Abstract
Background
There is some evidence that hyperglycemia increases the rate of poor outcomes in patients with intracerebral hemorrhage (ICH). We explored the relationship between various parameters of serum glucose concentrations measured during acute hospitalization and hematoma expansion, perihematomal edema, and three month outcome among subjects with ICH.
Methods
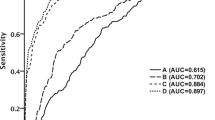
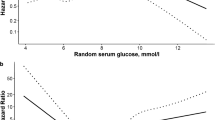
A post-hoc analysis of a multicenter prospective study recruiting subjects with ICH and elevated systolic blood pressure (SBP) ≥170 mmHg who presented within 6 h of symptom onset was performed. The serum glucose concentration was measured repeatedly up to 5 times over 3 days after admission and change over time was characterized using a summary statistic by fitting the linear regression model for each subject. The admission glucose, glucose change between admission and 24 hour glucose concentration, and estimated parameters (slope and intercept) were entered in the logistic regression model separately to predict the functional outcome as measured by modified Rankin scale (mRS) at 90 days (0–3 vs. 4–6); hematoma expansion at 24 h (≤33 vs. >33%); and relative perihematomal edema expansion at 24 h (≤40 vs. >40%).
Results
A total of 60 subjects were recruited (aged 62.0 ±15.1 years; 56.7% men). The mean of initial glucose concentration (±standard deviation) was 136.7 mg/dl (±58.1). Thirty-five out of 60 (58%) subjects had a declining glucose over time (negative slope). The risk of poor outcome (mRS 4–6) in those with increasing serum glucose levels was over two-fold relative to those who had declining serum glucose levels (RR = 2.64, 95% confidence interval [CI]: 1.03, 6.75). The RRs were 2.59 (95% CI: 1.27, 5.30) for hematoma expansion >33%; and 1.25 (95% CI: 0.73, 2.13) for relative edema expansion >40%.
Conclusions
Decline in serum glucose concentration correlated with reduction in proportion of subjects with hematoma expansion and poor clinical outcome. These results provide a justification for a randomized controlled clinical trial to evaluate the efficacy of aggressive serum glucose reduction in reducing death and disability among patients with ICH.
Similar content being viewed by others
References
Qureshi AI, Palesch YY. Antihypertensive Treatment of Acute Cerebral Hemorrhage (ATACH) II: design, methods, and rationale. Neurocrit Care. 2011.
Song E-C, Chu K, Jeong S-W, et al. Hyperglycemia exacerbates brain edema and perihematomal cell death after intracerebral hemorrhage. Stroke. 2003;34:2215–20.
Broderick JP, Diringer MN, Hill MD, et al. Determinants of intracerebral hemorrhage growth: an exploratory analysis. Stroke. 2007;38:1072–5.
Lee S-H, Kim BJ, Bae H-J, et al. Effects of glucose level on early and long-term mortality after intracerebral haemorrhage: the Acute Brain Bleeding Analysis Study. Diabetologia. 2010;53:429–34.
Adams HPJ, Adams RJ, Brott T, et al. Guidelines for the early management of patients with ischemic stroke: a scientific statement from the Stroke Council of the American Stroke Association. Stroke. 2003;34:1056–83.
Broderick J, Connolly S, Feldmann E, et al. Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Circulation. 2007;116:e391–413.
Meijering S, Corstjens AM, Tulleken JE, et al. Towards a feasible algorithm for tight glycaemic control in critically ill patients: a systematic review of the literature. Crit Care. 2006;10:R19.
Steiner T, Kaste M, Forsting M, et al. Recommendations for the management of intracranial haemorrhage—part I: spontaneous intracerebral haemorrhage. The European Stroke Initiative Writing Committee and the Writing Committee for the EUSI Executive Committee. Cerebrovasc Dis. 2006;22:294–316.
McCormick MT, Muir KW, Gray CS, Walters MR. Management of hyperglycemia in acute stroke: how, when, and for whom? Stroke. 2008;39:2177–85.
Qureshi AI. Antihypertensive Treatment of Acute Cerebral Hemorrhage (ATACH): rationale and design. Neurocrit Care. 2007;6:56–66.
Broderick JP, Adams HPJ, Barsan W, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 1999;30:905–15.
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–7.
Brott T, Broderick J, Kothari R, et al. Early hemorrhage growth in patients with intracerebral hemorrhage. Stroke. 1997;28:1–5.
McCarron MO, Hoffmann KL, DeLong DM, et al. Intracerebral hemorrhage outcome: apolipoprotein E genotype, hematoma, and edema volumes. Neurology. 1999;53:2176–9.
McCarron MO, McCarron P, Alberts MJ. Location characteristics of early perihaematomal oedema. J Neurol Neurosurg Psychiatry. 2006;77:378–80.
Zimmerman RD, Maldjian JA, Brun NC, Horvath B, Skolnick BE. Radiologic estimation of hematoma volume in intracerebral hemorrhage trial by CT scan. AJNR Am J Neuroradiol. 2006;27:666–70.
Qureshi AI, Bliwise DL, Bliwise NG, et al. Rate of 24-hour blood pressure decline and mortality after spontaneous intracerebral hemorrhage: a retrospective analysis with a random effects regression model. Crit Care Med. 1999;27:480–5.
