Abstract
Purpose of Review
Vitamin D and its derivatives are biologically active fat-soluble steroid hormones, which are transcription factors for numerous genes. The results of several observational studies suggest the relationship between plasma concentration of vitamin D and the risk of arterial hypertension, as well as between the intensity of insolation and the risk of arterial hypertension.
Recent Findings
Based on the results of the abovementioned studies, it was hypothesized that vitamin D is characterized by the antihypertensive properties. Animal experiments have shown that vitamin D reduces activity of the renin-angiotensin-aldosterone system and improves vasorelaxation of blood vessels. Results of clinical studies did not confirm these results. Moreover in interventional clinical trials, it was documented that supplementation of vitamin D did not reduce blood pressure. The influence of exposure to sunshine at different wave lengths on blood pressure was examined in clinical studies and it was found that ultraviolet A radiation (UVA) lead to the release of nitric oxide from the skin. This might explain lower level of blood pressure in subjects from the regions with a higher rate of insolation.
Summary
The aim of this review is to summarize current knowledge concerning the relationship between vitamin D and arterial hypertension based on both observational and interventional studies.
Similar content being viewed by others
Introduction
The beginning interest in vitamin D goes back to 1822, when Polish scientist Jędrzej Śniadecki described the significant positive relationship between prevalence of rickets and insufficient exposure to solar radiation. It was based on the observation concerning the frequency of rickets in children living in the countryside and in cities [1]. In 1919, British physiologist Edward Mallenby discovered vitamin D and demonstrated the role of its deficiency in the pathogenesis of rickets. In the early 1920s, German chemist Adolf Windaus described the structure of vitamin D2 and vitamin D3 and developed a technology for their production by irradiating lanolin with ultraviolet (UV) rays. In 1928, he received the Nobel Prize in medicine and physiology for his work on steroid hormones. In 1937, the Merck company introduced vitamin D to the pharmaceutical market with the indication of the prevention and treatment of rickets.
Vitamin D and its derivatives are biologically active fat-soluble steroid hormones, which are transcription factors for numerous genes. About 80% of vitamin D is produced in the skin (Fig. 1). The source of the remaining 20% is food (food products with a high content of vitamin D are fish, offal, and egg yolks). In the skin, mainly in the keratinocytes of the epidermal reproductive layer and under the influence of ultraviolet B radiation (UVB), 7-dehydrocholesterol (7-DHC) is converted to previtamin D, and then to cholecalciferol (vitamin D3; calcyol). Cholecalciferol produced in the skin and ergocalciferol (vitamin D2) provided with food are hydroxylated in the liver by 25-hydroxylase to 25(OH)D2 and 25(OH)D3, i.e., calciphediols [25(OH)D]. Calciphediols are inactive prohormones. The calciphediols are a reserve form of vitamin D in the body. In the kidneys, as a result of 1-hydroxylation, active derivatives are formed: 1,25(OH)2D2 and 1,25(OH)2D3 (calcitriols; 1,25(OH)2D). Fifteen to twenty percent of the total amount of calcitriol is produced in the kidneys. The remaining 80% of calcitriol is synthetized in peripheral tissues in which 1-hydroxylase also occurs. Calcitriol produced by the kidneys is characterized as a circulating hormone with several endocrine effects (Fig. 1). As a result of 24-hydroxylation in the kidneys, biologically inactive vitamin D derivatives are also synthetized: 24,25(OH)2D2 and 24,25(OH)2D3 (collectively referred to as 24,25(OH)2D) and 1,24,25(OH)3D2 and 1,24,25(OH)3D3 (calcitetrols; 1,24,25(OH)3D) (Fig. 1). There are also hydroxylated metabolites in positions C-23 and C-26 in the blood. In total, over 20 different vitamin D derivatives are currently known [2, 3].
