Abstract
Purpose of Review
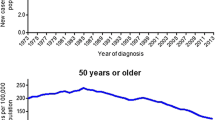
While the incidence and mortality of colorectal cancer have been declining in the USA in the last decades, there is a considerable increase in the incidence of this malignancy in the young adult patients. Several environmental and genetic factors have been studied and known to be associated with colorectal cancer. However, the exact causes of this increase are not clear. Therefore, in this review, we aimed to provide insights in terms of novel findings and avenues of research that may lead to a better way to treat this population of patients.
Recent Findings
Obesity and its associated behaviors, such as unhealthy dietary patterns and sedentary lifestyles, as well as gut microbiota may play a crucial role in colorectal cancer (CRC) risk for young adults. Recently, the American Cancer Society recommends that adults aged 45 years and older with an average risk of CRC undergo regular screening with either a high-sensitivity stool-based test or a structural examination, depending on patient preference and test availability. It is important to note that data on outcomes associated with systemic cytotoxic and biologic therapy specifically in young patients with CRC are lacking.
Summary
In this review, we provide an overview on the most recent evidence regarding incidence, screening, molecular features, and management of young patients with colorectal cancer.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major Importance
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30.
Siegel RL, Fedewa SA, Anderson WF, Miller KD, Ma J, Rosenberg PS, Jemal A Colorectal cancer incidence patterns in the United States, 1974-2013. J Natl Cancer Inst 2017; 109.
Mork ME, You YN, Ying J, Bannon SA, Lynch PM, Rodriguez-Bigas MA, et al. High prevalence of hereditary cancer syndromes in adolescents and young adults with colorectal cancer. J Clin Oncol. 2015;33:3544–9.
Pearlman R, Frankel WL, Swanson B, Zhao W, Yilmaz A, Miller K, et al. Prevalence and spectrum of germline cancer susceptibility gene mutations among patients with early-onset colorectal cancer. JAMA Oncol. 2017;3:464–71.
Moore HG. Colorectal cancer: what should patients and families be told to lower the risk of colorectal cancer? Surg Oncol Clin N Am. 2010;19:693–710.
Islami F, Goding Sauer A, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018;68:31–54.
Karahalios A, English DR, Simpson JA. Weight change and risk of colorectal cancer: a systematic review and meta-analysis. Am J Epidemiol. 2015;181:832–45.
Hidayat K, Yang CM, Shi BM. Body fatness at an early age and risk of colorectal cancer. Int J Cancer. 2018;142:729–40.
Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer. 2004;4:579–91.
Ma J, Pollak MN, Giovannucci E, Chan JM, Tao Y, Hennekens CH, et al. Prospective study of colorectal cancer risk in men and plasma levels of insulin-like growth factor (IGF)-I and IGF-binding protein-3. J Natl Cancer Inst. 1999;91:620–5.
McSkane M, Stintzing S, Heinemann V, Puccini A, Naseem M, Cao S, et al. Association between height and clinical outcome in metastatic colorectal cancer patients enrolled onto a randomized phase 3 clinical trial: data from the FIRE-3 study. Clin Colorectal Cancer. 2018;
de Kort S, Masclee AAM, Sanduleanu S, Weijenberg MP, van Herk-Sukel MPP, Oldenhof NJJ, et al. Higher risk of colorectal cancer in patients with newly diagnosed diabetes mellitus before the age of colorectal cancer screening initiation. Sci Rep. 2017;7:46527.
Aleksandrova K, Boeing H, Jenab M, Bas Bueno-de-Mesquita H, Jansen E, van Duijnhoven FJB, et al. Metabolic syndrome and risks of colon and rectal cancer: the European prospective investigation into cancer and nutrition study. Cancer Prev Res (Phila). 2011;4:1873–83.
Whitmore L, Wallace BA. DICHROWEB, an online server for protein secondary structure analyses from circular dichroism spectroscopic data. Nucleic Acids Res. 2004;32:W668–73.
O’Keefe SJ, Li JV, Lahti L, et al. Fat, fibre and cancer risk in African Americans and rural Africans. Nat Commun. 2015;6:6342.
Greer JB, O’Keefe SJ. Microbial induction of immunity, inflammation, and cancer. Front Physiol. 2011;1:168.
Bordonaro M, Lazarova DL, Sartorelli AC. Butyrate and Wnt signaling: a possible solution to the puzzle of dietary fiber and colon cancer risk? Cell Cycle. 2008;7:1178–83.
Raskov H, Burcharth J, Pommergaard HC. Linking gut microbiota to colorectal cancer. J Cancer. 2017;8:3378–95.
Guidelines N. Genetic/familial high-risk assessment: colorectal. Accessed January 10th 2018.
