Abstract
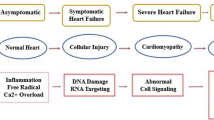
Although doxorubicin (Dox) is a backbone of chemotherapy, the search for an effective and safe therapy to revoke Dox-induced acute cardiotoxicity remains a critical matter in cardiology and oncology. The current study was the first to explore the probable protective effects of native and gamma-irradiated fractions with bradykinin-potentiating activity (BPA) isolated from scorpion (Leiurus quinquestriatus) venom against Dox-induced acute cardiotoxicity in rats. Native or irradiated fractions (1 μg/g) were administered intraperitoneally (i.p.) twice per week for 3 weeks, and Dox (15 mg/kg, i.p.) was administered on day 21 at 1 h after the last native or irradiated fraction treatment. Electrocardiographic (ECG) aberrations were ameliorated in the Dox-treated rats pretreated with the native fraction, and the irradiated fraction provided greater amelioration of ECG changes than that of the native fraction. The group pretreated with native protein with BPA also exhibited significant improvements in the levels of oxidative stress-related, inflammatory, angiogenic, fibrogenic, and apoptotic markers compared with those of the Dox group. Notably, the irradiated fraction restored these biomarkers to their normal levels. Additionally, the irradiated fraction ameliorated Dox-induced histological changes and alleviated the severity of cardiac injury to a greater extent than that of the native fraction. In conclusion, the gamma-irradiated detoxified fraction of scorpion venom elicited a better cardioprotective effect than that of the native fraction against Dox-induced acute cardiotoxicity in rats.








Similar content being viewed by others
Data Availability
All data generated or analyzed during this study are included in this published article.
References
Pennington, M. W., Czerwinski, A., & Norton, R. S. (2018). Peptide therapeutics from venom: Current status and potential. Bioorganic & Medicinal Chemistry, 26, 2738–2758.
Ferreira, S. H. A. (1965). A bradykinin-potentiating factor (BPF) present in the venom of Bothrops jararaca. British Journal of Pharmacology and Chemotherapy, 24(1), 163–169.
Cushman, D. W., & Ondetti, M. A. (1991). History of the design of captopril and related inhibitors of angiotensin converting enzyme. Hypertension, 17(4), 589–592.
Fernandez, J. H., Neshich, G., & Camargo, A. C. (2004). Using bradykinin-potentiating peptide structures to develop new antihypertensive drugs. Genetics and Molecular Research, 3(4), 554–563.
Dendorfer, A., Wolfrum, S., & Dominiak, P. (1999). Pharmacology and cardiovascular implications of the kinin-kallikrein system. Japanese Journal of Pharmacology., 79(4), 403–426.
Sciani, J. M., & Pimenta, D. C. (2017). The modular nature of bradykinin potentiating peptides isolated from snake venoms. Journal of Venomous Animals and Toxins including Tropical Diseases, 23, 45.
Verano-Braga, T., Rocha-Resende, C., Silva, D. M., Ianzer, D., Martin-Eauclaire, M. F., Bougis, P. E., et al. (2008). Tityus serrulatus hypotensins: A new family of peptides from scorpion venom. Biochemical and Biophysical Research Communications, 371(3), 515–520.
Conceição, K., Konno, K., de Melo, R. L., Antoniazzi, M. M., Jared, C., Sciani, J. M., et al. (2007). Isolation and characterization of a novel bradykinin potentiating peptide (BPP) from the skin secretion of Phyllomedusa hypochondrialis. Peptides, 28(3), 515–523.
Chi, C. W., Wang, S. Z., Lg, X., Wang, M. Y., Lo, S. S., & Huang, W. D. (1985). Structure-function studies on the bradykinin potentiating peptide from Chinese snake venom (Agkistrodon halys Pallas). Peptides, 6(3), 339–342.
Cintra, A. C., Vieira, C. A., & Giglio, J. R. (1990). Primary structure and biological activity of bradykinin potentiating peptides from Bothrops insularis snake venom. Journal of Protein Chemistry., 9(2), 221–227.
