Abstract
Purpose of Review
Enhanced recovery pathways are a well-described perioperative healthcare program involving evidence-based interventions. Enhanced recovery is designed to standardize techniques such as drug selection and nerve blocks in order to speed recovery and reduce overall hospital costs.
Recent Findings
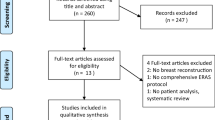
A PubMed literature search was performed for articles that included the terms enhanced recovery and breast reconstruction surgery. The present investigation summarizes enhanced recovery literature related to breast surgery with a focus on breast reconstruction.
Summary
Enhanced recovery considerations discussed in this review include patient education, preadmission optimization, perforator flap planning, anesthetic techniques, optimized fasting, venous thrombosis prophylaxis, early mobilization, and antimicrobial prophylaxis.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
•• Temple-Oberle C, Shea-Budgell MA, Tan M, Semple JL, Schrag C, Barreto M, et al. Consensus review of optimal perioperative care in breast reconstruction: Enhanced Recovery After Surgery (ERAS) Society recommendations. Plast Reconstr Surg. 2017;139:1056e–71e. https://doi.org/10.1097/PRS.0000000000003242. Excellent review of enhanced recovery after surgery for optimal perioperative care in breast reconstruction.
Temple-Oberle C, Ayeni O, Webb C, Bettger-Hahn M, Ayeni O, Mychailyshyn N. Shared decision-making: applying a person-centered approach to tailored breast reconstruction information provides high satisfaction across a variety of breast reconstruction options. J Surg Oncol. 2014;110:796–800. https://doi.org/10.1002/jso.23721.
Gregg JR, Cookson MS, Phillips S, Salem S, Chang SS, Clark PE, et al. Effect of preoperative nutritional deficiency on mortality after radical cystectomy for bladder cancer. J Urol. 2011;185:90–6. https://doi.org/10.1016/j.juro.2010.09.021.
Nguyen TJ, Costa MA, Vidar EN, Shahabi A, Peric M, Hernandez AM, et al. Effect of immediate reconstruction on postmastectomy surgical site infection. Ann Surg. 2012;256:326–33. https://doi.org/10.1097/SLA.0b013e3182602bb7.
Lee K-T, Mun G-H. Effects of obesity on postoperative complications after breast reconstruction using free muscle-sparing transverse rectus abdominis myocutaneous, deep inferior epigastric perforator, and superficial inferior epigastric artery flap. Ann Plast Surg. 2016;76:576–84. https://doi.org/10.1097/SAP.0000000000000400.
Ohkuma R, Mohan R, Baltodano PA, Lacayo MJ, Broyles JM, Schneider EB, et al. Abdominally based free flap planning in breast reconstruction with computed tomographic angiography. Plast Reconstr Surg. 2014;133:483–94. https://doi.org/10.1097/01.prs.0000438058.44505.d8.
•• Brady MC, Kinn S, Stuart P, Ness V. Preoperative fasting for adults to prevent perioperative complications. In: Brady MC, editor. Cochrane Database Syst. Rev., Chichester, UK: John Wiley & Sons, Ltd; 2003, p. CD004423. https://doi.org/10.1002/14651858.CD004423. Excellent review of preoperative fasting for adults to prevent perioperative complications.
Parameters P. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017;126:376–93. https://doi.org/10.1097/ALN.0000000000001452.
•• Feldheiser A, Aziz O, Baldini G, Cox BPBW, Fearon KCH, Feldman LS, et al. Enhanced Recovery After Surgery (ERAS) for gastrointestinal surgery, part 2: consensus statement for anaesthesia practice. Acta Anaesthesiol Scand. 2016;60:289–334. https://doi.org/10.1111/aas.12651. Excellent review of enhanced recovery after surgery for gastrointestinal surgery.
Bilku D, Dennison A, Hall T, Metcalfe M, Garcea G. Role of preoperative carbohydrate loading: a systematic review. Ann R Coll Surg Engl. 2014;96:15–22. https://doi.org/10.1308/003588414X13824511650614.
Noblett SE, Watson DS, Huong H, Davison B, Hainsworth PJ, Horgan AF. Pre-operative oral carbohydrate loading in colorectal surgery: a randomized controlled trial. Color Dis. 2006;8:563–9. https://doi.org/10.1111/j.1463-1318.2006.00965.x.
GUSTAFSSON UO, NYGREN J, THORELL A, SOOP M, HELLSTRÖM PM, LJUNGQVIST O, et al. Pre-operative carbohydrate loading may be used in type 2 diabetes patients. Acta Anaesthesiol Scand. 2008;52:946–51. https://doi.org/10.1111/j.1399-6576.2008.01599.x.