Vitamin D receptors (VDRs) are found in the cell nucleus (Fig. 1). VDR belongs to the family of genomic receptors for steroids, thyroid hormones, and retinoids. Stimulation of these receptors regulates gene expression of many proteins. Vitamin D receptors are found in most cells of the body, but those located in the small intestinal enterocytes are of major clinical importance. Activation of receptors in the small intestine leads to increased expression of the calcium-binding protein (CaBP) gene—calbindin—which increases the absorption of calcium in the gastrointestinal tract (Fig. 2). In addition, vitamin D enhances the expression of the inorganic phosphate cotransporter gene (NPT2b, sodium-dependent phosphate cotransporter 2b) by increasing the absorption of phosphate from the gastrointestinal tract (Fig. 2) [4,5,6].
Vitamin D increases the absorption of calcium and phosphate in the small intestine. VDBG - vitamin D-binding globulin; PMCA1b - plasma membrane Ca2+ ATPase 1b; VDR - vitamin D receptor; TRPV6 - transient receptor potential cation channel subfamily V member; NPT2b - sodium-dependent phosphate cotransporter 2b
Vitamin D and Arterial Hypertension—Results of Observational Studies
The results of numerous observational studies suggest a relationship between plasma 25(OH)D concentration and the risk of hypertension. According to data from the National Health and Nutrition Examination Survey (NHANES) study conducted in 2001–2004, subjects with low 25(OH)D plasma levels are characterized by an increased incidence of hypertension [7]. A meta-analysis of the results of 19 studies (90, 535 subjects) analyzing the relationship of vitamin D plasma concentration and risk of hypertension showed that hypertension is more frequent in subjects with low 25(OH)D plasma concentration [8]. Yilmaz et al. compared plasma vitamin D concentration in 100 patients with hypertension and no physiological blood pressure reduction at night (non-dippers) and 100 patients with hypertension and physiological reduction of blood pressure at night (dippers). Plasma vitamin D concentrations were significantly lower in subjects characterized as non-dippers [9]. Another meta-analysis of the results from 10 prospective studies including 48, 633 subjects showed that high plasma vitamin D concentration reduces the risk of new-onset hypertension [10]. Recently, it has also been shown that lower plasma vitamin D concentrations in the plasma are more frequent in patients with resistant hypertension [11].
In addition, the results of observational studies suggest a relationship between the intensity of sunlight and the risk of hypertension. Rostand showed elevated blood pressure in subjects living in areas with higher distances from the equator, i.e., in regions with less sunlight [12]. In the Reasons for Racial and Geographic Differences in Stroke (REGARDS) study, which involved 1104 participants, the effects of exposure to sunlight and blood pressure were assessed. A negative relationship was found between sunlight exposure and systolic blood pressure. In addition, plasma vitamin D concentrations did not affect the relationship between sunlight exposure and blood pressure [13]. Brennan et al., in a study performed in the UK, found that blood pressures in both normotensive subjects and hypertensive patients are higher during the winter [14]. As already mentioned above, vitamin D is mainly produced in the skin during exposure to UVB radiation, which explains the fact that the plasma concentration of 25(OH)D is higher in subjects living in areas with more intensive sunlight exposure, i.e., closer to the equator. Therefore, it was hypothesized that the relationship between sunlight and blood pressure is associated with the antihypertensive properties of vitamin D.
