Abstract
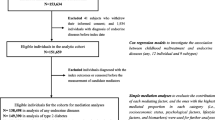
Research studies have identified associations between a range of social, familial and psychological risk factor and physical health. However, there are many methodological limitations in such studies (e.g. self-reported health status, retrospective recall of adverse events, and lack of control for possible heritability effects). The current study seeks to assess the effect of a range of social and psychosocial risk factors on a diagnosis of any endocrine, nutritional, and metabolic (ENM) disorders (ICD-10 E00–99) using linked Danish registry data from a large birth cohort. Data linkage. A national birth cohort of the Danish population born in 1984 was used in the current study (n = 54,458). Psychosocial risk factors including parental history of diagnosis of an ENM disorder, advanced parental age, gender, urban dwelling, economic deprivation, family dissolution and childhood adversity (child in care) were used to predict any ENM diagnosis. Bivariate associations showed that all variables, except advanced paternal age, were significantly associated with ENM diagnosis. When the variables were entered into a multivariate binary logistic regression analysis childhood adversity (child in care) was the strongest predictor of diagnosis (OR = 2.36) followed by maternal diagnosis of an endocrine disorder (OR = 1.74) and advanced maternal age (OR = 1.69). Results suggest that childhood adversity is the dominant factor in the prediction of an ENM diagnosis. The current study extends the literature conducted on adult populations by demonstrating that early adverse experiences are associated with poor or poorer health outcomes in young adulthood.
Similar content being viewed by others
Early adverse experiences, such as maladaptive family environments, low socioeconomic status, and childhood abuse have been associated with a variety of adult physical health outcomes (Felitti et al. 1998; Galobardes et al. 2006; Repetti et al. 2002). Similarly, markers for disease risk, such as inflammation and increased blood pressure, have been linked to adverse environments in childhood (Danese et al. 2007; Slopen et al. 2012). Empirical evidence suggests that early adverse experiences become ‘biologically embedded’ into multiple systems, altering brain function, neuroendocrine responses to stress, and the immune system (Shonkoff 2010; Shonkoff et al. 2009). Consequently, many adult endocrine, nutritional, and metabolic (ENM) disorders can originate during sensitive periods of development when biological systems are more vulnerable to physiological and environmental factors (Gonzalez 2013).
There is large body of literature examining the role of childhood adversity (e.g. neglect, sexual and physical abuse) on disorders related to the endocrine system such as type 1 and type 2 diabetes mellitus, obesity, and metabolic diseases (Joung et al. 2014; Thomas et al. 2008; Widom et al. 2012). A recent meta-analysis (Hemmingsson et al. 2014) reported significant positive associations between the severity of childhood abuse and adult obesity. In a prospective study of cases of childhood abuse and neglect, and matched controls, Widom et al. (2012) found that individuals who experienced childhood abuse and neglect were three times more likely to have developed diabetes. They also found specific types of abuse and neglect had shared and unique associations with endocrine conditions. Nygren et al. (2015) prospectively investigated the association between childhood stress and onset of type 1 diabetes in a large sample of Swedish participants. After controlling for potential confounding variables, including heredity of type 1 and type 2 diabetes and childhood BMI, it was reported that adverse life events increased the risk of onset of type 1 diabetes after the age of 13 by almost three times.
Familial risk-factors for ENM disorders include both environmental and heritable variables. Adolescents diagnosed with type 2 diabetes are more likely to belong to families that exhibit high-fat diets, binge-eating patterns, and low levels of physical exercise (Pinhas-Hamiel et al. 1999). Inconsistent evidence exists regarding the role of marital conflict, divorce, and separation in the prediction of ENM disorders with some findings suggesting a positive association (Troxel and Matthews 2004) and others suggesting no effect (Friedman et al. 2015; Thomas et al. 2008). Parental history of type 2 diabetes and obesity consistently increase the risk of both disorders among offspring (Lyssenko et al. 2008; Reilly et al. 2005). Vlachová et al. (2015) investigated metabolic risk-factors, prevalence of metabolic syndrome (MetS), and prediabetes in a Danish sample of adolescents with diabetic (type 1) mothers compared to a control group of adolescents of non-diabetic mothers. They reported that adolescents of diabetic mothers had a higher frequency of metabolic risk-factors, decreased insulin sensitivity, insufficient insulin secretion and a higher prevalence prediabetes compared to controls. Advanced parental age has also been examined as a risk-factor for type 1 (Harjutsalo et al. 2010) and type 2 (Köbberling and Tillil 1982) diabetes in offspring, however, research findings in this area remains equivocal. More consistent findings are reported for advanced maternal age with a recent meta-analysis indicating that maternal age over 35 at time of birth was associated with a 10% increase in offspring childhood type 1 diabetes risk compared to mothers aged 25 to 30 (Cardwell et al. 2010).