Gomes, C. L., Konno, K., Conceicao, I. M., Ianzer, D., Yamanouye, N., Prezoto, B. C., et al. (2007). Identification of novel bradykinin-potentiating peptides (BPPs) in the venom gland of a rattlesnake allowed the evaluation of the structure-function relationship of BPPs. Biochemical Pharmacology., 74(9), 1350–1360.
Zeng, X. C., Corzo, G., & Hahin, R. (2005). Scorpion venom peptides without disulfide bridges. IUBMB Life, 1, 13–21.
Zhijian, C., Feng, L., Yingliang, W., Xin, M., & Wenxin, L. (2006). Genetic mechanisms of scorpion venom peptide diversification. Toxicon, 47, 348–355.
Camargo, A. C., Ianzer, D., Guerreiro, J. R., & Serrano, S. M. (2012). Bradykinin-potentiating peptides: Beyond captopril. Toxicon, 59, 516–523.
Ortiz, E., Gurrola, G. B., Schwartz, E. F., & Possani, L. D. (2015). Scorpion venom com-ponents as potential candidates for drug development. Toxicon, 93, 125–135.
Amra, E. A., Lashein, F. M., Seleem, A. A., & Badr, A. H. (2018). Counter effect of bee venom and its extracted bradykinin-potentiating factor on acrylamide and chips administration induced complications in the liver and kidney of male mice. The Journal of Basic and Applied Zoology., 79, 34.
Lipps, B. V. (1998). Biological and immunological properties of nerve growth factor from snake venom. Journal of Natural Toxins., 7, 121–130.
Guo, L. Y., Zhu, J. F., & Wu, X. F. (1999). Cloning of a cDNA encoding a nerve growth factor precursor from the Agkistrodon halys Pallas. Toxicon, 37, 465–470.
Nassar, A. Y., Abu Sinna, G., & Abd-El-Rahim, S. A. (1990). Effect of a bradykinin potentiating fraction isolated from venom of the Egyptian scorpion, Buthus occitanus on the ovaries and endometrium of mice. Toxicon, 28(5), 525–534.
Bekheet, S. H. M., Awadallaa, E. A., Salman, M. M. A., & Hassan, M. K. (2011). Bradykinin potentiating factor isolated from Buthus occitanus venom has a protective effect against cadmium-induced rat liver and kidney damage. Journal of Tissue and Cell., 43, 337–343.
El-Saadani, M. A. (2004). A scorpion venom peptide fraction induced prostaglandin biosynthesis in guinea pig kidneys: Incorporation of 14C-linoleic acid. Journal of Biochemistry., 135, 109–116.
Meki, A. M. A., & Omar, H. M. A. (1997). Bradykinin potentiating fraction isolated from the venom of Egyptian scorpion Buthus occitanus induced prostaglandin biosynthesis in female guinea pigs. Comparative Biochemistry & Physiology., 116(3), 183–189.
Nassar, A. Y., Abu-Sinna, G., Abdel Rahim, S., Soliman, M., & El-Saadani, M. (1992). Bradykinin potentiating fraction isolated from venom of Buthus occitanus promotes spermatogenesis in premature mice. Rec Advantage Toxinology and Research, 2, 119–135.
Takemura, G., & Fujiwara, H. (2007). Doxorubicin-induced cardiomyopathy from the cardiotoxic mechanisms to management. Progress in Cardiovascular Diseases, 49, 330–352.
Sant, M., Allemani, C., & Santaquilani, M. (2009). Survival of cancer patients diagnosed in 1995–1999. Results and commentary. European Journal of Cancer., 45(6), 931–991.
Chang, W. T., Li, J., Haung, H. H., Liu, H., & Han, M. (2011). Baicalein protects against doxorubicin-induced cardiotoxicity by attenuation of mitochondrial oxidant injury and JNK activation. Journal of Cellular and Biochemistry, 112, 2873–2881.