Potential Mechanisms of the Antihypertensive Effect of Vitamin D
In experimental studies, vitamin D has been shown to have antihypertensive properties. It has been shown that mice lacking the VDR gene (VDR-knockout mice) are characterized by increased expression of the renin gene, which leads to an increased activity of the renin-angiotensin-aldosterone system. These mice were characterized by elevated blood pressure and heart failure. In addition, in wild-type mice, a decrease in vitamin D production (by administering strontium that inhibits calcitriol production) led to an increase of renin secretion. Additionally, it was shown that the administration of vitamin D reduced the expression of the renin gene in mice treated with strontium [15, 16]. Ni et al., in a study performed in VDR-knockout mice, showed that the maximum diastole of the isolated aorta, stimulated with acetylcholine, was reduced compared with wild-type mice. In addition, endothelial nitric oxide synthase (eNOS) expression was reduced in mice lacking the VDR gene. Moreover, endothelin-1 (ET-1) expression and sensitivity to the angiotensin II hypertensinogenic properties are increased in these VDR-knockout mice. Vitamin D has been found to increase vasoconstrictive properties of the vascular endothelium by increasing eNOS gene expression and by reducing ET-1 gene expression [17]. In studies in VDR-knockout mice, vitamin D has been shown to be a direct transcriptional regulator of eNOS [18]. Tare et al. studied the effect of vitamin D deficiency in the diet on vascular endothelial function in 7–8-week-old rats. It was found that the mesenteric artery of rats with vitamin D deficiency was characterized by a 2 times lower ability to relax by way of nitric oxide and endothelial hyperpolarizing factor (EDHF), which was assessed by measuring arterial pressure in the mesenteric artery using an intravascular catheter [19]. In another study, it was also found that vitamin D inhibited angiotensin II and endothelin-1 stimulated growth of adult rat aortic smooth muscle cells [20].
To confirm the results of studies in experimental animals that showed the effect of vitamin D on the renin-angiotensin-aldosterone system and on endothelial function, interventional clinical studies were carried out. In one of them, 84 patients with overweight or obesity with 25(OH)D plasma concentration < 20 ng/ml were treated with ergocalciferol (vitamin D2) in a dose of 50, 000 units per week vs. placebo. After 8 weeks of administration of ergocalciferol, there was a significant increase in plasma 25(OH)D concentration of 15 ng/ml compared with the placebo. However, ergocalciferol did not influence the plasma renin activity and plasma angiotensin II concentrations [21]. In addition, vitamin D administration in these patients did not influence the endothelium-dependent relaxation of the brachial artery [22]. Beveridge et al. performed a meta-analysis of 31 studies including 2751 subjects. During these studies, subjects were given vitamin D for 4 weeks–12 months, in a vitamin D dose of 900–5000 IU/day. No significant effect of vitamin D administration on endothelium-dependent brachial artery and pulse rate could be demonstrated [23].
Thus, the results of the above cited interventional clinical studies did not confirm the influence of vitamin D on mechanisms involved in blood pressure regulation.
Vitamin D and Hypertension—Results of Clinical Interventional Studies
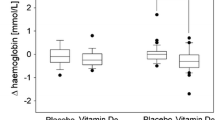
Observational studies were not able to show a causal relationship. Therefore, the results of such studies cited above led to clinical interventional studies aimed at determining whether vitamin D affects blood pressure. In the largest randomized intervention study to date, carried out by Arora et al. in 2015, the effect of cholecalciferol administration on blood pressure was studied. Five hundred and thirty-four subjects with antihypertensive therapy or 1st degree hypertension subjects who did not take antihypertensive drugs were eligible for the study. At the beginning of the study, the systolic blood pressure of the subjects was in the range of 120–159 mmHg. In addition, all subjects are characterized by 25(OH)D plasma concentrations less or equal to 25 ng/ml. The subjects were treated with cholecalciferol in doses of 400 IU/day vs. 4000 IU/day. After 6 months, an increase in plasma vitamin D concentration was demonstrated. However, no effect of cholecalciferol administration on blood pressure measured in a 24-h measurement (ABPM), as well as an office blood pressure, was found [24]. A meta-analysis of 46 prospective interventional studies with a follow-up of more than 4 weeks analyzing the effect of vitamin D administration vs. placebo on blood pressure in 4541 subjects was published by Beveridge et al. [25••]. The authors could not document that supplementation of vitamin D affects either SBP (systolic blood pressure) or DBP (diastolic blood pressure). In addition, the authors did not select a subgroup of patients where administration of vitamin D might reduce blood pressure [25••]. Qi et al. performed a meta-analysis of data from 8 randomized studies involving 917 patients [26••]. The effect of vitamin D administration vs. placebo on blood pressure after more than 3 months was analyzed. Compared with placebo, there was no statistical difference in reducing systolic blood pressure by vitamin D supplementation [26••]. A meta-analysis of 17 randomized clinical trials, involving 1687 subjects, performed by He et al., evaluated the effect of vitamin D administration on blood pressure in subjects with plasma vitamin D concentration < 20 ng/ml. No significant differences were found in both SBP and DBP between the group receiving vitamin D and the control group. In the summary of the study, the authors indicate that oral administration of vitamin D does not affect blood pressure in subjects with a plasma vitamin D concentration at the beginning of the study of < 20 ng/ml [27••].