Adverse familial environments including economic deprivation have been associated with elevated concentrations of inflammatory markers, such as, C-reactive protein (CRP) and pro-inflammatory cytokines such as inter-leukin-6 (IL-6) among adults (Danese et al. 2007) and adolescents (Slopen et al. 2012). These inflammatory markers have additionally been associated with obesity, metabolic syndrome, and type 2 diabetes (Segman and Stein 2015; Stringhini et al. 2013), suggesting a potential biological pathway from childhood adversity to increased risk of ENM disorders. In addition to familial environment, the physical environment in terms of urbanicity may influence risk for ENM disorders. Results have been inconsistent with findings from a Finnish study demonstrating a higher prevalence of diabetes in rural environments (Rytkönen et al. 2003) and an Australian study demonstrating higher prevalence in urban environments (Haynes et al. 2006). Cultural variations in associated risk-factors with urban/rural dwelling likely exist which may serve to explain such inconsistent findings, however it is clear that greater research in this area is required.
Despite the proliferation of studies in the area of childhood adversity and ENM disorders there are many limitations. First, studies have tended to focus on a single risk factor in isolation without controlling for other correlated variables. For example, some studies focus on a narrow range of experiences (usually sexual and physical abuse) which limits knowledge on broader aspects of childhood adversity (Fergusson et al. 2013; Nikulina et al. 2011; Springer et al. 2007; Trickett et al. 2011). Second, most studies have used self-report measures of physical health outcomes which are subject to reporting biases that may lead to unreliable results and reduce the apparent magnitude of the relationship between child adversity and later health outcomes (Wegman and Stetler 2009). Third, retrospective designs are commonly employed. The use retrospective self-report measures in childhood maltreatment research has received a lot of criticism relating to the reliability and validity of these approaches given the lengthy period of recall, proportion of false negatives, mood-congruent recall biases, psychopathology and measurement error (Hardt and Rutter 2004; Widom et al. 2004). Fourth, few studies examining the relationship between environmental factors and ENM disorders have controlled for the heritability associated with ENM disorders.
The current study aimed to contribute to the existing literature by examining the effect of a broad range of psychological (childhood adversity), familial (advanced paternal age, family dissolution, parental ENM diseases), and environmental (urbanicity, deprivation) risk-factors in the prediction of subsequent ENM disorders. Whereas previous studies have tended to use specific, and generally self-reported, measures of childhood adversity this study used administrative records of being taken into care during childhood as a broad measure of childhood adversity. This population represents a high-risk sample as they are likely to have experienced a range of maltreatment experiences that resulted in their placement into care. The primary aim of this study therefore is to investigate risk-factors for any lifetime diagnosis of endocrine, nutritional, or metabolic disorders using a national birth cohort (N = 58, 489) of the Danish population born in 1984, and tracked over the course of the first 21 years of their life using the Danish registry system. The analyses aimed to first estimate the risk associated with each predictor in bivariate analyses, and secondly, how these risks changed when entered into a multivariate analysis to estimate the unique effect of each predictor while controlling for others. Investigating a number of previously reported risk-factors simultaneously will allow for a more complete understanding of the key psychosocial risk factors for the onset of these conditions.
Material and Methods
Data
This study used longitudinal data from a cohort of all children born in 1984 (N = 27,840 males and 26,618 females) in Denmark. They were followed from birth (1984) to early adulthood (2005). Parental data were linked with the participants’ data, with parental data being available from four years prior to the birth (1980) until 2005. A criterion for participation was that the children were resident in Denmark on 1 January 1998 at 14 years of age. Data from 365 (.6%) participants who were not alive at 2005 were excluded.