Octavia, Y., Tocchetti, C. G., Gabrielson, K. L., Janssens, S., Crijns, H. J., & Moens, A. L. (2012). Doxorubicin-induced cardiomyopathy: From molecular mechanisms to therapeutic strategies. Journal of Molecular and Cellular Cardiology, 52, 1213–1225.
Sawyer, D. B., Peng, X., Chen, B., Pentassuglia, L., & Lim, C. C. (2010). Mechanisms of anthracycline cardiac injury: Can we identify strategies for cardioprotection? Progress in Cardiovascular Diseases, 53, 105–113.
Scott, J. M., Khakoo, A., Mackey, J. R., Haykowsky, M. J., & Douglas, P. S. (2011). Modulation of anthracycline-induced cardiotoxicity by aerobic exercise in breast cancer: Current evidence and underlying mechanisms. Circulation, 124, 642–650.
Kalyanaraman, B. (2020). Teaching the basics of the mechanism of doxorubicin-induced cardiotoxicity: Have we been barking up the wrong tree? Redox Biology, 29, 101394.
Swain, S. M., Whaley, F. S., & Ewer, M. S. (2003). Congestive heart failure in patients treated with doxorubicin: A retrospective analysis of three trials. Cancer, 97, 2869–2879.
Nebigil, C. G., & Désaubry, L. (2018). Updates in anthracycline-mediated cardiotoxicity. Frontiers in Pharmacology, 9, 1262.
Danz, E. D., Skramsted, J., Henry, N., Bennett, J. A., & Keller, R. S. (2009). Resveratrol prevents doxorubicin cardiotoxicity through mitochondrial stabilization and the Sirt1 pathway. Free Radical Biology and Medicine., 46, 1589–1597.
Chang, H. M., Moudgil, R., Scarabelli, T., Okwuosa, T. M., & Yeh, E. T. H. (2017). Cardiovascular complications of cancer therapy: Best practices in diagnosis, prevention, and management: Part 1. Journal of American College of Cardiology., 70(20), 2536–2551.
El-Demerdash, E., Ali, A. A., Sayed-Ahmed, M. M., & Osman, A. M. (2003). New aspects in probucol cardioprotection against doxorubicin-induced cardiotoxicity. Cancer Chemotherapy and Pharmacology., 52(5), 411–416.
Silva dos Santos, D., & Goldenberg, R. C. (2018). Doxorubicin-induced cardiotoxicity: From mechanisms to development of efficient therapy. In Cardiotoxicity. Intechopen.
Bosch, X., Rovira, M., Sitges, M., Domènech, A., Ortiz-Pérez, J. T., de Caralt, T. M., et al. (2013). Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies: The overcome trial (prevention of left ventricular dysfunction with Enalapril and carvedilol in patients submitted to intensive Chemotherapy for the treatment of Malignant hemopathies). Journal of American College of Cardiology., 61, 2355–2362.
Ibrahim, M. A., Ashour, O. M., Ibrahim, Y. F., El-Bitar, H. I., Gomaa, W., & Abdel-Rahim, S. R. (2009). Angiotensin-converting enzyme inhibition and angiotensin AT(1)-receptor antagonism equally improve doxorubicin-induced cardiotoxicity and nephrotoxicity. Pharmacological Research., 60, 373–381.
Blaes, A. H., Gaillard, P., Peterson, B. A., Yee, D., & Virnig, B. (2010). Angiotensin converting enzyme inhibitors may be protective against cardiac complications following anthracycline chemotherapy. Breast Cancer Research Treatment., 122, 585–590.
Morris, S. D., & Yellon, D. M. (1997). Angiotensin-converting enzyme inhibitors potentiate preconditioning through Bradykinin B2 Receptor activation in human heart. JACC., 29(7), 1599–1606.
Caproni, P., Baptista, J. A., de Almeida, T. L., Passos, L. A. C., & Nascimento, N. (2009). Study of irradiated bothropstoxin-1 with 60Co gamma rays: Immune system behavior. Journal of Venomous Animals and Toxins including Tropical Diseases., 15(2), 216–225.
