Abstract
Raynaud’s phenomenon and digital ulcers (DUs) are frequent among systemic sclerosis (SSc) patients. Our aim was to investigate the diagnostic and predictive value for DU of endothelial dysfunction biomarkers (flow-mediated dilatation (FMD), serum levels of endothelin-1 (ET-1), and ADMA), angiogenic/angiostatic biomarkers (vascular endothelial growth factor (VEGF), endoglin, and endostatin), and nailfold videocapillaroscopy (NVC). We compared our results with a literature review. In a cohort study of 77 SSc patients, we followed two groups of patients: (i) naïve DU patients (39) and (ii) active DU at baseline (38 patients) for 3 years. Telangiectasia (p < 0.001) and diffuse disease subset (p = 0.001) were significantly more frequent in patients with active DU at enrolment. Additionally, NVC late scleroderma pattern (AUC 0.846, 95%CI 0.760–0.932), lower values of FMD (AUC 0.754, 95%CI 0.643–0.864), increased serum levels of ET-1 (AUC 0.758, 95%CI 0.649–0.866), ADMA (AUC 0.634, 95%CI 0.511–0.757), and endoglin as well as low VEGF serum levels (AUC 0.705, 95%CI 0.579–0.830) were significantly associated to new DU events in the 3-year follow-up. Cox regression analysis showed that FMD > 9.41 % (HR 0.37, 95%CI 0.14–0.99); ET-1 >11.85 pmol/L (HR 3.81, 95%CI 1.41–10.26) and late NVC pattern (HR 2.29, 95%CI 0.97–5.38) were independent predictors of DU recurrence. When estimating the probability of occurrence of first DU in naïve DU patients, only late NVC pattern (HR 12.66, 95%CI 2.06–77.89) was an independent predictor factor. In conclusion, late scleroderma patterns in NVC are the best independent predictors of SSc patients who are at risk of developing DU. Endothelial dysfunction assessed by FMD and ET-1 was also found to be an independent predictor of DU recurrence in a 3-year follow-up.
Similar content being viewed by others
Introduction
Systemic sclerosis (SSc) is a severe autoimmune connective tissue disease that has at its core a triad of abnormalities: vasculopathy of small arterial vessels, elevated production of autoantibodies, and disjunction of fibroblasts with enhanced synthesis of extracellular matrix. The ethology and pathogenesis of SSc are still not completely understood. Important components of the clinical features of SSc are mainly derived from vascular damage [1]. Amongst them are endothelial dysfunction with abnormal vascular reactivity, hypoxia, insufficient neoangiogenesis, and oxidative stress with direct damage of vascular and perivascular cells. Vascular involvement plays a decisive role in early stages of the disease, with the first episodes of Raynaud’s phenomenon (RP) [2]. As a result of the progression of their severe vascular disease, up to 30–50 % of SSc patients will suffer from at least one ischemic digital ulcer (DU) [3, 4], and this type of lesion may become recurrent throughout the natural history of a SSc patient.
Vascular insufficiency resulting from progressive obliteration of both small arteries and microvessels in SSc is associated with a state of chronic tissue hypoxia [3]. Recurrent episodes of ischemia-reperfusion injury may contribute to tissue fibrosis, organ dysfunction, and significant morbidity and mortality in SSc patients. Currently, there are no biological measurements (biomarkers) to assess the subclinical vascular activity in patients with SSc, and therefore, the clinician is not able to detect disease until a late and irreversible stage [4].
The pathogenesis of DU is multifactorial and may differ with regard to DU localization. DUs may develop both on fingers or toes and can occur over the extensor surface of the joint, on the finger creases, under the nails, and in most cases, on the fingertips. Fingertip DUs are derived not only from the presence of the underlying vasculopathy but also from the persistent and repeated vasospasm bouts of the Raynaud phenomenon (RP) [5]. In contrast, DUs located on the dorsal side of the fingers are largely due to epidermal thinning and cutaneous retraction that lead to cracks on the skin overlying the joints [6]. DU may also develop from a preexisting calcinosis and sometimes from digital pitting scars [6]. DUs are painful, slow to heal, and are frequently complicated by secondary infections, with disabling effects, particularly regarding grip, feeding, dressing, and hand hygiene[7]. Severe DU episodes may necessitate hospitalization and require time away from the workplace [8].
Although new insights to management of DU have emerged, it is still challenging to identify patients at risk of developing DU episodes. Several reports have identified endothelial dysfunction and angiogenic vascular biomarkers, as well as capillaroscopic data, as potential parameters to predict new DU. However, these tools are expensive and difficult to be applied in routine clinical medicine. Even so, using these potential biomarkers of DU are pertinent to be performed, as the molecular analysis of the vascular mediators associated with SSc and its complications, peripheral microangiopathy in particular, may help in the early identification of patients at risk and in the search for new therapeutic that will prevent the progression of vascular injury in SSc patients.
The aim of the current study was to investigate the role of endothelial dysfunction, angiogenic factors, and microvascular abnormalities detected by nailfold videocapillaroscopy (NVC) as possible parameters to evaluate the risk of SSc patients to develop a first episode of DU or to have a recurrence of DU during a 3-year long follow-up period.
Materials and Methods
A prospective observational cohort study with a 3 years long clinical follow-up was conducted to evaluate 77 SSc patients, attending our Multidisciplinary Raynaud Clinics of the Clinical Immunology Unit at Centro Hospitalar do Porto in Portugal. We excluded from our study all patients with risk factors that could potentially interfere with flow-mediated dilatation (FMD): smokers, diabetics, with hyperlipidemia, and with past history of myocardial infarction, as well as patients on bosentan treatment, due to possible interference with endothelin-1 levels (ET-1). We had no patients lost during the entire course of our follow-up period.