This study was based on the Danish Civil Registration System (CRS) and the Danish National Registry of Patients and was supported by the Institutional Review Board of University of Southern Denmark. A detailed description of the structure of CRS was provided by Pedersen et al. (2006) and Thygesen et al. (2011) provide details of the structure of different Danish health and social registers and how data can be accessed. Access to CRS data was through ‘Denmark Statbank’, which is the central government agency for statistics. In order to use CRS data researchers must apply to Denmark Statbank from an authorized institution. The research proposal needs to be approved by the Danish Register Data Board (‘Datatilsynet’), which is the agency responsible for all studies using register data, and by the Health Board (‘Sundhedsstyrelsen’), a department of the Danish Ministry of Health, which is the agency responsible for all studies involving public health data. On the basis of the research proposal Denmark Statbank make data available on the relevant variables to the researchers and variables are matched using the individual civil registry number (CPR). The CPR identifies people at the individual level and allows information to be collated across different registries. Identification of individuals is not possible as the 10 digit CPR numbers were scrambled prior to release.
Measures
The outcome variable was if a diagnosis of an ICD-10 endocrine, nutritional or metabolic disorder was recorded for the participant from birth (1984) until approximately 21 years of age (2005). Every time a person has contact with a hospital, emergency room, or outpatient clinic in Denmark they receive an ICD-10 diagnosis code that is recorded on the Danish National Registry of Patients. The diagnosis code is registered at the time of discharge by the physician discharging the patient. For this study we used the ICD-10 (E00–99), and previously ICD-8/9 codes, to identify any lifetime diagnosis of an ENM disease (E00-E07 Disorders of thyroid gland; E08-E13 Diabetes mellitus; E15-E16 Other disorders of glucose regulation and pancreatic internal secretion; E20-E35 Disorders of other endocrine glands; E36-E36 Intraoperative complications of endocrine system; E40-E46 Malnutrition; E50-E64 Other nutritional deficiencies; E65-E68 Overweight, obesity and other hyperalimentation; E70-E88 Metabolic disorders; E89-E89 Postprocedural endocrine and metabolic complications and disorders, not elsewhere classified). Similarly, parental data were used to identify maternal or paternal ENM diagnosis from 1980 to 2005. This information was linked to data from the CRS from which the other variables were derived.
Paternal and maternal age were coded as under or over 40 years at age at the time of offspring birth. Location was coded as urban if one lived in any of the cities (Aarhus, Odense, Aalborg, or Copenhagen) during their lives. Deprivation was defined as parental unemployment (for either one or both parents) with more than 21 days unemployment during a calendar year for any five or more years of the child’s first 18 years according to registers of Income Compensation Benefits, Labour Market research, and Unemployment Statistics. Denmark has very low levels of unemployment and these criteria were used to attempt that chronic unemployment, as opposed to temporary unemployment, was captured in the analysis. Maternal or paternal Endocrine Disorder was indicated if the participant’s mother or father received a diagnosis of an ENM condition (ICD-10 E00-E90) any time from 1980 to 2005. Family dissolution was defined as the child having experienced divorce, separation, and/or the death of a parent. Childhood adversity was indicated if the child was placed into care via the children’s act section or the child was not living with the parents but in an institution or foster home according to the population-based register of social assistance for children in care. Adversity was indicated by the child having been in care at any time during the first 10 years of the study (1984 to 1993). The child’s gender was also recorded.
Results
There were 2798 (4.8%) cases of lifetime ENM diagnosis in the cohort. Table 1 shows the bivariate associations between the risk-factors and an ENM diagnosis. All were statistically significant with the exception of advanced paternal age. The largest effects were observed for childhood adversity (‘child in care’), maternal diagnosis, and advanced maternal age. The weakest effects were advanced paternal age and gender (female).
Table 2 shows the estimates from the binary logistic regression models where all predictor variables were entered into the model with an ENM diagnosis as the dependent variable. The overall model was statistically significant (χ2(9) =391.20, p < .001). In this multivariate model advanced paternal age remained non-significant. All other variables remained statistically significant, and the strongest predictor of receiving an ENM diagnosis was childhood adversity (‘child in care’) (OR = 2.36).
Discussion
The current study utilised data from the Danish national registry to assess a range of important trauma related (childhood adversity), familial (advanced paternal age, family dissolution, parental ENM diseases), and environmental (urbanicity, deprivation) risk-factors for diagnosis of an ENM disorder. Results of the multivariate analysis showed that advanced paternal age was the only risk-factor that was a non-significant predictor. The measure of childhood adversity (child in care) was the strongest predictor increasing the likelihood of diagnosis by nearly two and a half times (OR = 2.36). This finding compliments a large literature base that has reported associations between childhood abuse and adult obesity (Danese and Tan 2014; Hemmingsson et al. 2014), HbA1C levels outside ‘acceptable range’ (Widom et al. 2012) and metabolic risk-factors (Danese et al. 2009).