Oliveira, K. C., Spencer, P. J., Ferreira, R. S., & Nascimento, N. (2015). New insights into the structural characteristics of irradiated crotamine. Journal of Venomous Animals and Toxins including Tropical Diseases., 21, 14.
Nascimento, N., Seebart, C. S., Francis, B., Rogero, J. R., & Kaiser, I. I. (1996). Influence of ionizing radiation on crotoxin: Biochemical and immunological aspects. Toxicon, 34(1), 123–131.
Clissa, B. P., Nascimento, N. D., & Rogero, J. R. (1999). Toxicity and immunogenicity of Crotalus durissus terrificus venom treated with different doses of gamma rays. Toxicon, 37, 1131–1141.
Baptista, N. B., Saidemberg, D. M., de Souza, B. M., Cesar-Tognoli, L. M., Ferreira, V. M., Mendes, M. A., et al. (2010). Pro-tonectin (1–6): A novel chemotactic peptide from the venom of the social was Agelaia pallipes pallipes. Toxicon, 56, 880–889.
Yaqoob, R., Tahir, H. M., Arshad, M., Naseem, S., & Ahsan, M. M. (2016). Optimization of the conditions for maximum recovery of venom from scorpions by electrical stimulation. Pakistan Journal of Zoology., 48, 265–269.
Meier, J., & Theakston, R. D. C. (1986). Approximate LD50 determinations of snake venoms using eight to ten experimental animals. Toxicon, 24, 345–401.
Casare, M. S., Baptista, J. A., Spencer, P. J., & Nascimento, N. (2004). Effects of 60Co radiation on the molecular strucure of crotamine. Radiation Physics and Chemistry, 71, 417–418.
Zordoky, B. N. M., Mohamed, A. A., Aboutabl, M. E., & El-Kadi, A. O. S. (2011). Acute doxorubicin cardiotoxicity alters cardiac cytochrome P450 expression and arachidonic acid metabolism in rats. Toxicology and Applied Pharmacology., 242, 38–46.
Ashry, O., Moustafa, M., Baset, A. A. E., Abu Sinna, G. E., & Farouk, H. (2012). Outcome of venom bradykinin potentiating factor on rennin-angiotensin system in irradiated rats. International Journal of Radiation Biology, 88(11), 840–845.
Pacher, P., Liaudet, L., Bai, P., Mabley, J. G., Kaminski, P. M., Virág, L., et al. (2003). Potent Metalloporphyrin peroxynitrite decomposition catalyst protects against the development of doxorubicin-induced cardiac dysfunction. Circulation, 107(6), 896–904.
Lowry, O. H., Rosebrough, N. J., Farr, A. L., & Randall, R. J. (1951). Protein measurement with the Folin phenol reagent. The Journal of Biological Chemistry, 193, 265–275.
Ahmed, L. A., Shehata, N. I., Abdelkader, N. F., & Khattab, M. M. (2014). Tempol, a superoxide dismutase mimetic agent, ameliorates cisplatin-induced nephrotoxicity through alleviation of mitochondrial dysfunction in mice. PLoS ONE, 9, e108889.
Livak, K. J., & Schmittgen, T. D. (2001). Analysis of relative gene expression data using real-time quantitative PCR and the 2(-ΔΔC (T)) method. Methods, 25, 402–408.
Pfaffl, M. W. (2001). A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Research, 29, e45.
Bancroft, J. H. D., Stevens, A., & Turner, D. R. (1990). Theory and practice of histological techniques. In Bancroft, J. D., Stevens, A., & Turner, D. R. (Eds.). 3th ed. (p. 726) London, Melbourne and New York: Churchill Livingstone Edinburg.
Acikel, M., Buyukokuroglu, M. E., Erdogan, F., Aksoy, H., Bozkurt, E., & Senocak, H. (2005). Protective effects of dantrolene against myocardial injury induced by isoproterenol in rats: Biochemical and histological findings. International Journal of Cardiology., 98(3), 389–394.