All 77 included patients had SSc based on 2013 classification criteria for SSc of American College of Rheumatology [9]. Onset of the disease was defined as the time of first RP episode. All patients were on vasodilators calcium channel blockers (nifedipine) or angiotensin II receptor antagonist (losartan), and a washout of the vasodilator drugs was done before inclusion in the study. Thirty-four healthy, sex/age-matched, nonobese, without self-reported cardiovascular risk factors controls were invited to participate. No control subject was on any vasoactive medication.
SSc patients were divided into two groups: DU group that included 38 patients having an active ulcer at the beginning of our follow-up study, with or without a past history of DU (34 women; mean age 52.7 ± 14.8 years; range 14–75), and a group with no history of DU that included 39 patients with no history of DU until enrolment (38 women; mean age 53.2 ± 10.3 years; range 30–79).
The institutional ethical review board of Centro Hospitalar do Porto approved this study. All subjects signed informed consent before inclusion in the study. Data were collected by analysis of clinical file data and by clinical interview.
Definition of DU
Ischemic digital fingertip ulceration was defined as a painful area of 2 mm or greater in diameter, with visible depth and loss of dermis, amenable to healing and localized at a fingertip. DUs caused by conditions other than SSc were not considered.
Methods
Allen Test
Allen test was performed as follows: (1) instruct patient to clench his/her fist, (2) apply occlusive pressure to both ulnar and radial arteries by finger pressure, (3) confirm palm and finger blanching with the patient’s hand relaxed, (4) release the occlusive pressure on ulnar artery, and (5) positive test—if the hand flushes within 5–15 s, this indicates that the ulnar artery has good blood flow and palmar arch is complete—and negative test—if the hand does not flush within 5–15 s, this indicates that ulnar circulation is inadequate with an incomplete palmar arch.
FMD
Ultrasounds scans were performed using a two-dimensional ultrasonography General Electric Logic 7 with a 9-MHz Linear wideband multihertz imaging probe. Ultrasound images were recorded and analyzed for three consecutive end diastolic frames (onset of R wave) at 45 to 60 s after cuff deflation. The interoperator variability was 3.6 %.
Flow-mediated dilatation of the brachial artery in the lower arm was evaluated following International Brachial Artery Reactivity Task Force Guidelines [10] for the ultrasound assessment of brachial artery endothelial-dependent flow-mediated vasodilatation. Patients and controls (healthy subjects) were on overnight fasting for 12 h before the ultrasound study was performed. The exams were performed in the morning, with patients being kept in a quiet temperature-controlled room (22–24 °C) for a preliminary 20-min rest. Vasoactive drugs were withheld for ten half-lives. It was assured that patients did not exercise or ingest substances that could affect the response to ischemia like caffeine, vitamin C, tobacco, or high-fat foods for 24 h.
FMD was calculated as the percentage of change of the peak diameter in response to reactive hyperemia in (FMD% = (peak diameter − baseline diameter / baseline diameter) × 100) [10].
NVC
Nailfold Videocapillaroscopy was performed with KK technology Videocapillaroscopy with a ×200 magnification lens. In the end, all images were scored for each patient at the beginning of the follow-up study and 3 years later and were controlled by a capillaroscopy expert. The interoperator variability was 2.5 %.
Capillaroscopic findings were described following qualitative classification of scleroderma microangiopathy damaged described by Cutolo [11] in three patterns early, active, and late.
Autoantibody Detection
Antinuclear antibodies (ANA) were accessed by indirect immunofluorescence on Hep-2 cells (NOVAlite ANA, Inova Diagnostics, Inc., San Diego, CA, USA). Samples with a titer greater than or equal to 1:80 were considered positive. Autoantibodies anti-Scl-70, anti-centromere (ACA), anti-Ro52, anti-PM-Scl, anti-RNA-polymerase, anti-fibrillarin (AFA), and anti-NOR 90 were detected by immunoblotting using a Euroline Myositis Profile antibody test syst (Euroimmun, Lübeck, Germany). Quantification of anti-U1RNP and antibodies was carried out using a Fluoro Enzyme Immuno Assay (EliA™ U1RNP70; Phadia, Uppsala, Sweden).
Vascular Biomarkers
Venous blood samples from fasting individuals were collected into a serum tube and another tube containing sodium heparin (Vacuette, Greiner-Bio-One, Austria). Serum was allowed to clot at room temperature and then separated from cells within 60 min, and stored at −70 °C until analysis for asymmetric dimethylarginine (ADMA), endoglin, endostatin, and vascular endothelial growth factor (VEGF-A).
-
ET-1 assessment: Plasma was centrifuged immediately in a refrigerated centrifuge and stored at −70 °C until analysis for endothelin. Plasma endothelin was measured using a RIA assay (Euro-Diagnostics AG, Sweden). The resulting values are reported as picomole per milliliter.
-
ADMA assessment: Serum was allowed to clot at room temperature and then separated from cells within 60 min and stored at −70 °C before analysis for ADMA. Serum ADMA was measured using enzyme-linked immunosorbent assay (Immunodiagnostik AG, Germany). The resulting values are reported as micromole per liter.
-
VEGF assessment: Serum VEGF-A was measured using enzyme-linked immunosorbent assay (IBL International GMBH, Germany). The resulting values were reported as picogram per milliliter.
-
Endoglin and endostatin assessment: Serum endoglin and endostatin were measured using enzyme-linked immunosorbent assay (Uscn, Life Science Inc., Wuhan). The resulting values were reported as nanogram per milliliter.
Follow-up
When included in the study cohort, patients were followed for 3 years. Patients were instructed to come to the hospital clinics whenever a new digital tropic lesion occurred. If no DU developed, patients were seen on a regular basis at 3–6-month intervals, as indicated by disease severity.
Major Clinical Outcomes
Our primary outcome was the occurrence of at least one new ischemic fingertip DU in the 3-year clinical follow-up period. In addition, we applied survival analysis to investigate freedom from DU recurrence in the study period, regarding (i) endothelium dysfunction (FMD, ET-1 and ADMA), (ii) microvascular abnormalities in qualitative scleroderma pattern NVC, and (iii) angiogenic VEGF/angiostatic (endostatin, endoglin) factors.