Mose et al. evaluated in a randomized, double-blind, placebo-controlled study the effect of cholecalciferol administration on blood pressure in dialysed patients with chronic kidney diseases. The study completed 50 patients who received cholecalciferol at a dose of 3000 IU/day or placebo for 6 months. Cholecalciferol administration did not influence blood pressure measured with ABPM method in these patients [28•].
Thus, results from clinical trials did not show antihypertensive properties of vitamin D supplementation.
How Is It Possible to Explain the Relationship Between Low Vitamin D Plasma Concentration and an Increased Risk of Hypertension Found in the Observational Studies?
Observational studies have shown that hypertension is one and a half to five times more common in obese patients than in subjects with normal body weight [29,30,31]. Analysis of the data from the Framingham Heart Study showed that as many as in 78% of men and in 65% of women hypertension is directly associated with obesity [32]. In the Physician Health Study 13, 563 healthy men were observed for 15 years. It was found that a body weight increase of 10% leads to an increased risk of hypertension by as much as 70% [33]. Mathieu et al. analyzed the relationship between plasma vitamin D concentration and body fat content (Fig. 3). In a study of 271 subjects older than 60 years of age, it was shown that lower 25(OH)D plasma concentration is associated with higher fat mass [34•]. Turer et al. conducted a study in which over 12,000 children aged 6–18 participating in the National Health and Nutrition Examination Survey (NHANES) 2003–2006 study were analyzed. The subjects were divided into 4 groups: with healthy weight, overweight, obesity, and severe obesity. It was demonstrated that a plasma 25(OH)D concentration lower than 20 ng/ml occurred in 21% of children with normal body weight, in 29% of overweight children, in 34% children with obesity, and in 49% children with severe obesity (Fig. 4) [35•]. Rock et al. assessed the effect of body weight changes on plasma 25(OH)D concentration in 383 overweight or obese women who participated in a 2-year obesity treatment program (reduced energy diet and moderate physical activity for 30 min at least 5 days a week). It has been shown that in obese women who decreased body weight by 5–10%, the 25(OH)D plasma concentration increased by 2.7 ng/ml. In women who reduced body weight by more than 15%, the plasma 25(OH)D concentration increased by 6 ng/ml. In addition, it was found that in women who increased body weight by more than 10%, the 25(OH)D plasma concentration decreased by 3.9 ng/ml (Fig. 5) [36•]. Taking the results of the above studies, into account, the cause of low vitamin D plasma concentrations in obese subjects seems to be that fat-soluble vitamin D is accumulated in adipose tissue. Thus, the higher incidence of hypertension demonstrated in observational studies in subjects with low vitamin D plasma concentrations might only be the result of lower vitamin D plasma concentrations in obese subjects who are strongly predisposed to arterial hypertension (Fig. 6).
Serum vitamin D concentration in obese patients. Based on [34]
Body weight and frequency of plasma 25(OH)D concentration < 20 ng/ml in children. BMI – body mass index. Based on [35•]
Effect of body weight change on plasma 25(OH)D concentration in overweight or obese women. Based on [36•]
How Is It Possible to Explain the Relationship Between Exposure to Sunlight and Reduced Incidence of Hypertension Found in the Observational Study?
Ultraviolet radiation emitted by the sun reaches the Earth mainly in the form of ultraviolet A radiation (UVA, 315–400 nm wavelength radiation) and, to a lesser extent, UVB radiation (280–315 nm wavelength). The effect of UV radiation on vitamin D metabolism in hypertensive patients was the subject of the clinical study performed in our department in the late 1980s [37]. More recently, to determine the effect of an increase in endogenous vitamin D synthesis, on blood pressure, stimulating by sunlight, an interventional clinical study was conducted.