Ammar, E. M., Said, S. A., Suddek, G. M., & El Damarawy, S. L. (2011). Amelioration of doxorubicin-induced cardiotoxicity by deferiprone in rats. Canadian Journal of Physiology and Pharmacology, 89, 269–276.
Koti, B. C., Nagathan, S., Vishwanathswamy, A., Gadad, P. C., & Thippeswamy, A. (2013). Cardioprotective effect of vedic guard against doxorubicin-induced cardiotoxicity in rats: A biochemical, electrocardiographic and histopathological study. Pharmacognosy Magazine, 9(34), 176–181.
Warpe, V. S., Mali, V. R., Arulmozhi, S., Bodhankar, S. L., & Mahadik, K. R. (2015). Cardioprotective effect of ellagic acid on doxorubicin induced cardiotoxicity in Wistar rats. Journal of Acute Medicine., 5, 1–8.
Emeka, P. M., & Al-Ahmed, A. (2017). Effect of metformin on ECG, HR and BP of rats administered with cardiotoxic agent doxorubicin. International Journal of Basic & Clinical Pharmacology., 6(5), 1054–1059.
Sun, X. P., Wan, L., Yang, Q. J., Huo, Y., Han, Y. L., & Arch, C. G. (2017). Scutellarin protects against doxorubicin-induced acute cardiotoxicity and regulates its accumulation in the heart. Pharmaceutical Research., 40, 875–883.
Shaker, R. A., Abboud, S. H., Assad, H. C., & Hadi, N. (2018). Enoxaparin attenuates doxorubicin induced cardiotoxicity in rats via interfering with oxidative stress, inflammation and apoptosis. BMC Pharmacology and Toxicology., 19, 3.
Henri, C., Heinonen, T., & Tardif, J. C. (2016). The role of biomarkers in decreasing risk of cardiac toxicity after cancer therapy. Biomarkers in Cancer., 8(S2), 39–45.
Rao, V. A. (2013). Iron chelators with topoisomerase-inhibitory activity and their anticancer applications. Antioxidants & Redox Signaling., 18(8), 930–955.
Abu Gazia, M., & Abu El-Magd, M. (2018). Ameliorative effect of cardamom aqueous extract on doxorubicin-induced cardiotoxicity in rats. Cells Tissues Organs., 206(1–2), 62–72.
Ciaccio, M., Valenza, M., Tesoriere, L., Bongiorno, A., Albiero, R., & Livrea, M. A. (1993). Vitamin A inhibits doxorubicin-induced membrane lipid peroxidation in rat tissues in vivo. Archives of Biochemistry and Biophysics., 302, 103–108.
Childs, A. C., Phaneuf, S. L., Dirks, A. J., Phillips, T., & Leeuwenbur, C. (2002). Doxorubicin treatment in vivo causes cytochrome c release and cardiomyocyte apoptosis, as well as increased mitochondrial efficiency, superoxide dismutase activity, and Bcl-2: Bax ratio. Cancer Research., 62(16), 4592–4598.
Mikrut, K., Paluszak, J., Kozlik, J., Sosnowski, P., Krauss, H., & Grześkowiak, E. (2001). The effect of bradykinin on the oxidative state of rats with acute hyperglycaemia. Diabetes Research and Clinical Practice, 51, 79–85.
Sancho-Bru, P., Bataller, R., Fernandez-Varo, G., Moreno, M., Ramalho, L. N., Colmenero, J., et al. (2007). Bradykinin attenuates hepatocellular damage and fibrosis in rats with chronic liver injury. Gastroenterology, 133(6), 2019–2028.
Oeseburg, H., Iusuf, D., Harst, P., Gilst, W. H., Henning, R. H., & Roks, A. J. (2009). Bradykinin protects against oxidative stress–induced endothelial cell senescence. Hypertension, 53, 417–422.