Statistical Analysis
For comparison of normally distributed scale variables, we used unpaired two-sided Student’s t test or analysis of variance (ANOVA). In these cases, data were described by mean ± standard deviation (SD) followed by the minimal and the maximal values (range). Normal distribution was tested by Q–Q plots. In the cases of nonnormally distributed variables, we used nonparametric tests: Mann–Whitney and Kruskal–Wallis tests and data were described by median followed by the interquartile interval (Q 1–Q 3), where Q 1 represents the first quartile (corresponding to 25 % of data) and Q 3 represents the third quartile (corresponding to 75 % of data). In ANOVA test, when the homogeneity of variance was not satisfied, we used the Welch test. For comparison of categorical variables, we used chi-square or Fisher’s exact probability test. We applied survival analysis to determine the probability of freedom from new DU during the study period and evaluated the effects of FMD, ET-1, ADMA, VEGF, endostatin, endoglin, and NVC scleroderma patterns in that probability using the Kaplan–Meier method and the Cox regression. To evaluate the predictive effect of these variables, we considered them as categorical variables, and associations were assessed according to the median value of each variable. The association between initial characteristics and the DU reoccurrence or new DU event was first analyzed in univariate Cox regression followed by multivariate Cox regression including all variables with p < 0.2 in univariate analysis. A receiver operating characteristic (ROC) curve analysis was performed to obtain the predictive accuracy of FMD, MES score, ET-1, ADMA, VEGF, endostatin, and endoglin. We considered p values <0.05 as significant. Data were analyzed using the SPSS software (v.22.0, SPSS, Chicago, IL).
Results
Study Population
The mean age of the 77 SSc patients (72 women, 93.5 %) was 52.95 ± 12.65 years, and the median disease duration was 10.00 years (6.00–20.5) (Table 1). At enrolment, two subpopulations were distinguished among these 77 SSc patients: (i) with active DU and (ii) with no history of DU. Active DU was present in 38 patients, with or without a past history of DU (34 women; mean age 52.7 ± 14.8 years; range 14–75), and 39 of the SSc patients had no history of DU (38 women; mean age 53.2 ± 10.3 years; range 30–79). The median time for the first DU occurrence was 4.00 years (2.02–11.75) since disease onset.
Clinical features such as telangiectasia (p < 0.001), sclerodactily (p < 0.001), calcinosis (p < 0.001), digital pitting scars (p = 0.001), and positive Allen test (p < 0.001) were significantly more frequent in patients in the subpopulation of SSc patients with active DU. Additionally, diffuse disease subset (p = 0.001), NVC scleroderma pattern (p < 0.001), lower values of FMD (p < 0.001), increased serum levels of ET-1 (p < 0.001), ADMA (p = 0.049), and endoglin(p = 0.017) as well as low VEGF serum levels (p = 0.009) were significantly associated to active DU. No significant differences were found concerning age, gender, disease duration (p = 0.0602) or in angiostatic biomarker endostatin (p = 0.129) (Table 2).
ROC analysis was performed in order to define the serum levels that were the best predictors for new DU events (Table 3). Positive diagnostic value of the different parameters studied as potential risk factors for DU events reflected by an area under the curve: ET-1 (AUC 0.758, 95%CI 0.649–0.866), FMD (AUC 0.754, 95%CI 0.643–0.864), VEGF (AUC 0.705, 95%CI 0.579–0.830), ADMA (AUC 0.634, 95%CI 0.511–0.757), endoglin (AUC 0.606, 95%CI 0.480–0.733) and endostatin (AUC 0.591, 95%CI 0.463–0.720), and for NVC scleroderma pattern (AUC 0.846, 95%CI 0.760–0.932).
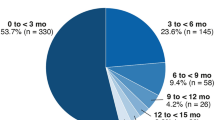
Primary Outcome: New Ischemic Digital Ulcer Episode in 3-Year Follow-up
During the 3-year clinical follow-up of this study, 40 of the 77 SSc patients (51.9 %) developed at least one new ischemic fingertip. Most of these 40 patients (30, i.e., 75 %) belonged to the subpopulation with active DU at enrolment. The median time of occurrence of these new DU was 4.5 months (1.25–16.25), which is significantly shorter than the data available at the Eustar registry [12] (Table 4). Also, patients with active DU at enrolment had a more severe progression of their capillaroscopic patterns (p < 0.001) when initial and final (3 years) results were compared (Supplementary Table 1).
Reccurence of DU
Of the 38 SSc patients with active DU at beginning of the study, 30 of them (79 %) had DU recurrence during the 3-year course of this investigation (Table 4). By the use of univariate Cox regression analysis, we were able to identify the following predictor factors of DU recurrence: FMD > 9.41 % (HR 0.37, 95%CI 0.14–0.99), ET-1 > 11.85 pmol/L (HR 3.81, 95%CI 1.41–10.26), and late NVC pattern (HR 2.29, 95%CI 0.97–5.38) (Supplementary Table 2). Kaplan–Meyer analyses of freedom from the DU recurrence showed that the median values of FMD (p = 0.035), ET-1 (p = 0.004), and qualitative scleroderma NVC (p = 0.047) were significantly associated with the new episodes of DU (Fig. 1a–c). Multivariate Cox regression confirmed ET-1 (HR 4.23, 95%CI 1.51–11.83) and late NVC pattern (HR 2.49, 95%CI 1.03–6.04) as independent predictors of DU recurrence (Supplementary Table 3).