Scragg et al. published a study in which 58 healthy individuals were exposed twice weekly for 12 weeks to UVB radiation. In this study, after using the above described intervention, an increase of plasma 25(OH)D concentration from 17 to 37 ng/ml was observed. However, both systolic and diastolic blood pressure did not change [38•]. To explain the relationship between solar radiation and blood pressure, another part of the sunlight spectrum—UVA radiation—was examined. A study was conducted in 7 healthy subjects who were exposed to UVA radiation for 15 min. UVA radiation has been found to reduce blood pressure. This hypotensive effect lasted for over an hour and was associated with an increase in plasma nitric oxide (NO) concentration [39•]. In subsequent experiments, the skin was incubated in vitro with fluorochrome NO under the influence of UVA radiation and the release of NO into the circulation could be observed. In addition, it has been shown that the observed increase of NO concentration in the dermis is not dependent on nitric oxide synthase activity [40]. An increase in NO plasma concentration under the influence of UVA radiation is associated with the release of NO into circulation from depots that are located in the dermis (Fig. 7) [41]. Results from the experimental studies indicate that the release of NO stored in the dermis under the influence of UVA radiation leads to vasorelaxation and to blood pressure reduction. Taking into account the above data, it appears that stimulation of vitamin D production in the skin under the influence of sunlight has no effect on blood pressure. The effect of sunlight on arterial pressure is only associated with the NO release in the dermis under the influence of UVA radiation.
Conclusions
-
1.
Experimental and observational studies may suggest the role of vitamin D in the pathogenesis of hypertension.
-
2.
Prospective clinical studies did not confirm that vitamin D supplementation exerts any antihypertensive properties.
-
3.
Antihypertensive effect of sunlight was not associated with increased vitamin D plasma concentrations but was rather due to the release of nitric oxide in the skin.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Rutkowski B, Ostrowski J. Jędrzej Śniadecki (1768-1838) and his flirtation with nephrology. J Nephrol. 2013;26:40–4.
Al Mheid I, Patel RS, Tangpricha V, Quyyumi AA. Vitamin D and cardiovascular disease: is the evidence solid? Eur Heart J. 2013;34:3691–8.
Ramagopalan SV, Heger A, Berlanga AJ, Maugeri NJ, Lincoln MR, Burrell A, et al. A ChIP-seq defined genome-wide map of vitamin D receptor binding: associations with disease and evolution. Genome Res. 2010;20:1352–60.
Cozzolino M. Vitamin D: something new under the sun. Clin Kidney J. 2012;5:285–7.
Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr. 2004;80:1678–88.
Rojas-Rivera J, De La Piedra C, Ramos A, Ortiz A, Egido J. The expanding spectrum of biological actions of vitamin D. Nephrol Dial Transplant. 2010;25:2850–65.
Kim DH, Sabour S, Sagar UN, Adams S, Whellan DJ. Prevalence of hypovitaminosis D in cardiovascular diseases (from the National Health and Nutrition Examination Survey 2001 to 2004). Am J Cardiol. 2008;102:1540–4.
Ke L, Mason RS, Kariuki M, Mpofu E, Brock KE. Vitamin D status and hypertension: a review. Integr Blood Press Control. 2015;8:13–35.
Yilmaz S, Sen F, Ozeke O, Temizhan A, Topaloglu S, Aras D, et al. The relationship between vitamin D levels and non-dipper hypertension. Blood Press Monit. 2015;20:330–4.
Kunutsor SK, Burgess S, Munroe PB, Khan H. Vitamin D and high blood pressure: causal association or epiphenomenon? Eur J Epidemiol. 2014;29:1–14.
Del Pinto R, Wright JT, Monaco A, Pietropaoli D, Ferri C. Vitamin D and blood pressure control among hypertensive adults: results from NHANES 2001-2014. J Hypertens. 2020;38:150–8.