Anderson CS, Huang Y, Wang JG, et al. Intensive blood pressure reduction in acute cerebral haemorrhage trial (INTERACT): a randomised pilot trial. Lancet Neurol. 2008;7:391–9.
Davis SM, Broderick J, Hennerici M, et al. Hematoma growth is a determinant of mortality and poor outcome after intracerebral hemorrhage. Neurology. 2006;66:1175–81.
Gebel JMJ, Jauch EC, Brott TG, et al. Natural history of perihematomal edema in patients with hyperacute spontaneous intracerebral hemorrhage. Stroke. 2002;33:2631–5.
Schettini A, Walsh EK. Contribution of brain distortion and displacement to CSF dynamics in experimental brain compression. Am J Physiol. 1991;260:R172–8.
Wilson JTL, Hareendran A, Grant M, et al. Improving the assessment of outcomes in stroke: use of a structured interview to assign grades on the modified Rankin Scale. Stroke. 2002;33:2243–6.
Wolfe CD, Taub NA, Woodrow EJ, Burney PG. Assessment of scales of disability and handicap for stroke patients. Stroke. 1991;22:1242–4.
Mayer SA, Brun NC, Begtrup K, et al. Recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2005;352:777–85.
Broderick JP, Brott TG, Tomsick T, Barsan W, Spilker J. Ultra-early evaluation of intracerebral hemorrhage. J Neurosurg. 1990;72:195–9.
Qureshi AI, Mendelow AD, Hanley DF. Intracerebral haemorrhage. Lancet. 2009;373:1632–44.
Concato J, Feinstein AR, Holford TR. The risk of determining risk with multivariable models. Ann Intern Med. 1993;118:201–10.
van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001;345:1359–67.
Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354:449–61.
Eslami S, de Keizer NF, de Jonge E, Schultz MJ, Abu-Hanna A. A systematic review on quality indicators for tight glycaemic control in critically ill patients: need for an unambiguous indicator reference subset. Crit Care. 2008;12:R139.
Fuentes B, Castillo J, San Jose B, et al. The prognostic value of capillary glucose levels in acute stroke: the GLycemia in Acute Stroke (GLIAS) study. Stroke. 2009;40:562–8.
Yong M, Kaste M. Dynamic of hyperglycemia as a predictor of stroke outcome in the ECASS-II trial. Stroke. 2008;39:2749–55.
Fogelholm R, Murros K, Rissanen A, Avikainen S. Admission blood glucose and short term survival in primary intracerebral haemorrhage: a population based study. J Neurol Neurosurg Psychiatry. 2005;76:349–53.
Passero S, Ciacci G, Ulivelli M. The influence of diabetes and hyperglycemia on clinical course after intracerebral hemorrhage. Neurology. 2003;61:1351–6.
Woo J, Lam CW, Kay R, et al. The influence of hyperglycemia and diabetes mellitus on immediate and 3-month morbidity and mortality after acute stroke. Arch Neurol. 1990;47:1174–7.
Weir CJ, Murray GD, Dyker AG, Lees KR. Is hyperglycaemia an independent predictor of poor outcome after acute stroke? Results of a long-term follow up study. BMJ. 1997;314:1303–6.
van Kooten F, Hoogerbrugge N, Naarding P, Koudstaal PJ. Hyperglycemia in the acute phase of stroke is not caused by stress. Stroke. 1993;24:1129–32.
Stead LG, Jain A, Bellolio MF, Odufuye A, Gilmore RM, Rabinstein A, et al. Emergency Department hyperglycemia as a predictor of early mortality and worse functional outcome after intracerebral hemorrhage. Neurocrit Care. 2010;13(1):67–74.
Ho CL, Ang CBT, Lee KK, Ng IHB. Effects of glycaemic control on cerebral neurochemistry in primary intracerebral haemorrhage. J Clin Neurosci. 2008;15:428–33.
Esposito K, Nappo F, Marfella R, et al. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress. Circulation. 2002;106:2067–72.
Godoy DA, Pinero GR, Svampa S, Papa F, Di Napoli M. Hyperglycemia and short-term outcome in patients with spontaneous intracerebral hemorrhage. Neurocrit Care. 2008;9:217–29.
Zubkov AY, Mandrekar JN, Claassen DO, et al. Predictors of outcome in warfarin-related intracerebral hemorrhage. Arch Neurol. 2008;65:1320–5.
Gray CS, Hildreth AJ, Sandercock PA, et al. Glucose-potassium-insulin infusions in the management of post-stroke hyperglycaemia: the UK Glucose Insulin in Stroke Trial (GIST-UK). Lancet Neurol. 2007;6:397–406.
Antihypertensive Treatment of Acute Cerebral Hemorrhage (ATACH) investigators. Antihypertensive treatment of acute cerebral hemorrhage. Crit Care Med. 2010;38(2):637–48.
Acknowledgments
The principal investigator, Dr. Qureshi had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Qureshi, A.I., Palesch, Y.Y., Martin, R. et al. Association of Serum Glucose Concentrations During Acute Hospitalization with Hematoma Expansion, Perihematomal Edema, and Three Month Outcome Among Patients with Intracerebral Hemorrhage. Neurocrit Care 15, 428–435 (2011). https://doi.org/10.1007/s12028-011-9541-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-011-9541-8