A possible explanation of these findings is illustrated in a recent study by Joung et al. (2014) that demonstrated how childhood adversity can place stress on the endocrine system through the dysregulation of certain hormones (i.e. leptin, adiponectin and irisin) and the inflammatory marker C-reactive protein (CRP) all of which have been associated with obesity and diabetes in adulthood. Their findings indicated that higher levels of childhood adversity were associated with higher levels of these hormones, in particular leptin and irisin which remained significant even when controlling for demographic variables, physical activity and diet, current mental health status, and body mass index. Further support may be drawn from the growing research base demonstrating the links between posttraumatic stress disorder (PTSD) and the endocrine system. For example, Roberts et al. (2015) utilised data from a US longitudinal cohort of women (N = 49,739) to examine the association between PTSD symptoms and type II diabetes incidence over a 22-year follow-up period. PTSD symptoms were associated in a dose-response fashion with the onset of type II diabetes with approximately a 2-fold increased risk compared with non-traumatised women. Further, a review on the comorbidity of MetS and PTSD and found 38.7% of the PTSD population had MetS, and a two-fold increase in relative risk for MetS, compared to a control sample from the general population (Rosenbaum et al. 2015).
Familial factors such as advanced maternal age at birth and maternal ENM diagnosis were also strong predictors supporting previous findings (Bingley et al. 2000; Gale 2010; Lyssenko et al. 2008). A possible explanation for these findings is that research has demonstrated a link between advanced maternal age and the risk of gestational diabetes which has been found to be a predictor of increased long-term risks of type 2 diabetes, metabolic syndrome and increased cardiovascular disorders in mothers and abnormal glucose tolerance, obesity and metabolic syndrome in their offspring (Malcolm 2012). A UK study examined the association between maternal age and a wide range of adverse pregnancy outcomes (e.g. gestational diabetes mellitus and large for gestational age) and found that the incidence of gestational diabetes increases in mothers aged 35 and over. This finding remained even after adjusting for confounding factors associated with decreased insulin sensitivity such as ethnicity and obesity (Khalil et al. 2013).
Parental unemployment, which was used as a proxy for childhood socioeconomic status, was also found to be associated with diagnosis of an ENM disorder. There are numerous explanations as to why lower SES in childhood may increase susceptibility to ill-health; poor dietary intake/malnutrition, high fat diets, and lack of access to health care services (Cohen et al. 2013). Risk was also elevated due to a history of family dissolution (parental bereavement/ divorce/separation). These findings can be interpreted in light of a recent U.S. study using data from The National Health and Nutrition Examination Survey (NHNES) that reported children from single parent households were more likely to be overweight and have higher fat intake diets than children from dual parent households (Huffman et al. 2010).
Collectively, all risk-factors with the exception of advanced paternal age were associated with a diagnosis of an ENM disorder. The magnitude of these effects were small to moderate and may be reflective of the younger sample used in the current study in comparison to adult studies. Shonkoff et al. (2009) highlighted that early adverse experiences can affect adult health either through cumulative damage over time or the biological effects of adversity during sensitive developmental periods but that it may be several years or even decades before they manifest. In light of this, it is notable that given the developmental period in which this study is based, the current findings have important implications for the short term effects of adversity on ENM disorders in young adults.
The current study has notable strengths as the analyses were based on public record information on all Danish residents born in 1984. Diagnoses were therefore based on clinically recorded ICD-10 classifications rather than self-report measures which has been a limitation of the majority of research carried out in this area to date (Wegman and Stetler 2009). Additionally, by using national prospective cohort data from multiple administrative sources provides objective measures of a range of risk factors that may be associated with the later development of ENM disorders. Despite these strengths these findings should be interpreted in light of some limitations. First, the age range of the current cohort is likely to attenuate the associations between the risk variables and the outcome variables given that the available data recorded experiences up until the age of 21. It is therefore likely that a proportion of this cohort developed ENM disorders from 2005 onwards. Second, the current findings are limited to general ENM diagnoses and so inferences about specific diseases are not possible. Third, the analyses did not consider potential mediating variables such as health compromising behaviours such as alcohol/substance misuse which may be potential mechanisms underlying these associations. Indeed, the ‘child in care’ variable may be a proxy for some psychological variables that are associated with adolescent health; Resnick et al. (1997) reported that parent-family connectedness was a protective factor against health risk behaviours and children who have been placed in care are likely to have experienced low levels of family connectedness. Fourth, parental data was only available for a period of 4 years prior to the child’s birth, therefore parental risk factors preceding this time were not included which may have attenuated the findings reported in this study. Finally, caution may be required when interpreting public record data. It is possible that in some cases, for example, children who are taken into care are likely, due to state dependence, to encounter medical services and/or intervention in comparison than children raised in more traditional domestic settings which may have altered the strength of these associations.