Rostand SG. Ultraviolet light may contribute to geographic and racial blood pressure differences. Hypertension. 1997;2:150–6.
Rostand SG, McClure LA, Kent ST, Judd SE, Gutiérrez OM. Associations of blood pressure, sunlight, and vitamin D in community-dwelling adults. J Hypertens. 2016;34:1704–10.
Brennan PJ, Greenberg G, Miall WE, Thompson SG. Seasonal variation in arterial blood pressure. Br Med J. 1982;285:919–23.
Li YC, Kong J, Wei M, Chen ZF, Liu SQ, Cao LP. 1,25-Dihydroxyvitamin D(3) is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest. 2002;110:229–38.
Rousselet F, El Solh N, Maurat JP, Gruson M, Girard ML. Strontium and calcium metabolism. Interaction of strontium and vitamin D. C R Seances Soc Biol Fil. 1975;169:322–9.
Ni W, Watts SW, Ng M, Chen S, Glenn DJ, Gardner DG. Elimination of vitamin D receptor in vascular endothelial cells alters vascular function. Hypertension. 2014;64:1290–8.
Andrukhova O, Slavic S, Zeitz U, Riesen SC, Heppelmann MS, Ambrisko TD, et al. Vitamin D is a regulator of endothelial nitric oxide synthase and arterial stiffness in mice. Mol Endocrinol. 2014;28:53–64.
Tare M, Emmett SJ, Coleman HA, Skordilis C, Eyles DW, Morley R, et al. Vitamin D insufficiency is associated with impaired vascular endothelial and smooth muscle function and hypertension in young rats. J Physiol. 2011;589:4777–86.
Chen S, Law CS, Grigsby CL, Olsen K, Gardner DG. A role for the cell cycle phosphatase Cdc25a in vitamin D-dependent inhibition of adult rat vascular smooth muscle cell proliferation. J Steroid Biochem Mol Biol. 2010;122:326–32.
McMullan CJ, Borgi L, Curhan GC, Fisher N, Forman JP. The effect of vitamin D on renin-angiotensin system activation and blood pressure: a randomized control trial. J Hypertens. 2017;35:822–9.
Borgi L, McMullan C, Wohlhueter A, Curhan GC, Fisher ND, Forman JP. Effect of vitamin D on endothelial function: a randomized, double-blind, placebo-controlled trial. Am J Hypertens. 2017;30:124–9.
Beveridge LA, Khan F, Struthers AD, Armitage J, Barchetta I, Bressendorff I, et al. Effect of vitamin D supplementation on markers of vascular functions: a systematic review and individual participant meta-analysis. J Am Heart Assoc. 2018;7:e008273.
Arora P, Song Y, Dusek J, Plotnikoff G, Sabatine MS, Cheng S, et al. Vitamin D therapy in individuals with prehypertension or hypertension: the DAYLIGHT trial. Circulation. 2015;131:254–62.
•• Beveridge LA, Struthers AD, Khan F, Jorde R, Scragg R, Macdonald HM, et al. Effect of vitamin D supplementation on blood pressure: a systematic review and meta-analysis incorporating individual patient data. JAMA Intern Med. 2015;175:745–54 Meta-analysis of 46 prospective interventional clinical studies demonstrated that vitamin D treatment did not lead to the reduction in blood pressure.
•• Qi D, Nie X, Cai J. The effect of vitamin D supplementation on hypertension in non-CKD populations: a systemic review and meta-analysis. Int J Cardiol. 2017;227:177–86 Meta-analysis of data from 8 randomized interventional clinical studies demonstrated that vitamin D did not exhibit antihypertensive properties.
•• He S, Hao X. The effect of vitamin D3 on blood pressure in people with vitamin D deficiency: a system review and meta-analysis. Medicine. 2019;98:e15284 Meta-analysis of 17 randomized clinical trials evaluated the effect of vitamin D administration on blood pressure in subjects with serum vitamin D concentration < 20 ng/ml. No significant differences were found in both SBP and DBP between subjects receiving vitamin D and the control group.