Nwaogu I, Yan Y, Margenthaler JA, Myckatyn TM. Venous thromboembolism after breast reconstruction in patients undergoing breast surgery: an American College of Surgeons NSQIP analysis. J Am Coll Surg. 2015;220:886–93. https://doi.org/10.1016/j.jamcollsurg.2015.01.031.
Murphy RX, Alderman A, Gutowski K, Kerrigan C, Rosolowski K, Schechter L, et al. Evidence-based practices for thromboembolism prevention. Plast Reconstr Surg. 2012;130:168e–75e. https://doi.org/10.1097/PRS.0b013e318254b4ee.
Patiar S, Kirwan CC, McDowell G, Bundred NJ, McCollum CN, Byrne GJ. Prevention of venous thromboembolism in surgical patients with breast cancer. Br J Surg. 2007;94:412–20. https://doi.org/10.1002/bjs.5782.
Olsen MA, Nickel KB, Fox IK, Margenthaler JA, Ball KE, Mines D, et al. Incidence of surgical site infection following mastectomy with and without immediate reconstruction using private insurer claims data. Infect Control Hosp Epidemiol. 2015;36:907–14. https://doi.org/10.1017/ice.2015.108.
Drinane JJ, Bergman RS, Folkers BL, Kortes MJ. Revisiting triple antibiotic irrigation of breast implant pockets. Plast Reconstr Surg Glob Open. 2013;1:e55. https://doi.org/10.1097/GOX.0b013e3182aa8760.
Jain S, Gupta P. Postoperative nausea and vomiting prophylaxis: a comparative study of ondansetron, granisetron and granisetron and dexamethasone combination after modified radical mastectomy. Saudi J Anaesth. 2014;8:67. https://doi.org/10.4103/1658-354X.144081.
Sinha AC, Singh PM, Williams NW, Ochroch EA, Goudra BG. Aprepitant’s prophylactic efficacy in decreasing postoperative nausea and vomiting in morbidly obese patients undergoing bariatric surgery. Obes Surg. 2014;24:225–31. https://doi.org/10.1007/s11695-013-1065-1.
Vallejo MC, Phelps AL, Ibinson JW, Barnes LR, Milord PJ, Romeo RC, et al. Aprepitant plus ondansetron compared with ondansetron alone in reducing postoperative nausea and vomiting in ambulatory patients undergoing plastic surgery. Plast Reconstr Surg. 2012;129:519–26. https://doi.org/10.1097/PRS.0b013e31822b6932.
•• McEvoy MD, Scott MJ, Gordon DB, Grant SA, Thacker JKM, Wu CL, et al. American Society for Enhanced Recovery (ASER) and Perioperative Quality Initiative (POQI) joint consensus statement on optimal analgesia within an enhanced recovery pathway for colorectal surgery: part 1—from the preoperative period to PACU. Perioper Med. 2017;6:8. https://doi.org/10.1186/s13741-017-0064-5. Excellent joint consensus statement on optimal analgesia within an enhanced recovery pathway for colorectal surgery.
Mathew P, Yaddanapudi S, Sehgal S, Grover V. A single dose of preoperative gabapentin for pain reduction and requirement of morphine after total mastectomy and axillary dissection: randomized placebo-controlled double-blind trial. J Postgrad Med. 2009;55:257. https://doi.org/10.4103/0022-3859.58928.
Sun M, Liao Q, Wen L, Yan X, Zhang F, Ouyang W. Effect of perioperative intravenous flurbiprofen axetil on chronic postmastectomy pain. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2013;38:653–60. https://doi.org/10.3969/j.issn.1672-7347.2013.07.001.
Riest G, Peters J, Weiss M, Pospiech J, Hoffmann O, Neuhäuser M, et al. Does perioperative administration of rofecoxib improve analgesia after spine, breast and orthopaedic surgery? Eur J Anaesthesiol. 2006;23:219–26. https://doi.org/10.1017/S026502150500222X.
Glissmeyer C, Johnson W, Sherman B, Glissmeyer M, Garreau J, Johnson N. Effect of paravertebral nerve blocks on narcotic use after mastectomy with reconstruction. Am J Surg. 2015;209:881–3. https://doi.org/10.1016/j.amjsurg.2015.01.013.