In conclusion, using large population-based data on young adults in Denmark, this study provided evidence of a range of psychosocial markers of early adversity associated with conditions affecting the endocrine system in young adulthood. The findings of this study confirm that, at least up to the age of 21 years, psychosocial factors, in particular childhood adversity, are important factors along with familial/genetic risk-factors. Therefore, further research is warranted to explore the relationship of adverse childhood experiences on specific endocrine conditions in early adulthood in order to increase understanding of the dynamic interplay of these experiences and inform preventive treatment strategies.
References
Bingley, P. J., Douek, I. F., Rogers, C. A., & Gale, E. A. (2000). Influence of maternal age at delivery and birth order on risk of type 1 diabetes in childhood: prospective population based family study. BMJ, 321, 420–424.
Cardwell, C. R., Stene, L. C., Joner, G., Bulsara, M. K., Cinek, O., Rosenbauer, J., Ludvigsson, J., Jané, M., Svensson, J., Goldacre, M. J., Waldhoer, T., Jarosz-Chobot, P., Gimeno, S., Chuang, L. M., Parslow, R., Wadsworth, E., Chetwynd, A., Pozzilli, P., Brigis, G., Urbonaitė, B., Šipetić, S., Schober, E., Devoti, G., Ionescu-Tirgoviste, C., de Beaufort, C., Stoyanov, D., Buschard, K., & Patterson, C. (2010). Maternal age at birth and childhood type 1 diabetes: a pooled analysis of 30 observational studies. Diabetes, 59, 486–494.
Cohen, S., Janicki-Deverts, D., Turner, R. B., Marsland, A. L., Casselbrant, M. L., Li-Korotky, H. S., & Doyle, W. J. (2013). Childhood socioeconomic status, telomere length, and susceptibility to upper respiratory infection. Brain, Behavior, and Immunity, 34, 31–38.
Danese, A., & Tan, M. (2014). Childhood maltreatment and obesity: systematic review and meta-analysis. Molecular Psychiatry, 19, 544–554.
Danese, A., Pariante, C. M., Caspi, A., Taylor, A., & Poulton, R. (2007). Childhood maltreatment predicts adult inflammation in a life-course study. Proceedings of the National Academy of Sciences, 104, 1319–1324.
Danese, A., Moffitt, T. E., Harrington, H., Milne, B. J., Polanczyk, G., Pariante, C. M., Poulton, R., & Caspi, A. (2009). Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Archives of Pediatrics & Adolescent Medicine, 163, 1135–1143.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine, 14, 245–258.
Fergusson, D. M., McLeod, G. F., & Horwood, L. J. (2013). Childhood sexual abuse and adult developmental outcomes: findings from a 30-year longitudinal study in New Zealand. Child Abuse & Neglect, 37, 664–674.
Friedman, E. M., Karlamangla, A. S., Gruenewald, T. L., Koretz, B., & Seeman, T. E. (2015). Early life adversity and adult biological risk profiles. Psychosomatic Medicine, 77, 176–185.
Gale, E. A. M. (2010). Maternal age and diabetes in childhood. BMJ, 340, c623.
Galobardes, B., Smith, G. D., & Lynch, J. W. (2006). Systematic review of the influence of childhood socioeconomic circumstances on risk for cardiovascular disease in adulthood. Annals of Epidemiology, 16, 91–104.
Gonzalez, A. (2013). The impact of childhood maltreatment on biological systems: implications for clinical interventions. Paediatrics & Child Health, 18, 415–418.
Hardt, J., & Rutter, M. (2004). Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. Journal of Child Psychology and Psychiatry, 45, 260–273.
Harjutsalo, V., Lammi, N., Karvonen, M., & Groop, P. H. (2010). Age at onset of type 1 diabetes in parents and recurrence risk in offspring. Diabetes, 59, 210–214.
