) and \(x\in [40;60]\) in 2019 respectively. Note that hospital cash cover is available to ages from 21–65 only. Finally, for dental insurance we set \(_{2}q_{x}\in [0.0027;0.0135]\) which implies \(x\in [50;65]\) in 2019.
The modelling results are as follows (Table 3).
To sum up, we selected suitable age ranges for each benefit type in such a way that the linear regression exercise results in a near perfect fit. Goodness of fit is proven by applying the Siegel test. Therefore, we may interpret the slope of estimated linear function as the slope of the curve for health care expenditure per capita with respect to the chosen age interval.
For illustration purposes we plot raw average claim amounts per head as well as estimated ones for inpatient benefits (see Fig. 10). It becomes clear that the approximation constitutes a local good fit.
5.3 The slope of the health care expenditure per capita curve
Based on the linear model above we analyse the slope of the estimated straight line in the given age interval for each benefit type and each calendar year. Results are summarised in Table 4.
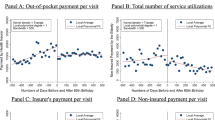
We define steepening as the slope getting bigger over time. Rather than considering the tangent for every age we use the estimated straight line over a given age range instead. In particular, we observe steepening of average private medical expenses per capita with respect to inpatient benefits, outpatient benefits and dental insurance. Steepening is most pronounced for dental insurance. Moreover, the change in the slope is bigger for inpatient benefits than for outpatient benefits. Finally, we observe flattening, i.e. the opposite of steepening, relating to hospital cash cover from 2009–2019.
For illustration purposes, we plot estimated average claim amounts per head relating to calendar years 2009 and 2019. Note that we have analysed goodness of fit in the previous section as per Table 3 and Fig. 10. We therefore omit the original health care expenditure curve in Fig. 11. In order to judge the slope and its changes over time we have to consider the estimated straight line instead.
6 The evolution of private medical expenses
Building on our linear regression model we want to better understand the evolution of average private medical claims per capita as plotted in Figs. 3 and 4. Our approach is motivated by physics.
Consider the gravitational force that acts on a car standing on a slope of a hill. The force can be additively decomposed into two forces. The first acts in parallel to the slope and makes the car move downhill. The latter is called adhesive force and keeps the car on the road. The sum of downhill force and adhesive force is the gravitational force.
Likewise, we assume that the change in average claim cost per head over time is caused by two effects: compression and medicalisation. The first stretches the profile and shifts the curve to the right. The latter moves the curve upwards.
Therefore, we decompose a given profile of average claim cost per head into two functions:
whereas we define
and
We call function ct(x) the compression effect. Compared with the estimated claims profile \(\hat{h}_{{t_{0}}}\left(x\right)\) in year t0 it causes a shift of this curve to the right. Then, the only difference is that we apply \(_{k}{q}_{x}^{t}\) instead of \(_{k}{q}_{x}^{t_{0}}\) when computing ct(x).
We call function mt(x) the medicalisation effect. It causes a shift of function ct(x) upwards. The sum of compression effect and medicalisation effect yields the estimated claims profile \(\hat{h}_{t}\left(x\right)\) in year t which can be easily verified.
For illustration purposes, we set \(t_{0}=2009\)and \(t=2019\) and consider outpatient benefits as well as inpatient benefits for the age group of 70–79 (see Fig. 12).
As a result, medicalisation is more pronounced with respect to outpatient benefits. As for inpatient benefits, medicalisation has a comparatively smaller impact on the evolution of health care expenditure per capita over time. Thus, compression is of higher relative importance with respect to inpatient cover while medicalisation dominates changes over time relating to outpatient cover.
7 Conclusion
In this article, we studied secondary statistics relating to private medical insurance in Germany. The data published by the German supervisory authority BaFin is used by insurance companies for pricing purposes and may therefore be deemed as a useful data source.