a-d Kaplan–Meier analyses of freedom from new digital ulcers in 36 months follow-up of 77 SSc patients. Recurrence DU: curves A–C are shown for a patients who had FMD levels ≤9.41 % or >9.41 % (p = 0.035), b patients who had ET-1 serum levels ≤11.85 pmol/ml or >than 11.85 pmol/ml (p = 0.004), and c patients who had active/late scleroderma pattern (p = 0.047). Naïve DU patients: curve d shows freedom of digital ulcers at any time of the disease course/patients who had early/active/late pattern (p < 0.001). FMD flow-mediated dilatation, ET-1 endothelin-1, NVC nailfold videocapillaroscopy
First DU Event in SSc Patients with No History of DU
We have also searched for predictive factors for the first DU event among the patients with no history of DU at enrollment in this study (Table 4). From univariate analysis, we are able to conclude that only late NVC pattern (HR 12.66, 95%CI 2.06–77.89) is an independent predictor for a first DU event. Kaplan–Meyer analyses of freedom from the occurrence a DU event at any time of disease course strengthen the results of Cox analysis with NVC qualitative late scleroderma pattern (p < 0.001) as a significant factor (Fig. 1d). Multivariate Cox regression confirmed late NVC (HR 13.38, 95%CI 2.10–85.38) as an independent predictor of the first DU (Supplementary Table 4).
SSc Patients with No DU at Enrolment and in the 3-Year Follow-up
Median SSc duration in patients with no previous history of DU was 10.00 years (5.25–22.5) with no significant differences in comparison with disease duration in the subpopulation of SSc patients with DU. These naïve DU SSc patients were largely lcSSc (96.6 %; p = 0.025) and anti-scleroderma 70 negative (p = 0.036). They also presented less peripheral vascular impairment, as evidenced by encompassing a smaller number of patient with telangiectasia (p = 0.007) and the predominance of negative Allen test (p < 0.001); this was strengthened by a good response to shear stress FMD% (p < 0.001). They exhibited lower serum levels of vasoconstrictive ET-1 (p < 0.001), and increased ADMA (p = 0.049) and VEGF (p = 0.003) serum levels. Late scleroderma pattern was only present in one of the patients (3.4 %) (Table 5).
Discussion
We report here on the clinical and laboratory data regarding a large group of patients with diagnosis of SSc patients, all with Raynaud’s phenomenon, with the goal of identifying predictor factors for the development of DU. This study is based in 3-year long follow-up of 77 SSc patients that were divided into two subpopulations (with or without previous history of DU).
As far as we know, this is the first study that demonstrates that both endothelial dysfunction and impaired angiogenesis are risk factors for DU and have a predictive role for new DU events. We were also able to conclude that late scleroderma pattern is the strongest independent predictive risk factor for the occurrence of DU in SSc patients. Clearly, our findings suggest that endothelial dysfunction underlies recurrence of digital ulcers, which might explain why endothelin receptor antagonist treatment (bosentan) reduces the recurrence of DU [13]. Another new and useful information coming out of this investigation is that the capillaroscopic findings make up the only independent predictor factor for a first DU episode in SSc patients.
Association between previous history of DU and its recurrence is a commonly accepted concept [14], but this correlation has not been scientifically demonstrated. Manfredi et al. [15] have recently reported that DUs in the previous year were associated with new DU in the next 6 months. Our data do confirm previous DU as strong predictors for new DU episodes.
NVC is routinely used as a clinical marker in early and even preclinical stages of SSc [16] since it captures impaired capillary architecture and capillary loss that is a result of endothelial cell injury with disorganization of the inner layer of arterial vessels. As a very accessible tool, NVC could be a putative biomarker of disease progression, allowing target preventive therapy to be initialized [17].
Structural changes such as giant capillaries, microhemorrhages, avascular areas, and neo-angiogenic capillaries are important markers of disease progression and are present in more than 90 % of SSc patients [18]. Scoring the capillaroscopic patterns changes during the follow-up of SSc patients [19] enables capillaroscopy as a mandatory tool to quantify microangiopathy.
In clinical setting, qualitative evaluation is the more accessible and easy to perform. Late NVC patterns have been mostly described as an increased risk for DU development [17]. Caramaschi et al. reports a strong correlation between patients with late pattern and DU [20], Smith et al. described a correlation between worsening of NVC patterns and peripheral vascular lesions [21], Lambova et al. reported that DUs were strongly associated with active pattern, giant capillaries, hemorrhages, and avascular areas, proposing that active pattern could be used as a predictor for trophic lesions in the future and an indication for preventive target therapy [22], Alivernini et al. reported that patients with active skin ulcers have more avascular areas and a lower capillary density [23], and Ghizzoni et al. [2] described a correlation of DU with progression of NVC features.
Several scores have been proposed with prognostic purposes. Sulli et al. [24] proposed a semiquantitative microangiopathy evolution score (MES) that paralleled the evolution of the SSc microangiopathy but with no reference to association to DU, but it is an interesting microvascular injury surveillance score [17]. Smith et al. has proposed a simple semiquantitative NVC evaluation for day-to-day clinical use as a prognostic index of digital trophic lesions. Limitation of this study is that it includes and compares severe digital pitting scars, digital tip ulcerations, and gangrene without no differentiation between presentation and outcomes [25]. Sebastini et al. [26] proposed a Capillaroscopic Skin Ulcer Risk Index (CSURI) as a predictor risk of new onset of DU using NVC parameters. The strong limitation of this index was the mandatory presence of megacapillaries, so late patterns were excluded [26].
Manfredi et al. [15] recently suggested predictive risk chart of DU, taking into account capillaroscopic, demographic, and clinical–serological parameters. A significant positive association between DU and male gender, past DU, CSURI with a cutoff of 2.96, and ERS rate ≥20 mm h−1[15] was found.
Kim et al. described a quantitative analysis of NVC in six digits. Number of capillaries, number of capillaries loss, apical limb width, capillary width, and endothelin-1 (ET-1) were analyzed [27]. The major limitation of this study was that dilated capillaries were mandatory. The authors concluded that capillary dimension and loss of capillaries were strongly associated with DU. Recently, Ennis et al. [28] reported that intercapillary distance was greater in patients with active ulcers and capillary density was lower although not significant and no differences between patients with or without DU regarding capillary width, tortuosity, or derangement [28].