Haynes, A., Bulsara, M. K., Bower, C., Codde, J. P., Jones, T. W., & Davis, E. A. (2006). Independent effects of socioeconomic status and place of residence on the incidence of childhood type 1 diabetes in Western Australia. Pediatric Diabetes, 7, 94–100.
Hemmingsson, E., Johansson, K., & Reynisdottir, S. (2014). Effects of childhood abuse on adult obesity: a systematic review and meta-analysis. Obesity Reviews, 15, 882–893.
Huffman, F. G., Kanikireddy, S., & Patel, M. (2010). Parenthood—a contributing factor to childhood obesity. International Journal of Environmental Research and Public Health, 7, 2800–2810.
Joung, K. E., Park, K. H., Zaichenko, L., Sahin-Efe, A., Thakkar, B., Brinkoetter, M., Usher, N., Warner, D., Davis, C., Crowell, J., & Mantzoros, C. S. (2014). Early life adversity is associated with elevated levels of circulating leptin, irisin, and decreased levels of adiponectin in midlife adults. The Journal of Clinical Endocrinology and Metabolism, 99, E1055–E1060.
Khalil, A., Syngelaki, A., Maiz, N., Zinevich, Y., & Nicolaides, K. H. (2013). Maternal age and adverse pregnancy outcome: a cohort study. Ultrasound in Obstetrics and Gynecology, 42, 634–643.
Köbberling, J., & Tillil, H. (1982). Empirical risk figures for first degree relatives of non-insulin dependent diabetics. In J. Köbberling & R. Tattersall (Eds.), Serono symposium no. 47. The genetics of diabetes mellitus (pp. 201–209). London: Academic Press.
Lyssenko, V., Jonsson, A., Almgren, P., Pulizzi, N., Isomaa, B., Tuomi, T., Berglund, G., Altshuler, D., Nilsson, P., & Groop, L. (2008). Clinical risk factors, DNA variants, and the development of type 2 diabetes. The New England Journal of Medicine, 359, 2220–2232.
Malcolm, J. (2012). Through the looking glass: gestational diabetes as a predictor of maternal and offspring long-term health. Diabetes/Metabolism Research and Reviews, 28, 307–311.
Nikulina, V., Widom, C., & Czaja, S. (2011). The role of childhood neglect and childhood poverty in predicting mental health, academic achievement and crime in adulthood. American Journal of Community Psychology, 48, 309–321.
Nygren, M., Carstensen, J., Koch, F., Ludvigsson, J., & Frostell, A. (2015). Experience of a serious life event increases the risk for childhood type 1 diabetes: the ABIS population-based prospective cohort study. Diabetologia, 58, 1188–1197.
Pedersen, C. B., Gotzsche, H., Moller, J. O., & Mortensen, P. B. (2006). The Danish civil registration system. A cohort of eight million persons. Danish Medical Bulletin, 53, 441–449.
Pinhas-Hamiel, O., Standiford, D., Hamiel, D., Dolan, L. M., Cohen, R., & Zeitler, P. S. (1999). The Type 2 family: a setting for development and treatment of adolescent Type 2 diabetes mellitus. Archives of Pediatrics and Adolescent Medicine, 153, 1063–1067.
Reilly, J.J., Armstrong, J., Dorosty, A.R., Emmett, P.M., Ness, A., Rogers, I., Steer, C., Sherriff, A. (2005). Early life risk factors for obesity in childhood: cohort study. BMJ, 330. https://doi.org/10.1136/bmj.38470.670903.E0.
Repetti, R. L., Taylor, S. E., & Seeman, T. E. (2002). Risky families: family social environments and the mental and physical health of offspring. Psychological Bulletin, 128, 330–366.
Resnick, M., Bearman, P., Blum, R., Bauman, K. E., Harris, K. M., Jones, J., Tabor, J., Beuhring, T., Sieving, R., Shew, M., Ireland, M., Bearinger, L. H., & Udry, R. (1997). Protecting adolescents from harm. Findings from the National Longitudinal Study on Adolescent Health. JAMA, 278, 823–832.
Roberts, A. L., Agnew-Blais, J. C., Spiegelman, D., Kubzansky, L. D., Mason, S. M., Galea, S., Hu, F., Rich-Edwards, J., & Koenen, K. C. (2015). Posttraumatic stress disorder and incidence of type 2 diabetes mellitus in a sample of women: a 22-year longitudinal study. JAMA Psychiatry, 72, 203–210.