There are certain limitations to this study as we analysed secondary data only. Any change over time in producing these private medical insurance stats which are the basis for our analysis may not be known to BaFin and subsequently to us. Note that we analyse market data collected from all private medical insurance companies in the market. Any changes in data collections procedures may not be revealed to BaFin either. For instance, we observed a change in the average claims amount with respect to inpatient benefits for female insureds in 2019. As it is not possible for us to get to the bottom of these observations we primarily, but not exclusively, focussed on male civil servants. This part of the data makes up the bulk of private medical insurance business in Germany and does not exhibit any strange abnormalities.
A first descriptive analysis revealed that health care expenditure per capita rises with attained age, especially with respect to inpatient and outpatient benefits provided to older ages. As for outpatient benefits provide to male civil servants, for instance, annual rates of increase were more than two percent per year on average for almost all age groups.
We then shed light on the driving factors behind this development. It is a well known fact in demographics that the modal age of death at which most people die has significantly increased over time. Likewise, we found out that the modal age at which health care expenditure is highest has also increased. As for inpatient benefits for male civil servants the modal age has increased from age 69 in year 2009 to age 79 in year 2019, for instance. We found out that population ageing is the driving factor for this development.
In demographics the increase of the modal age of death over time is associated with an effect called the rectangularisation of the survival curve. More and more people reach a high age before dying relatively soon thereafter. We revealed an analogous effect that we call the rectangularisation of the health care expenditure curve. An ever larger share of total medical expenses is attributable to ever older people. A small part of total health care expenditure is sufficient to cover an increasingly large age band.
We then analysed the slope of the health care expenditure per capita curve by age over time. To broaden the scope, we applied a linear regression model based on mortality rates. In essence, we assume that health care expenditure per capita is given by the sum of the cost for maintaining good health as well as the cost of death. We proved goodness of fit by applying the Siegel test.
Notably, we observed rising average medical claim cost per head within the given age ranges for all benefit types. Thereby, we define steepness of the underlying health care expenditure curve by a positive slope of the estimated straight line. In particular, we note an increasing slope, called steepening, over time with respect to inpatient and outpatient benefits as well as dental cover. As for hospital cash cover, we found flattening of health care expenditure per capita by age over time.
Finally, we considered the evolution of claims cost profiles. To do so, we isolated two effects on the health care expenditure per capita curve over time: a shift to the right and a shift upwards. The former is called compression effect, the latter is called medicalisation effect. The compression effect takes the ageing effect within the population into account. Consequently, over time, the cost of death is referred to a higher age. The medicalisation effect on the other hand refers to the general effect of price trends on medical expenditure. Reasons may be medical inflation, advances in medical technology and increased take-up rates for certain procedures, to name but a few.
Comparing the effects, we found out that the compression effect is of relatively high importance with respect to inpatient benefits. The medicalisation effect dominates the evolution of health care expenditure with respect to outpatient cover. These two findings may be correlated by the fact that there is a trend to outsource certain medical procedures from hospitals into day clinics such as cataract surgeries.
As for future research we suggest validating our findings on primary statistics of private medical insurance companies or national health services respectively, possibly all over of the world. It would be very interesting to learn more about the evolution over time of heath care expenditure per capita in general and the impact of compression and medicalisation in particular in other countries. By so doing, we would gain a deeper understanding of the evolution of health care expenditure all in general as well as compression and medicalisation in particular. It would also be useful to analyse steepness and steeping more comprehensively for more age bands based on our concept of linear approximation. Last but not least, the insights gained in this study may be helpful with respect to projecting medical expenses into the future on a population level.