CAP multicenter observational, longitudinal prospective study of SSc patients with or without history of DU and with a 6 months follow-up reached the conclusion that final model for prediction of new DU in SSc patients with a past history of DU was a reduced mean number of capillaries in the middle finger of the dominant hand, increased number of current DU, and presence of current critical digital ischemia [29].
Our cohort investigation confirms results from previous studies that suggest a direct correlation between DU and NVC patterns [21, 25, 26, 30–32]. In addition to strengthening previous data on NVC and DU in SSc, we conclude that NVC is a useful method to predict which of the SSc patients are more likely to develop DU.
Endothelial dysfunction and free-radical damage are primary events throughout the course of the SSc disease, which result in vascular obliteration and diminished blood flow to the organs involved [33] and are prominently features of RP and DU. Among serological biomarkers of vasculopathy are vasoconstrictor ET-1 [34], cell adhesion molecules, including selectin, anti-endothelial antibodies, and the controversial vasodilator nitric oxide (NO), as well as ADMA, inhibitor of endothelial NO synthase (eNOS) [34].
ET-1 is known to play a key role in vascular pathology by various deleterious effects including hypertrophy of the vascular smooth muscle cells, cellular proliferation and fibrosis, increased vascular permeability, activation of leucocytes, and induction of cytokine and adhesion molecule expression [35]. Elevated ET-1 serum levels have been reported in primary RP, secondary RP, and SSc patients [36, 37], as well in the “late” scleroderma variant. ET-1 serum levels are correlated with a more severe clinical involvement, namely the presence of DU, either active or in the past [27, 38, 39]. Nevertheless, it must be referred that other studies found no correlation between ET-1 and DU [37, 40]. Sulli et al. [38] described significantly lower plasma levels of ET-1 in patients with “early” pattern compared to patients with late NVC pattern, thus supporting the involvement of ET-1 in the progression of microvascular/fibrotic damage in SSc. In our cohort of SSc patients with DU, we found increased serum levels of ET-1, compared with values for SSc patients with no previous episode of DU. In addition, we found that ET-1 levels less than 11.85 pmol/ml were strong predictors for a new DU episode in our 3-year long follow-up study. This finding supports the use of an endothelin receptor antagonist (bosentan) for preventive therapy of DU recurrence.
Elevated ADMA concentrations in patients with secondary Raynaud [41] and in diffuse cutaneous disease [42] are considered to be a reflection of the endothelial insult through either reduced and enhanced NO production. Besides the inhibition of endothelial NOS, deranged NO regulation due to overexpression of iNOS occurs in patients with SSc [43] and may contributes to accumulation of ADMA by eliminating dimethylarginine dimethylamonohydrolase (DDAH) activity [41]. In our study, SSc patients with active DU had increased ADMA serum levels compared to values from SSc patients with no previous DU; however, we could not demonstrate a predictive value for ADMA in DU.
As a response to increase in shear stress observed in SSc, patients release several vasodilators such as NO, prostaglandins, and endothelium-derived hyperpolarizing factor [44]. This response is commonly known as FMD and has been largely used for endothelium dysfunction assessment. NO is probably the major mediator of vasodilation, and reduced NO bioavailability has been broadly accepted as a marker of endothelium dysfunction [45]. A systematic review and meta-analysis of FMD [46] showed that in 71 % of the analyzed studies, brachial artery FMD% was significantly lower in SSc patients, as compared with controls. Also, low brachial artery FMD% has been reported as an independent predictor of cardiovascular risk [46]. Moreover, calcification and fibrosis both reduce vascular compliance and subsequently affect NO signaling by limiting vascular stretch [47], favoring macrovascular disease and arterial stiffness. Given that vascular changes leading to DU are characterized microscopically by intimal fibrosis, the decrease in vascular compliance may also contribute to the reduction of FMD values by reducing NOS activity in SSc patients. Clearly, the decrease in endothelial NO production is a characteristic feature of SSc vasculopathy, which largely explains the reduced FMD values in these patients [47]. Our study showed reduced FMD in SSc patients with active DU. Also, FMD < 9.41 % had a predictive role for new DU episodes. Strengthening macrovascular disease in DU pathogenesis is the predominance of positive Allen test in DU patients.
The severe capillary loss observed in the late-NVC pattern might also be related to impaired angiogenesis due to an imbalance of angiogenic factors. Our results are in accordance to those of other research groups that have reported significantly lower VEGF levels in SSc patients with active DU [48–50]. In contrast with the findings of Avouac et al. [51], we found lower serum levels of VEGF in patients with late NVC patterns compared to those with early/active NVC pattern, supporting those authors that have proposed before an inverse correlation between serum VEGF levels and capillary density [49, 52]. A prolonged overexpression of VEGF may have deleterious effects on the vascular network, as it may result in a chaotic vascular morphology with reduced blood flow in the newly formed vessels. A chronic and uncontrolled overexpression of VEGF does occur in SSc, and it may be significantly implicated in the altered vessel morphology observed in patients with the late NVC pattern [48, 51]. Previous reports have hypothesized that the insufficient angiogenesis observed in patients presenting the late-NVC pattern might be a result of increased angiostatic factors levels, which have been reported to be predominant in the late stages of SSc [51, 53–55]. In our cohort of SSc patients, enhanced serum levels of endoglin were a risk factor for DU but had with no significant predictive role. Further evaluation of other angiostatic markers should be assessed to confirm these findings.