Rosenbaum, S., Stubbs, B., Ward, P. B., Steel, Z., Lederman, O., & Vancampfort, D. (2015). The prevalence and risk of metabolic syndrome and its components among people with posttraumatic stress disorder: a systematic review and meta-analysis. Metabolism. https://doi.org/10.1016/j.metabol.2015.04.009.
Rytkönen, M., Moltchanova, E., Ranta, J., Taskinen, O., Tuomilehto, J., & Karvonen, M. (2003). The incidence of type 1 diabetes among children in Finland—rural–urban difference. Health & Place, 9, 315–325.
Segman, R. H., & Stein, M. B. (2015). C-reactive protein: a stress diathesis marker at the crossroads of maladaptive behavioral and Cardiometabolic sequelae. The American Journal of Psychiatry, 172, 307–309.
Shonkoff, J. P. (2010). Building a new biodevelopmental framework to guide the future of early childhood policy. Child Development, 81, 357–367.
Shonkoff, J. P., Boyce, W. T., & McEwen, B. S. (2009). Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. Journal of the American Medical Association, 301, 2252–2259.
Slopen, N., Koenen, K. C., & Kubzansky, L. D. (2012). Childhood adversity and immune and inflammatory biomarkers associated with cardiovascular risk in youth: a systematic review. Brain, Behavior, and Immunity, 26, 239–250.
Springer, K. W., Sheridan, J., Kuo, D., & Carnes, M. (2007). Long-term physical and mental health consequences of childhood physical abuse: results from a large population-based sample of men and women. Child Abuse & Neglect, 31, 517–530.
Stringhini, S., Batty, G.D., Bovet, P., Shipley, M.J., Marmot, M.G., Kumari, M., Tabak, A., Kivimäki, M. (2013) Association of lifecourse socioeconomic status with chronic inflammation and type 2 diabetes risk: the Whitehall II prospective cohort study. PLoS Medicine, 10. https://doi.org/10.1371/journal.pmed.1001479.
Thomas, C., Hyppönen, E., & Power, C. (2008). Obesity and type 2 diabetes risk in midadult life: the role of childhood adversity. Pediatrics, 121, e1240–e1249.
Thygesen, L. C., Daasnes, C., Thaulow, I., & Brønnum-Hansen, H. (2011). Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scandinavian Journal of Public Health, 39, 12–16.
Trickett, P. K., Noll, J. G., & Putnam, F. W. (2011). The impact of sexual abuse on female development: lessons from a multigenerational, longitudinal research study. Development and Psychopathology, 23, 453–476.
Troxel, W. M., & Matthews, K. A. (2004). What are the costs of marital conflict and dissolution to children's physical health? Clinical Child and Family Psychology Review, 7, 29–57.
Vlachová, Z., Bytoft, B., Knorr, S., Clausen, T. D., Jensen, R. B., Mathiesen, E. R., & Jensen, D. M. (2015). Increased metabolic risk in adolescent offspring of mothers with type 1 diabetes: the EPICOM study. Diabetologia. https://doi.org/10.1007/s00125-015-3589-5.
Wegman, H. L., & Stetler, C. (2009). A meta-analytic review of the effects of childhood abuse on medical outcomes in adulthood. Psychosomatic Medicine, 71, 805–812.
Widom, C. S., Raphael, K. G., & DuMont, K. A. (2004). The case for prospective longitudinal studies in child maltreatment research: commentary on Dube, Williamson, Thompson, Felitti, and Anda (2004). Child Abuse & Neglect, 28, 715–722.
Widom, C. S., Czaja, S. J., Bentley, T., & Johnson, M. S. (2012). A prospective investigation of physical health outcomes in abused and neglected children: new findings from a 30-year follow-up. American Journal of Public Health, 102, 1135–1144.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
This project was approved by the Danish Register Data Board in Denmark. All data were stored and registers linked, at Statistics Denmark where individuals were anonymized. The researchers analysed anonymized individual level but report at an aggregate level.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Shevlin, M., Hyland, P., Elklit, A. et al. Social, Familial and Psychological Risk Factors for Endocrine, Nutritional and Metabolic Disorders in Childhood and Early Adulthood: a Birth Cohort Study Using the Danish Registry System. Curr Psychol 38, 1297–1303 (2019). https://doi.org/10.1007/s12144-017-9687-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-017-9687-4