Zhong T, Ojha M, Bagher S, Butler K, Srinivas C, McCluskey SA, et al. Transversus abdominis plane block reduces morphine consumption in the early postoperative period following microsurgical abdominal tissue breast reconstruction. Plast Reconstr Surg. 2014;134:870–8. https://doi.org/10.1097/PRS.0000000000000613.
Yu H-P, Chen H-P, Hsu Y-H, Hua K-C, Lin C-C, Lo Y-F. Comparison of sevoflurane versus propofol under auditory evoked potential monitoring in female patients undergoing breast surgery. Biomed J. 2013;36:125. https://doi.org/10.4103/2319-4170.113228.
Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334:1209–15. https://doi.org/10.1056/NEJM199605093341901.
Warttig S, Alderson P, Campbell G, Smith AF. Interventions for treating inadvertent postoperative hypothermia. Cochrane Database Syst Rev 2014:CD009892. https://doi.org/10.1002/14651858.CD009892.pub2.
Scott EM, Buckland R. A systematic review of intraoperative warming to prevent postoperative complications. AORN J. 2006;83:1090–104 1107–13.
Nelson JA, Fischer JP, Grover R, Nelson P, Au A, Serletti JM, et al. Intraoperative vasopressors and thrombotic complications in free flap breast reconstruction. J Plast Surg Hand Surg. 2017;51:336–41. https://doi.org/10.1080/2000656X.2016.1269777.
Zhong T, Neinstein R, Massey C, McCluskey SA, Lipa J, Neligan P, et al. Intravenous fluid infusion rate in microsurgical breast reconstruction. Plast Reconstr Surg. 2011;128:1153–60. https://doi.org/10.1097/PRS.0b013e318221da56.
Booi DI. Perioperative fluid overload increases anastomosis thrombosis in the free TRAM flap used for breast reconstruction. Eur J Plast Surg. 2011;34:81–6. https://doi.org/10.1007/s00238-010-0466-9.
Lassen K, Kjæve J, Fetveit T, Tranø G, Sigurdsson HK, Horn A, et al. Allowing normal food at will after major upper gastrointestinal surgery does not increase morbidity. Ann Surg. 2008;247:721–9. https://doi.org/10.1097/SLA.0b013e31815cca68.
Andersen HK, Lewis SJ, Thomas S. Early enteral nutrition within 24h of colorectal surgery versus later commencement of feeding for postoperative complications. Cochrane Database Syst Rev 2006:CD004080. https://doi.org/10.1002/14651858.CD004080.pub2.
Whitaker I, Rozen W, Chubb D, Acosta R, Kiil B, Birke-Sorensen H, et al. Postoperative monitoring of free flaps in autologous breast reconstruction: a multicenter comparison of 398 flaps using clinical monitoring, microdialysis, and the implantable Doppler probe. J Reconstr Microsurg. 2010;26:409–16. https://doi.org/10.1055/s-0030-1249607.
Paddon-Jones D, Sheffield-Moore M, Cree MG, Hewlings SJ, Aarsland A, Wolfe RR, et al. Atrophy and impaired muscle protein synthesis during prolonged inactivity and stress. J Clin Endocrinol Metab. 2006;91:4836–41. https://doi.org/10.1210/jc.2006-0651.
Henriksen MG, Jensen MB, Hansen HV, Jespersen TW, Hessov I. Enforced mobilization, early oral feeding, and balanced analgesia improve convalescence after colorectal surgery. Nutrition. 2002;18:147–52.
Testa A, Iannace C, Di Libero L. Strengths of early physical rehabilitation programs in surgical breast cancer patients: results of a randomized controlled study. Eur J Phys Rehabil Med. 2014;50:275–84.
Author information
Authors and Affiliations
Contributions
The manuscript has been read and approved by all the authors, the requirements for authorship have been met, and each author believes that the manuscript represents honest work. All authors contributed equally to the manuscript and are involved in institutional protocols and policies for enhanced recovery pathways.
Corresponding author
Ethics declarations
Conflict of Interest
Amir Elhassan, Ahmed Ahmed, Hamdy Awad, Michelle Humeidan, Carmen L. Labrie-Brown, and Elyse M. Cornett declare no conflict of interest. Alan D. Kaye serves on the Speakers Bureau of Depomed and Merck. Richard D. Urman received research funding from Medtronic.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Other Pain
Rights and permissions
About this article
Cite this article
Elhassan, A., Ahmed, A., Awad, H. et al. Enhanced Recovery for Breast Reconstruction Surgery. Curr Pain Headache Rep 23, 27 (2019). https://doi.org/10.1007/s11916-019-0761-5
Published:
DOI: https://doi.org/10.1007/s11916-019-0761-5