Our study has several limitations that deserve consideration. First, our study is limited by its observational design, and only ischemic digital ulcers as marker of vasculopathy were assessed. Additionally, further studies are required to confirm our findings. However, our results show that qualitative capillaroscopic features can be used as an early identification tool of the SSc patients who are at the greatest risk of developing DU. Moreover, our NVC findings demonstrate its predictive value for new DU events in SSc patients. Endothelial dysfunction assessed by FMD and ET-1 levels were also predictor factors for DU recurrence, as detected in our 3-year long follow-up investigation. We propose that these findings are useful to identify high-risk patients since they will signal those patients that are to be selected for a closer clinical follow-up. Further studies assessing further clinical usefulness of our data are needed to validate their application in routine use, preventive or early therapeutic strategies. Finally, we should note that scleroderma remains amongst the most enigmatic of the connective tissue diseases, including not only its classification but also its associated conditions such as primary biliary cirrhosis, introduction of new therapies, development of new biomarkers, and genetic and epigenetic phenomenon [56–69].
Abbreviations
- ADMA:
-
Symmetric dimethylarginine
- ANA:
-
Antinuclear antibodies
- DU:
-
Digital ulcer
- ET-1:
-
Endothelin-1
- RP:
-
Raynaud’s phenomenon
- FMD:
-
Flow-mediated dilatation
- VEGF:
-
Vascular endothelial growth factor
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthase
- NVC:
-
Nailfold videocapillaroscopy
- SSc:
-
Systemic sclerosis
References
Muller-Ladner U, Distler O, Ibba-Manneschi L, Neumann E, Gay S (2009) Mechanisms of vascular damage in systemic sclerosis. Autoimmunity 42(7):587–595
Ghizzoni C, Sebastiani M, Manfredi A, Campomori F, Colaci M, Giuggioli D et al (2015) Prevalence and evolution of scleroderma pattern at nailfold videocapillaroscopy in systemic sclerosis patients: clinical and prognostic implications. Microvasc Res 99:92–95
Flavahan NA (2008) Regulation of vascular reactivity in scleroderma: new insights into Raynaud’s phenomenon. Rheum Dis Clin N Am 34(1):81–87, vii
Hummers LK, Hall A, Wigley FM, Simons M (2009) Abnormalities in the regulators of angiogenesis in patients with scleroderma. J Rheumatol 36(3):576–582
Galluccio F, Matucci-Cerinic M (2011) Two faces of the same coin: Raynaud phenomenon and digital ulcers in systemic sclerosis. Autoimmun Rev 10(5):241–243
Amanzi L, Braschi F, Fiori G, Galluccio F, Miniati I, Guiducci S et al (2010) Digital ulcers in scleroderma: staging, characteristics and sub-setting through observation of 1614 digital lesions. Rheumatology (Oxford, England) 49(7):1374–1382
Merkel PA, Herlyn K, Martin RW, Anderson JJ, Mayes MD, Bell P et al (2002) Measuring disease activity and functional status in patients with scleroderma and Raynaud’s phenomenon. Arthritis Rheum 46(9):2410–2420
Hachulla E, Clerson P, Launay D, Lambert M, Morell-Dubois S, Queyrel V et al (2007) Natural history of ischemic digital ulcers in systemic sclerosis: single-center retrospective longitudinal study. J Rheumatol 34(12):2423–2430
Hudson M, Fritzler MJ (2014) Diagnostic criteria of systemic sclerosis. J Autoimmun 48–49:38–41
Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA et al (2002) Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol 39(2):257–265
Cutolo M, Pizzorni C, Secchi ME, Sulli A (2008) Capillaroscopy. Best Pract Res Clin Rheumatol 22(6):1093–1108
Avouac J, Walker UA, Hachulla E, Riemekasten G, Cuomo G, Carreira PE, et al. (2014) Joint and tendon involvement predict disease progression in systemic sclerosis: a EUSTAR prospective study. Ann Rheum Dis
Matucci-Cerinic M, Denton CP, Furst DE, Mayes MD, Hsu VM, Carpentier P et al (2011) Bosentan treatment of digital ulcers related to systemic sclerosis: results from the RAPIDS-2 randomised, double-blind, placebo-controlled trial. Ann Rheum Dis 70(1):32–38
Korn JH, Mayes M, Matucci Cerinic M, Rainisio M, Pope J, Hachulla E et al (2004) Digital ulcers in systemic sclerosis: prevention by treatment with bosentan, an oral endothelin receptor antagonist. Arthritis Rheum 50(12):3985–3993
Manfredi A, Sebastiani M, Carraro V, Iudici M, Bocci M, Vukatana G, et al. (2014) Prediction risk chart for scleroderma digital ulcers: a composite predictive model based on capillaroscopic, demographic and clinico-serological parameters. Clin hemorheol Microcirc
Avouac J, Fransen J, Walker UA, Riccieri V, Smith V, Muller C et al (2011) Preliminary criteria for the very early diagnosis of systemic sclerosis: results of a Delphi Consensus Study from EULAR Scleroderma Trials and Research Group. Ann Rheum Dis 70(3):476–481
Silva I, Almeida J, Vasconcelos C (2015) A PRISMA-driven systematic review for predictive risk factors of digital ulcers in systemic sclerosis patients. Autoimmun Rev 14(2):140–152
Cutolo M, Smith V (2013) State of the art on nailfold capillaroscopy: a reliable diagnostic tool and putative biomarker in rheumatology? Rheumatology (Oxford, England) 52(11):1933–1940
Rossi D, Russo A, Manna E, Binello G, Baldovino S, Sciascia S et al (2013) The role of nail-videocapillaroscopy in early diagnosis of scleroderma. Autoimmun Rev 12(8):821–825