Weinberg BA, Marshall JL, Salem ME. The growing challenge of young adults with colorectal cancer. Oncology (Williston Park). 2017;31:381–9.
Moreira L, Balaguer F, Lindor N, de la Chapelle A, Hampel H, Aaltonen LA, et al. Identification of Lynch syndrome among patients with colorectal cancer. JAMA. 2012;308:1555–65.
Umar A, Boland CR, Terdiman JP, Syngal S, Chapelle A, Ruschoff J, et al. Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst. 2004;96:261–8.
Le DT, Durham JN, Smith KN, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357:409–13.
Burn J, Gerdes AM, Macrae F, Mecklin JP, Moeslein G, Olschwang S, et al. Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomised controlled trial. Lancet. 2011;378:2081–7.
Galiatsatos P, Foulkes WD. Familial adenomatous polyposis. Am J Gastroenterol. 2006;101:385–98.
Half E, Bercovich D, Rozen P. Familial adenomatous polyposis. Orphanet J Rare Dis. 2009;4:22.
Aretz S, Uhlhaas S, Caspari R, Mangold E, Pagenstecher C, Propping P, et al. Frequency and parental origin of de novo APC mutations in familial adenomatous polyposis. Eur J Hum Genet. 2004;12:52–8.
Murphy CC, Sanoff HK, Stitzenberg KB, Baron JA, Sandler RS, Yang YC, et al. RE: colorectal cancer incidence patterns in the United States, 1974-2013. J Natl Cancer Inst. 2017;109
Knudsen AB, Zauber AG, Rutter CM, Naber SK, Doria-Rose VP, Pabiniak C, et al. Estimation of benefits, burden, and harms of colorectal Cancer screening strategies: modeling study for the US preventive services task force. JAMA. 2016;315:2595–609.
•• Wolf AMD, Fontham ETH, Church TR et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin 2018; DOI https://doi.org/10.3322/caac.21457. Guideline update that recommends to start CRC screening at 45 years old, instead of 50, for average-risk adults.
Murphy CC, Lund JL, Sandler RS. Young-onset colorectal cancer: earlier diagnoses or increasing disease burden? Gastroenterology. 2017;152:1809–12. e1803
Hubbard JM, Grothey A. Adolescent and young adult colorectal cancer. J Natl Compr Cancer Netw. 2013;11:1219–25.
Bleyer A, Barr R, Hayes-Lattin B, et al. The distinctive biology of cancer in adolescents and young adults. Nat Rev Cancer. 2008;8:288–98.
Chang CC, Lin PC, Lin CC, Lan YT, Lin HH, Lin CH, et al. Molecular and clinicopathological differences by age at the diagnosis of colorectal cancer. Int J Mol Sci. 2017;18
Weinberg BA, Poorman K, Arguello D, et al. Impact of patient age on molecular alterations in left-sided colorectal tumors. J Clin Oncol. 2017;35:3592.
Network NCC. Genetic/familial high-risk assessment: colorectal. Version 3.2017.
Magnani G, Furlan D, Sahnane N, et al. Molecular features and methylation status in early onset (</=40 years) colorectal cancer: a population based. Case-Control Study Gastroenterol Res Pract. 2015;2015:132190.
Jones JC, Renfro LA, Al-Shamsi HO, et al. (Non-V600) BRAF mutations define a clinically distinct molecular subtype of metastatic colorectal cancer. J Clin Oncol. 2017;35:2624–30.
Puccini A, Lenz HJ, Marshall JL, et al. Impact of patient age on molecular alterations of the left-sided colorectal tumors. Oncologist. 2018. https://doi.org/10.1634/theoncologist.2018-0117.
NCCN. Colon cancer. 2018; Version 1.2018.
Shi Q, Sobrero AF, Shields AF, et al. Prospective pooled analysis of six phase III trials investigating duration of adjuvant (adjuv) oxaliplatin-based therapy (3 vs 6 months) for patients (pts) with stage III colon cancer (CC): the IDEA (International Duration Evaluation of Adjuvant chemotherapy) collaboration. J Clin Oncol. 2017;35:LBA1.
• Grothey A, Sobrero AF, Shields AF, et al. Duration of adjuvant chemotherapy for stage III colon cancer. N Engl J Med. 2018;378:1177–88. The largest trial in adjuvant setting ever conducted that has led to a paradigm shift in the treatment of stage III CRC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Personalized Medicine in Colorectal Cancer
Rights and permissions
About this article
Cite this article
Sonbol, M.B., Bekaii-Saab, T.S., Puccini, A. et al. Young Patients with Colorectal Cancer: Risk, Screening, and Treatment. Curr Colorectal Cancer Rep 14, 159–165 (2018). https://doi.org/10.1007/s11888-018-0412-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11888-018-0412-y