• Mose FH, Vase H, Larsen T, Kancir AS, Kosierkiewic R, Jonczy B, et al. Cardiovascular effects of cholecalciferol treatment in dialysis patients–a randomized controlled trial. BMC Nephrol. 2014;15:50 Clinical study demonstrated that administration of cholecalciferol in dialysed patients with chronic kidney disease did not affect blood pressure.
Tsujimoto T, Sairenchi T, Iso H, Irie F, Yamagishi K, Tanaka K, et al. Impact of obesity on incident hypertension independent of weight gain among nonhypertensive Japanese: the Ibaraki Prefectural Health Study (IPHS). J Hypertens. 2012;30:1122–8.
Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J Am Coll Surg. 2008;207:928–34.
Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–9.
Garrison RJ, Kannel WB, Stokes J 3rd, Castelli WP. Incidence and precursors of hypertension in young adults: the Framingham Offspring Study. Prev Med. 1987;16:235–51.
Gelber RP, Gaziano JM, Manson JE, Buring JE, Sesso HD. A prospective study of body mass index and the risk of developing hypertension in men. Am J Hypertens. 2007;20:370–7.
• Mathieu SV, Fischer K, Dawson-Hughes B, Freystaetter G, Beuschlein F, Schietzel S, et al. Association between 25-hydroxyvitamin D status and components of body composition and glucose metabolism in older men and women. Nutrients. 2018;10:E1826 Observational study demonstrated that lower serum 25(OH)D levels may be associated with higher body fat content.
• Turer CB, Lin H, Flores G. Prevalence of vitamin D deficiency among overweight and obese US children. Pediatrics. 2013;131:152–61 Observational study demonstrated that the prevalence vitamin D deficiency is higher in overweight and obese than in normal weight children.
• Rock CL, Emond JA, Flatt SW, Heath DD, Karanja N, Pakiz B, et al. Weight loss is associated with increased serum 25-hydroxyvitamin D in overweight or obese women. Obesity (Silver Spring). 2012;20:2296–301 Clinical study performed in overweight or obese females demonstrated that weight loss is associated with an increase of serum 25(OH)D concentration.
Kokot F, Schmidt-Gayk H, Wiecek A, Mleczko Z, Bracel B. Influence of ultraviolet irradiation on plasma vitamin D and calcitonin levels in humans. Kidney Int Suppl. 1989;27:143–6.
• Scragg R, Wishart J, Stewart A, Ofanoa M, Kerse N, Dyall L, et al. No effect of ultraviolet radiation on blood pressure and other cardiovascular risk factors. J Hypertens. 2011;29:1749–56 Interventional clinical study demonstrated that UVB radiation did not change blood pressure.
• Opländer C, Volkmar CM, Paunel-Görgülü A, van Faassen EE, Heiss C, Kelm M, et al. Whole body UVA irradiation lowers systemic blood pressure by release of nitric oxide from intracutaneous photolabile nitric oxide derivates. Circ Res. 2009;105:1031–40 Interventional clinical study demonstrated that UVA radiation reduced blood pressure. This hypotensive effect was associated with an increase in plasma nitric oxide concentration.
Liu D, Fernandez BO, Hamilton A, Lang NN, Gallagher JMC, Newby DE, et al. UVA irradiation of human skin vasodilates arterial vasculature and lowers blood pressure independently of nitric oxide synthase. Invest Dermatol. 2014;134:1839–46.
Feelisch M, Kolb-Bachofen V, Liu D, Lundberg JO, Revelo LP, Suschek CV, et al. Is sunlight good for our heart? Eur Heart J. 2010;31:1041–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Hypertension and Obesity
Rights and permissions
About this article
Cite this article
Adamczak, M., Surma, S. & Więcek, A. Vitamin D and Arterial Hypertension: Facts and Myths. Curr Hypertens Rep 22, 57 (2020). https://doi.org/10.1007/s11906-020-01059-9
Published:
DOI: https://doi.org/10.1007/s11906-020-01059-9