Cappetta, D., De Angelis, A., Sapio, L., Prezioso, L., Illiano, M., & Quaini, F., et al. (2017). Oxidative stress and cellular response to doxorubicin: A common factor in the complex milieu of anthracycline cardiotoxicity. Oxidative Medicine and Cellular Longevity. 15210202017.
Rocca, C., Pasqua, T., Cerra, M. C., & Angelone, T. (2020). Cardiac damage in anthracyclines therapy: Focus on oxidative stress and inflammation. Antioxidants and Redox Signaling., 32(15), 1081–1097.
Yadav, U., & Ramana, K. V. (2013). Regulation of NF-κB- induced inflammatory signaling by lipid peroxidation-derived aldehydes. Oxidative Medicine and Cellular Longevity., 690545, 11.
Djavaheri-Mergny, M., Javelaud, D., Wietzerbin, J., & Besançon, F. (2004). NF-kappa B activation prevents apoptotic oxidative stress via an increase of both thioredoxin and MnSOD levels in TNF alpha treated Ewing sarcoma cells. FEBS Letters., 578, 111–115.
Lingappan, K. (2018). NF-κB in oxidative stress. Current in Opinion Toxicology., 7, 81–86.
Zhou, S., Palmeira, C. M., & Wallace, K. B. (2001). Doxorubicin-induced persistent oxidative stress to cardiac myocytes. Toxicological Letters., 121, 151–157.
Minotti, G., Menna, P., Salvatorelli, E., Cairo, G., & Gianni, L. (2004). Anthracyclines: Molecular advances and pharmacologic developments in antitumor activity and cardiotoxicity. Pharmacological Reviews., 56, 185–229.
Sun, Z., Yan, B., YanYu, W., Yao, X., Ma, X., Sheng, G., et al. (2016). Vitexin attenuates acute doxorubicin cardiotoxicity in rats via the suppression of oxidative stress, inflammation and apoptosis and the activation of FOXO3a. Experimental and Therapeutic Medicine., 12, 1879–1884.
Abdel-Wahab, B. A., & Metwally, M. E. (2014). Clozapine-induced cardiotoxicity in rats: Involvement of tumor necrosis factor alpha, NF-Kβ and caspase-3. Toxicological Reports, 20(1), 1213–1223.
Kong, P., Christia, P., & Frangogiannis, N. G. (2014). The pathogenesis of cardiac fibrosis. Cellular and Molecular Life Sciences., 71(4), 549–574.
Bujak, M., & Frangogiannis, N. G. (2007). The role of TGF-beta signaling in myocardial infarction and cardiac remodeling. Cardiovascular Research., 74(2), 184–195.
Chen, C. T., Wang, Z. H., Hsu, C. C., Lin, H. H., & Chen, J. H. (2015). In vivo protective effects of diosgenin against doxorubicin-induced cardiotoxicity. Nutrients., 7, 4938–4954.
Beckman, S. A., Chen, W. C., Tang, Y., Proto, J. D., Mlakar, L., Wang, B., et al. (2013). Beneficial effect of mechanical stimulation on the regenerative potential of muscle-derived stem cells is lost by inhibiting vascular endothelial growth factor. Arteriosclerosis, Thrombosis, and Vascular Biology., 33, 2004–2012.
Attia, G. M., & El mansy RA and Algaidi SA,. (2017). Silymarin decreases the expression of VEGF-A, iNOS and caspase-3 and preserves the ultrastructure of cardiac cells in doxorubicin induced cardiotoxicity in rats: A possible protective role. International Journal of Clinical Medicine., 10(2), 4158–4173.
Abdel-Raheem, I. T., Taye, A., & Abouzied, M. M. (2013). Cardioprotective effects of nicorandil, a mitochondrial potassium channel opener against doxorubicin-induced cardiotoxicity in rats. Basic & Clinical Pharmacology & Toxicology., 113, 158–166.