Caramaschi P, Canestrini S, Martinelli N, Volpe A, Pieropan S, Ferrari M et al (2007) Scleroderma patients nailfold videocapillaroscopic patterns are associated with disease subset and disease severity. Rheumatology (Oxford, England) 46(10):1566–1569
Smith V, Decuman S, Sulli A, Bonroy C, Piettte Y, Deschepper E et al (2012) Do worsening scleroderma capillaroscopic patterns predict future severe organ involvement? a pilot study. Ann Rheum Dis 71(10):1636–1639
Lambova S, Muller-Ladner U (2011) Capillaroscopic findings in systemic sclerosis -- are they associated with disease duration and presence of digital ulcers? Discov Med 12(66):413–418
Alivernini S, De Santis M, Tolusso B, Mannocci A, Bosello SL, Peluso G et al (2009) Skin ulcers in systemic sclerosis: determinants of presence and predictive factors of healing. J Am Acad Dermatol 60(3):426–435
Sulli A, Secchi ME, Pizzorni C, Cutolo M (2008) Scoring the nailfold microvascular changes during the capillaroscopic analysis in systemic sclerosis patients. Ann Rheum Dis 67(6):885–887
Smith V, De Keyser F, Pizzorni C, Van Praet JT, Decuman S, Sulli A et al (2011) Nailfold capillaroscopy for day-to-day clinical use: construction of a simple scoring modality as a clinical prognostic index for digital trophic lesions. Ann Rheum Dis 70(1):180–183
Sebastiani M, Manfredi A, Colaci M, D’Amico R, Malagoli V, Giuggioli D et al (2009) Capillaroscopic skin ulcer risk index: a new prognostic tool for digital skin ulcer development in systemic sclerosis patients. Arthritis Rheum 61(5):688–694
Kim HS, Park MK, Kim HY, Park SH (2010) Capillary dimension measured by computer-based digitalized image correlated with plasma endothelin-1 levels in patients with systemic sclerosis. Clin Rheumatol 29(3):247–254
Ennis H, Moore T, Murray A, Vail A, Herrick AL (2014) Further confirmation that digital ulcers are associated with the severity of abnormality on nailfold capillaroscopy in patients with systemic sclerosis. Rheumatology (Oxford, England) 53(2):376–377
Cutolo MHA, Distler O et al (2013) Nailfold videocapillaroscopy and other predictive factors associated with new digital ulcers in systemic sclerosis. Data from the CAP study. Ann Rheum Dis 72(S3):146
Sebastiani M, Manfredi A, Vukatana G, Moscatelli S, Riato L, Bocci M et al (2012) Predictive role of capillaroscopic skin ulcer risk index in systemic sclerosis: a multicentre validation study. Ann Rheum Dis 71(1):67–70
Sebastiani M, Manfredi A, Lo Monaco A, Praino E, Riccieri V, Grattagliano V et al (2013) Capillaroscopic Skin Ulcers Risk Index (CSURI) calculated with different videocapillaroscopy devices: how its predictive values change. Clin Exp Rheumatol 31(2 Suppl 76):115–117
Sebastiani M, Manfredi A, Cassone G, Giuggioli D, Ghizzoni C, Ferri C (2014) Measuring microangiopathy abnormalities in systemic sclerosis patients: the role of capillaroscopy-based scoring models. Am J Med Sci
Zhang L, Wan YN, Zhao JH, Wang YJ, Wang YX, Yan JW, et al. (2014) The Association Between Systemic Sclerosis, Arginine and Asymmetric Dimethylarginine. Inflammation
Kahaleh B, Mulligan-Kehoe MJ (2012) Mechanisms of Vascular Disease. J. Varga et al. (eds), Scleroderma: from pathogenesis to comprehensive managment:227–46
Kim NH, Rubin LJ (2002) Endothelin in health and disease: endothelin receptor antagonists in the management of pulmonary artery hypertension. J Cardiovasc Pharmacol Ther 7(1):9–19
Kahaleh MB, Sherer GK, LeRoy EC (1979) Endothelial injury in scleroderma. J Exp Med 149(6):1326–1335
Yamane K, Miyauchi T, Suzuki N, Yuhara T, Akama T, Suzuki H et al (1992) Significance of plasma endothelin-1 levels in patients with systemic sclerosis. J Rheumatol 19(10):1566–1571
Sulli A, Soldano S, Pizzorni C, Montagna P, Secchi ME, Villaggio B et al (2009) Raynaud’s phenomenon and plasma endothelin: correlations with capillaroscopic patterns in systemic sclerosis. J Rheumatol 36(6):1235–1239
Aghaei M, Gharibdost F, Zayeni H, Akhlaghi M, Sedighi S, Rostamian AR et al (2012) Endothelin-1 in systemic sclerosis. Indian Dermatol Online J 3(1):14–16
Cozzani E, Javor S, Laborai E, Drosera M, Parodi A (2013) Endothelin-1 levels in scleroderma patients: a pilot study. ISRN Dermatol 2013:125632
Dimitroulas T, Sandoo A, Kitas GD (2012) Asymmetric dimethylarginine as a surrogate marker of endothelial dysfunction and cardiovascular risk in patients with systemic rheumatic diseases. Int J Mol Sci 13(10):12315–12335
Dooley A, Gao B, Bradley N, Abraham DJ, Black CM, Jacobs M et al (2006) Abnormal nitric oxide metabolism in systemic sclerosis: increased levels of nitrated proteins and asymmetric dimethylarginine. Rheumatology (Oxford, England) 45(6):676–684
Cotton SA, Herrick AL, Jayson MI, Freemont AJ (1999) Endothelial expression of nitric oxide synthases and nitrotyrosine in systemic sclerosis skin. J Pathol 189(2):273–278
Pyke KE, Tschakovsky ME (2005) The relationship between shear stress and flow-mediated dilatation: implications for the assessment of endothelial function. J Physiol 568(Pt 2):357–369
Harris RA, Nishiyama SK, Wray DW, Richardson RS (2010) Ultrasound assessment of flow-mediated dilation. Hypertension 55(5):1075–1085