References
Becker, G.S., Philipson, T.J., Soares, R.R.: The quantity and quality of life and the evolution of world inequality. Am. Econ. Rev. 95(1), 277–291 (2005)
Breyer, F., Felder, S.: Life expectancy and health care expenditures: A new calculation for Germany using the costs of dying. Health Policy. 75(2), 178–186 (2006)
Brockmann, H.: Why is less money spent on health care for the elderly than for the rest of the population? Health care rationing in German hospitals. Soc. Sci. Med. 55(4), 593–608 (2002)
Buchner, F., Wasem, J.: “Steeping” of health expenditure profiles. Geneva Pap. Risk Insur. Pract. 31, 581–599 (2006)
Bundesanstalt für Finanzdienstleistungsaufsicht (BaFin): Wahrscheinlichkeitstafeln in der privaten Krankenversicherung (2021). https://www.bafin.de/DE/PublikationenDaten/Statistiken/PKV/wahrscheinlichkeitstafeln_artikel.html. Accessed 1 Oct 2010
Busse, R., Krauth, C., Schwartz, F.W.: Use of acute hospital beds does not increase as the population ages: results from a seven year cohort study in Germany. J Epidemiol Community Health 56(4), 289–293 (2002)
Canudas-Romo, V.: Three measures of longevity: time trends and record values. Demography 47(2), 299–312 (2010)
Felder, S., Werblow, A., Zweifel, P.: Do red herrings swim in circles? Controlling for the endogeneity of time to death. J Health Econ 29(2), 205–212 (2010)
French, E.B., et al.: End-of-life medical spending in last twelve months of life is lower than previously reported. Health Aff 36, 1211–1217 (2017)
Fries, J.F.: Aging, natural death, and the compression of morbidity. N Engl J Med 303, 130–135 (1980)
Getzen, T.: Population aging and the growth of health expenditures. J Gerontol 47, 98–104 (1992)
Gregersen, F.A.: The impact of ageing on health care expenditures: a study of steepening. Eur. J. Health Econ. 15, 979–989 (2014)
Kannisto, V.: Mode and dispersion of the length of life. Population 13, 159–171 (2001)
Lutz, W., Sanderson, W., Scherbov, S.: The coming acceleration of global population ageing. Nature 451(7179), 716–719 (2008)
Niehaus, F.: Auswirkungen des Alters auf die Gesundheitsausgaben. Wissenschaftliches Institut der PKV (2006)
Nusselder, W.J., Mackenbach, J.P.: Rectangularization of the survival curve in the Netherlands, 1950–1992. Gerontologist 36(6), 773–782 (1996)
Oeppen, J., Vaupel, J.W.: Broken limits to life expectancy. Science 296(5570), 1029–1031 (2002)
Robine, J.M.: Redefining the stages of the epidemiological transition by a study of the dispersion of life spans: the case of France. Population 13, 173–193 (2001)
Salas, C., Raftery, J.P.: Econometric issues in testing the age neutrality of health care expenditure. Health Econ. Lett. 10, 669–671 (2001)
Seshamani, M., Gray, A.: Ageing and health-care expenditure: the red herring argument revisited. Health Econ. 13, 303–314 (2004)
Siegel, G.: Signifikanztest für Kopfschadenprofile. Blätter der DGVFM., pp. 585–616 (2002)
Stearns, S.C., Norton, E.C.: Time to include time to death? The future of health care expenditure predictions. Health Econ. 13, 315–327 (2004)
Verbrugge, L.: Longer life but worsening health? Trends in health and mortality of middle-aged and older persons. Milbank Mem Fund Q Health Soc 62(3), 475–519 (1984)
Wong, A., van Baal, P.H.M., Boshuizen, H.C., Polder, J.J.: Exploring the influence of proximity to death on disease-specific hospital expenditures: a carpaccio of red herrings. Health Econ. 20(4), 379–400 (2010)
Yang, Z., Norton, E.C., Stearns, S.C.: Longevity and health care expenditures: the real reasons older people spend more. J Gerontol B Psychol Sci Soc Sci 58(1), 2–10 (2003)
Zweifel, P., Felder, S., Meiers, M.: Ageing of population and health care expenditure: a red herring? Health Econ. 8, 485–496 (1999)
Zweifel, P., Felder, S., Werblow, A.: Population ageing and health care expenditure: new evidence on the “red herring”. Geneva Pap. Risk Insur. Issues Pract. 29(4), 652–666 (2004)
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ortmann, K.M. The evolution of private medical expenses for civil servants in Germany. ZVersWiss 111, 515–533 (2022). https://doi.org/10.1007/s12297-022-00540-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12297-022-00540-5