Laursen, J. B., Somers, M., Kurz, S., McCann, L., Warnholtz, A., & Freeman, B. A. (2001). Endothelial regulation of vasomotion in apoE-deficient mice: Implications for interactions between peroxynitrite and tetrahydrobiopterin. Circulation, 103, 1282–1288.
Mungrue, I. N., Gros, R., You, X., Pirani, A., Azad, A., & Csont, T. (2002). Cardiomyocyte overexpression of iNOS in mice results in peroxynitrite generation, heart block, and sudden death. Journal of Clinical Investigation, 109, 735–743.
Abbas, N. A. T., & Kabil, S. L. (2017). Pentoxifylline and cilostazol against rat heart injuries induced by doxorubicin. Egyptian Journal of Basic and Clinical Pharmacology., 7(1), 47–56.
Yu, J., Gao, H., Wu, C., Xu, Q. M., Lu, I. D. J. J., & Chen, X. (2018). Diethyl Blechnic, a novel natural product isolated from salvia miltiorrhiza bunge, inhibits doxorubicin-induced apoptosis by inhibiting ROS and activating JNK1/2. International Journal of Molecular Sciences, 19, 1809.
Mantawy, E. M., Esmat, A., El-Bakly, W. M., Salah ElDin, R. A., & El-Demerdash, E. (2017). Mechanistic clues to the protective effect of chrysin against doxorubicin-induced cardiomyopathy: Plausible roles of p53 MAPK and AKT pathways. Science Reports, 7, 4795.
Salman, M. M., Kotb, A. M., Haridy, M. A., & Hammad, S. (2016). Hepato-and nephroprotective effects of bradykinin potentiating factor from scorpion (Buthusoccitanus) venom on mercuric chloride-treated rats. EXCLI Journal, 15, 807–816.
Dong, R., Xu, X., Li, G., Feng, W., Zhao, G., Zhao, J., et al. (2013). Bradykinin inhibits oxidative stress-induced cardiomyocytes senescence via regulating redox state. PLoS ONE, 8(10), e77034.
Ďurackova, Z. (2014). Free radicals and antioxidants for non-experts. In I. Laher (Ed.), Systems biology of free radicals and antioxidants (1st ed., pp. 3–38). Berlin: Springer.
Hagiwara, M., Murakami, H., Ura, N., Agata, J., Yoshida, H., & Higashiura, K. (2004). Renal protective role of bradykinin B1 receptor in stroke-prone spontaneously hypertensive rats. Hypertension and Research., 27, 399–408.
Yoshihisa, M., Katsuya, H., Junji, N., Tomio, S., & Hideo, K. (2004). Endothelial dysfunction and altered bradykinin response due to oxidative stress induced by serum deprivation in the bovine cerebral artery. European Journal of Pharmacology., 491(1), 53–60.
Acknowledgements
The authors are thankful to the Faculty of Pharmacy, Cairo University, and the Atomic Energy Authority for cooperation. The authors are also grateful to Prof. Dr. Ahmed Othman, Faculty of Veterinary Medicine, Cairo University, for his efforts in the histopathological examinations.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
LAA, FYA and AAA conceived and designed research. LAA, FYA and AAE conducted experiments. LAA, EAS and FYA analyzed data. LAA and FYA wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethical Approval
All procedures performed in this study were conducted in accordance with the regulations approved by the Ethics Committee at Faculty of Pharmacy, Cairo University (permit number:1776). The investigation complied with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 2011).
Additional information
Handling editor: Y. James Kang.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ahmed, L.A., Abdou, F.Y., El Fiky, A.A. et al. Bradykinin-Potentiating Activity of a Gamma-Irradiated Bioactive Fraction Isolated from Scorpion (Leiurus quinquestriatus) Venom in Rats with Doxorubicin-Induced Acute Cardiotoxicity: Favorable Modulation of Oxidative Stress and Inflammatory, Fibrogenic and Apoptotic Pathways. Cardiovasc Toxicol 21, 127–141 (2021). https://doi.org/10.1007/s12012-020-09602-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12012-020-09602-5