Au K, Singh MK, Bodukam V, Bae S, Maranian P, Ogawa R et al (2011) Atherosclerosis in systemic sclerosis: a systematic review and meta-analysis. Arthritis Rheum 63(7):2078–2090
Takahashi T, Asano Y, Amiya E, Hatano M, Tamaki Z, Takata M et al (2014) Clinical correlation of brachial artery flow-mediated dilation in patients with systemic sclerosis. Modern Rheumatol / Jpn Rheumatism Assoc 24(1):106–111
Distler O, Distler JH, Scheid A, Acker T, Hirth A, Rethage J et al (2004) Uncontrolled expression of vascular endothelial growth factor and its receptors leads to insufficient skin angiogenesis in patients with systemic sclerosis. Circ Res 95(1):109–116
Koch AE, Distler O (2007) Vasculopathy and disordered angiogenesis in selected rheumatic diseases: rheumatoid arthritis and systemic sclerosis. Arthritis Res Ther 9(2):S3
Farouk HM, Hamza SH, El Bakry SA, Youssef SS, Aly IM, Moustafa AA et al (2013) Dysregulation of angiogenic homeostasis in systemic sclerosis. Int J Rheum Dis 16(4):448–454
Avouac J, Vallucci M, Smith V, Senet P, Ruiz B, Sulli A et al (2013) Correlations between angiogenic factors and capillaroscopic patterns in systemic sclerosis. Arthritis Res Ther 15(2):R55
Ferri C, Giuggioli D, Sebastiani M, Colaci M (2007) Treatment of severe scleroderma skin ulcers with recombinant human erythropoietin. Clin Exp Dermatol 32(3):287–290
Mulligan-Kehoe MJ, Drinane MC, Mollmark J, Casciola-Rosen L, Hummers LK, Hall A et al (2007) Antiangiogenic plasma activity in patients with systemic sclerosis. Arthritis Rheum 56(10):3448–3458
Hebbar M, Peyrat JP, Hornez L, Hatron PY, Hachulla E, Devulder B (2000) Increased concentrations of the circulating angiogenesis inhibitor endostatin in patients with systemic sclerosis. Arthritis Rheum 43(4):889–893
Fujimoto M, Hasegawa M, Hamaguchi Y, Komura K, Matsushita T, Yanaba K et al (2006) A clue for telangiectasis in systemic sclerosis: elevated serum soluble endoglin levels in patients with the limited cutaneous form of the disease. Dermatology (Basel, Switzerland) 213(2):88–92
Mosca M, Tani C, Vagnani S, Carli L, Bombardieri S (2014) The diagnosis and classification of undifferentiated connective tissue diseases. J Autoimmun 48–49:50–52
Voswinkel J, Francois S, Simon JM, Benderitter M, Gorin NC, Mohty M, Fouillard L et al (2013) Use of mesenchymal stem cells (MSC) in chronic inflammatory fistulizing and fibrotic diseases: a comprehensive review. Clin Rev Allergy Immunol 45(2):180–192
Moinzadeh P, Nihtyanova SI, Howell K, Ong VH, Denton CP (2012) Impact of hallmark autoantibody reactivity on early diagnosis in scleroderma. Clin Rev Allergy Immunol 43(3):249–255
Salazar GA, Assassi S, Wigley F, Hummers L, Varga J, Hinchcliff M et al (2015) Antinuclear antibody-negative systemic sclerosis. Semin Arthritis Rheum 44(6):680–686
Bose N, Chiesa-Vottero A, Chatterjee S (2015) Scleroderma renal crisis. Semin Arthritis Rheum 44(6):687–694
Maverakis E, Patel F, Kronenberg DG, Chung L, Fiorentino D, Allanore Y et al (2014) International consensus criteria for the diagnosis of Raynaud’s phenomenon. J Autoimmun 48–49:60–65
Srivastava N, Hudson M, Tatibouet S, Wang M, Baron M, Fritzler MJ, et al. (2015)Thinking outside the box-The associations with cutaneous involvement and autoantibody status in systemic sclerosis are not always what we expect. Semin Arthritis Rheum
Tani C, Carli L, Vagnani S, Talarico R, Baldini C, Mosca M et al (2014) The diagnosis and classification of mixed connective tissue disease. J Autoimmun 48–49:46–49
Hudson M, Fritzler MJ (2014) Diagnostic criteria of systemic sclerosis. J Autoimmun 48–49:38–41
Mitchell RN (2013) Learning from rejection: what transplantation teaches us about (other) vascular pathologies. J Autoimmun 45:80–89
Massie C, Hudson M, Tatibouet S, Steele R, Huynh T, Friztler MJ et al (2014) Absence of an association between anti-Ro antibodies and prolonged QTc interval in systemic sclerosis: a multicenter study of 689 patients. Semin Arthritis Rheum 44(3):338–344
Luo Y, Wang Y, Wang Q, Xiao R, Lu Q (2013) Systemic sclerosis: genetics and epigenetics. J Autoimmun 41:161–167
Floreani A, Franceschet I, Cazzagon N, Spinazze A, Buja A, Furlan P et al (2015) Extrahepatic autoimmune conditions associated with primary biliary cirrhosis. Clin Rev Allergy Immunol 48(2–3):192–197
van den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, Tyndall A et al (2013) 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League against Rheumatism collaborative initiative. Arthritis Rheum 65(11):2737–2747
Acknowledgments
This study was partially supported by a research grant from Teaching and Research Department (Departamento de Ensino e Investigação) of Oporto Hospital Center (reference 054/10 (036-DEFI/051-CES) and from a Foundation for Science and Technology (FCT) postdoc grant SFRH/BPD/86383/2012. The authors thank the Clinical Pathology Department for their valuable technical assistance.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Silva, I., Teixeira, A., Oliveira, J. et al. Endothelial Dysfunction and Nailfold Videocapillaroscopy Pattern as Predictors of Digital Ulcers in Systemic Sclerosis: a Cohort Study and Review of the Literature. Clinic Rev Allerg Immunol 49, 240–252 (2015). https://doi.org/10.1007/s12016-015-8500-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-015-8500-0